How Reality Therapy and Choice Theory Help You Achieve Success in Nursing
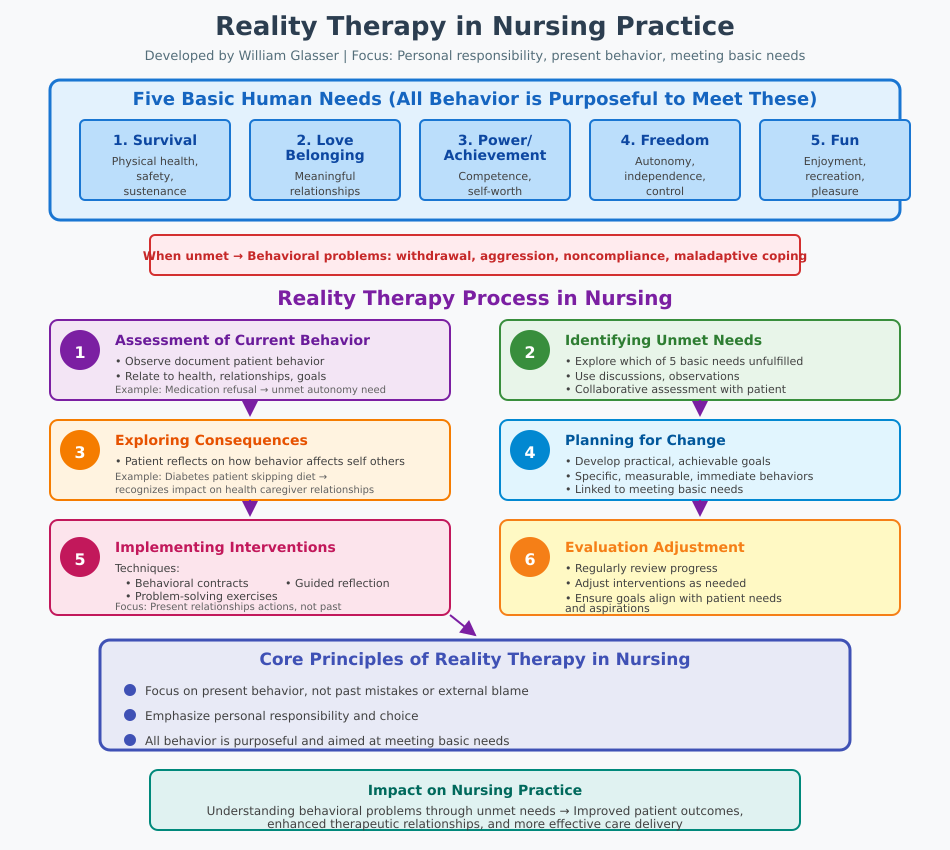
Reality therapy is a structured form of therapy developed by William Glasser that emphasizes personal responsibility, present-focused behavior, and the capacity to make better choices to achieve meaningful goals. Grounded in choice theory, this approach posits that human behavior is purposeful and motivated by the need to fulfill essential psychological needs, such as survival, love and belonging, power, freedom, and fun. When these basic needs are unmet, individuals may exhibit behavioral challenges or struggle with maintaining healthy present relationships. Reality therapy provides a framework for understanding current behavior, addressing unmet needs, and guiding interventions that encourage individuals to take control of their lives and move closer to their goals.
Unlike therapeutic approaches that focus heavily on past experiences or external circumstances, reality therapy focuses on the present and emphasizes actionable strategies for change. By assessing essential needs and applying reality therapy techniques, practitioners can help individuals reconnect with meaningful relationships, set achievable goals, and engage in problem-solving to modify behaviors that hinder wellbeing. Therapists use this method to create interventions that are practical, empowering, and adaptable to diverse clinical contexts, ranging from psychiatric care to family counseling and general nursing practice.
The reality therapy process involves guiding individuals to examine their behaviors in light of their needs and goals, evaluating how their actions impact themselves and others, and identifying more effective strategies to meet unmet needs. This approach encourages individuals to recognize the connection between behavior and satisfaction of basic psychological needs, fostering accountability, self-efficacy, and long-term behavioral change. By emphasizing choice of behaviors and focusing on present relationships, reality therapy provides a roadmap for meaningful, measurable improvements in mental health and interpersonal functioning.
In nursing practice, reality therapy and choice theory offer valuable tools for patient-centered care. Nurses can assess patients’ needs, guide them in making better choices, and support them in adopting behaviors that promote health and wellness. Through structured interventions, such as behavioral goal setting, needs assessment, and fostering connections with others, nurses can help patients navigate challenges related to behavioral problems, stress, and unmet psychological needs. Evidence suggests that applying reality therapy principles can improve patient engagement, enhance treatment adherence, and strengthen therapeutic relationships.
This article provides a comprehensive exploration of reality therapy and choice theory, highlighting their application in nursing practice, the principles of reality therapy, William Glasser’s five basic needs, and practical strategies for implementing interventions that facilitate meaningful behavioral change. By understanding the reality therapy process and employing targeted techniques, practitioners can help individuals meet their basic needs, improve their decision-making, and achieve positive outcomes in diverse healthcare settings.
Understanding Reality Therapy in Nursing
What Reality Therapy Is and How It Works in Nursing Practice
Reality therapy is a form of therapy developed by William Glasser that emphasizes personal responsibility, the satisfaction of essential psychological needs, and present-focused behavior. It is grounded in the understanding that all human behavior is purposeful and aimed at meeting basic needs, which include:
- Survival – Physical health, safety, and sustenance.
- Love and belonging – Meaningful connections and relationships.
- Power or achievement – Competence, recognition, and self-worth.
- Freedom – Autonomy, independence, and control over one’s choices.
- Fun – Enjoyment, recreation, and pleasurable experiences.
When these basic needs are not being met, individuals may engage in behavioral problems such as withdrawal, aggression, noncompliance, or maladaptive coping strategies. In nursing, understanding these behaviors is crucial because they directly impact patient outcomes and the effectiveness of care.
The reality therapy process in nursing practice typically follows these steps:
- Assessment of Current Behavior
- Nurses observe and document the patient’s current behavior in relation to their health, relationships, and goals.
- For example, a patient refusing to take medications may be exhibiting behavior driven by unmet needs for autonomy or safety.
- Identifying Unmet Needs
- The nurse explores which of the five basic needs are not being fulfilled.
- This may involve discussions, observations, and collaborative assessment with the patient.
- Exploring the Consequences of Behavior
- Patients are encouraged to reflect on how their behaviors affect themselves and others.
- A patient with diabetes skipping dietary recommendations may recognize how this choice impacts health outcomes and relationships with caregivers.
- Planning for Change
- Nurses guide patients to develop practical, achievable goals that help them meet their basic needs.
- Goals are specific, measurable, and linked to behaviors that can be altered immediately.
- Implementing Interventions
- Reality therapy techniques such as behavioral contracts, problem-solving exercises, and guided reflection are used.
- Nurses focus on present relationships and actions rather than past mistakes or external factors.
- Evaluation and Adjustment
- Progress is regularly reviewed, and interventions are adjusted to ensure behavioral goals remain aligned with patient needs and aspirations.
Practical Example in Nursing:
- A patient in a psychiatric ward exhibits aggressive outbursts due to unmet love and belonging needs.
- The nurse applies reality therapy by:
- Helping the patient identify triggers for aggression.
- Encouraging social engagement with peers and family.
- Setting goals to practice self-regulation techniques during stressful interactions.
- Monitoring progress and celebrating positive behavioral changes.
This approach not only addresses behavioral problems but also empowers patients to take control of their actions and decisions, aligning interventions with their essential needs.
Reality Therapy as a Form of Choice Theory
Reality therapy is also a form of therapy based on choice theory, which emphasizes that individuals are responsible for the choices that shape their behavior. Choice theory and reality therapy are inherently linked, as they both focus on:
- Autonomy and personal responsibility – Patients can control their own actions and make decisions that align with their needs and goals.
- Behavior as a tool to meet needs – All behavior is viewed as an attempt to satisfy unmet needs.
- Focus on present actions rather than past experiences – Change is achieved through actionable strategies in the here-and-now.
Application in Nursing:
- Facilitating Better Choices
- Nurses guide patients to identify maladaptive behaviors and consider better choices that help fulfill five basic needs.
- Example: A patient with chronic pain is encouraged to engage in physical therapy exercises to regain mobility and independence, addressing the power and freedom needs.
- Promoting Accountability and Problem-Solving
- Through structured conversations, patients are supported in taking responsibility for behaviors that hinder goal achievement.
- Example: In a long-term care facility, a resident avoiding social activities may be helped to understand how unmet love and belonging needs contribute to withdrawal and how participation in group events can improve wellbeing.
- Aligning Behavior with Quality World
- The quality world concept refers to an individual’s internal vision of ideal relationships, goals, and experiences. Nurses can help patients assess if their behaviors bring them closer to or further from their quality world, guiding them toward more adaptive actions.
- Empowering Through Choice
- Reality therapy encourages patients to make choices William Glasser’s framework identifies as essential for satisfaction.
- Example: Encouraging a patient struggling with dietary compliance to plan meals that are both enjoyable and healthy supports freedom, fun, and survival needs simultaneously.
By integrating choice theory and reality therapy, nurses provide a framework that transforms behavioral assessment into actionable interventions. This approach is particularly valuable in nursing because it:
- Enhances patient engagement.
- Supports individualized care planning.
- Improves adherence to treatment.
- Encourages sustainable behavioral change.
Core Principles of Reality Therapy and Choice Theory
Reality therapy, grounded in choice theory, emphasizes the relationship between human needs, behavior, and personal choice. Understanding these principles is essential for nurses seeking to implement therapeutic strategies that support patient wellbeing. The core principles of reality therapy revolve around the fulfillment of basic needs, the influence of current behavior on outcomes, and the alignment of actions with an individual’s quality world.
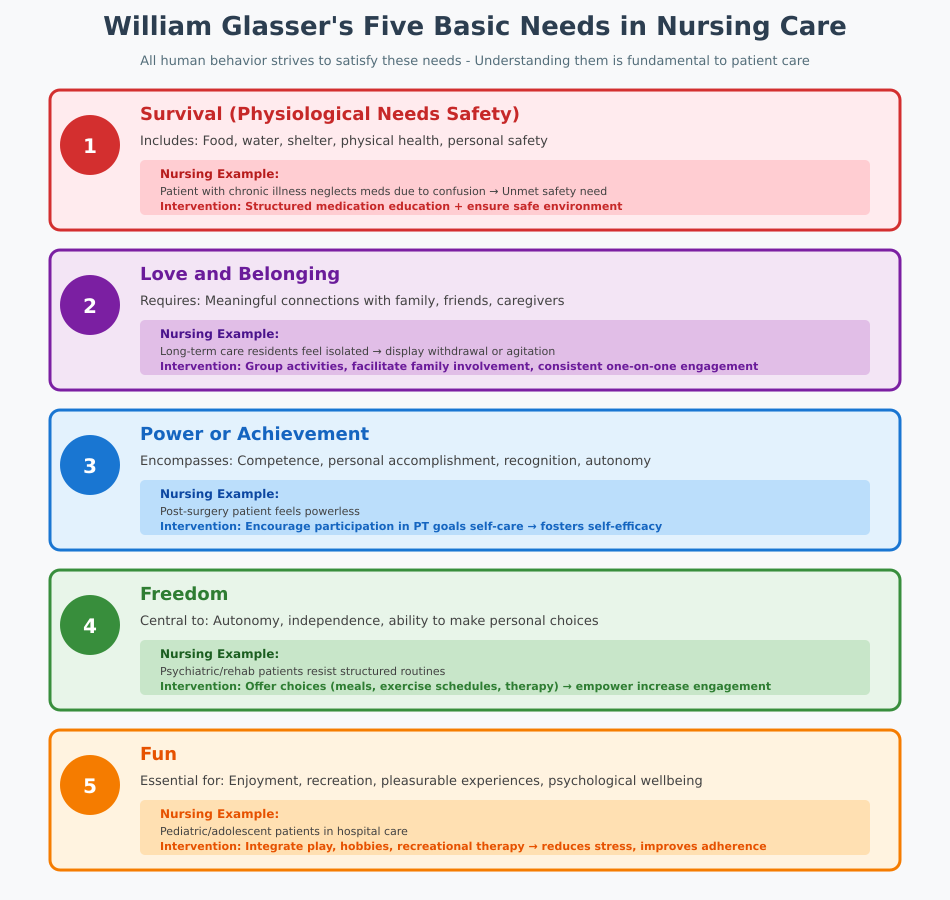
William Glasser’s Five Basic Needs in Nursing Care
William Glasser identified five basic needs that all humans strive to satisfy through their behaviors. In nursing practice, recognizing these needs is fundamental to understanding why patients behave the way they do and designing interventions that are both therapeutic and practical. The five needs include:
- Survival (Physiological Needs and Safety)
- This includes access to food, water, shelter, physical health, and personal safety.
- Example: A patient with chronic illness may neglect medications due to confusion about dosage or lack of understanding, reflecting unmet safety needs. A nurse can intervene by providing structured medication education and ensuring a safe environment, thereby helping the patient meet their basic needs.
- Love and Belonging
- Humans require meaningful connections with others, including family, friends, and caregivers.
- Example: In long-term care settings, residents who feel isolated may display withdrawal or agitation. Nurses can organize group activities, facilitate family involvement, or provide consistent one-on-one engagement to address unmet love and belonging needs.
- Power or Achievement
- This need encompasses competence, personal accomplishment, recognition, and autonomy.
- Example: A patient recovering from surgery may feel powerless. Encouraging participation in physical therapy goals or self-care activities allows them to take control, fostering self-efficacy and satisfaction of the power need.
- Freedom
- Autonomy, independence, and the ability to make personal choices are central to this need.
- Example: In psychiatric or rehabilitation nursing, patients may resist structured routines. By offering choices in daily activities—such as meal selections, exercise schedules, or therapy participation—nurses empower patients to make better choices and increase engagement.
- Fun
- Enjoyment, recreation, and pleasurable experiences are essential for psychological wellbeing.
- Example: For pediatric or adolescent patients in hospital care, integrating play, hobbies, or recreational therapy can fulfill fun needs, reducing stress and improving adherence to treatment plans.
By addressing these five basic needs, nurses can create care plans that influence behavior positively, promote self-regulation, and reduce maladaptive coping strategies. Reality therapy maintains that unmet needs often drive problematic behavior, making it imperative for nurses to conduct thorough assessments of patients’ essential needs during care.
Current Behavior and Unmet Needs: Implications for Care
Current behavior is the most observable indicator of unmet needs. Reality therapy recognizes that behavior is purposeful and aimed at satisfying essential needs. When behaviors are maladaptive—such as noncompliance, aggression, or withdrawal—they signal unmet needs that require intervention.
Strategies for addressing unmet needs in nursing practice include:
- Observation and Documentation
- Nurses should systematically observe behaviors in the context of needs and goals, noting patterns that indicate unmet psychological or physiological needs.
- Example: A patient refusing meals may be struggling with freedom or power needs, desiring more control over dietary choices.
- Engaging Patients in Reflection
- Nurses can use reality therapy techniques to explore the purpose behind behaviors and guide patients toward understanding the connection between actions and need fulfillment.
- Example: A patient expressing anger during wound care may reflect unmet love and belonging needs. The nurse can facilitate discussions to address these feelings while maintaining therapeutic care.
- Collaborative Goal Setting
- Linking behavioral goals to meeting basic needs encourages accountability and active participation in care.
- Example: Encouraging a patient with mobility limitations to participate in physical therapy sessions can satisfy power and freedom needs while improving functional outcomes.
- Practical Interventions at the Bedside
- Incorporating structured routines, behavioral contracts, or skill-building exercises allows patients to engage in behaviors that meet needs constructively.
By aligning interventions with unmet needs, nurses enhance the likelihood of positive behavioral change, strengthen therapeutic relationships, and support the reality therapy process in clinical care.
The Quality World Concept in Clinical Decision-Making
The quality world concept is central to choice theory and reality therapy. It represents an individual’s internal vision of ideal relationships, experiences, and goals—essentially, the world the person wants to live in. Understanding a patient’s quality world helps nurses:
- Guide Behavioral Interventions
- Behaviors are evaluated based on how closely they align with the patient’s quality world.
- Example: A patient who values independence may resist assistance with daily living. By negotiating tasks that allow partial independence, nurses respect the patient’s quality world while ensuring safety.
- Enhance Patient Engagement
- Aligning care plans with patients’ perceived priorities increases motivation and adherence.
- Example: In a rehabilitation unit, allowing patients to select therapy activities that reflect personal interests integrates fun needs and strengthens engagement.
- Support Goal Achievement
- The quality world provides a framework for setting realistic, meaningful goals that meet basic needs.
- Example: For a patient recovering from substance use, nurses can explore goals related to connections with others and power needs, incorporating steps that gradually shift behavior toward healthful routines.
By applying the quality world concept, nurses can bridge the gap between patient aspirations and actionable care, ensuring that interventions are therapeutic, need-driven, and contextually relevant.
Applying Reality Therapy Techniques in Nursing Practice
Applying reality therapy in nursing involves using structured techniques that guide patients to make better choices, address unmet needs, and improve overall wellbeing. Nurses and reality therapists can incorporate these strategies across clinical settings, from acute care to mental health units, ensuring interventions are practical, evidence-based, and patient-centered.
Problem-Solving and Decision-Making Skills for Nurses
One of the foundational aspects of reality therapy and choice theory is helping patients recognize that behavior is a choice and that current behavior can be changed to meet essential needs. Nurses can facilitate problem-solving and decision-making through the following techniques:
- Assessing Needs and Goals
- Begin by identifying which of the five basic needs are unmet and how these influence current behavior.
- Example: A patient refusing to participate in physical therapy may be experiencing unmet power and freedom needs. The nurse can explore the patient’s goals and barriers to participation.
- Encouraging Self-Reflection
- Nurses guide patients to evaluate the consequences of their behavior and consider alternative actions.
- Example: In a mental health setting, a patient expressing anger may reflect on how outbursts affect relationships (love and belonging needs) and treatment progress.
- Goal Setting and Action Planning
- Collaboratively establish achievable, measurable goals linked to needs and wants.
- Example: A patient recovering from surgery may set the goal of completing daily mobility exercises to satisfy power and freedom needs, with progress reviewed each day.
- Behavioral Contracts
- Formalize agreements outlining specific behaviors the patient will undertake to meet their essential needs.
- Example: In psychiatric care, a behavioral contract can guide adolescents to participate in group therapy while practicing coping strategies, helping them make better choices and rebuild trust in present relationships.
- Problem-Solving Exercises
- Facilitate structured exercises where patients identify challenges, explore solutions, and evaluate outcomes.
- Example: A patient struggling with chronic illness may list obstacles to medication adherence and brainstorm feasible strategies, such as using pill organizers or reminders.
Through these steps, nurses integrate the reality therapy process, ensuring that patients develop decision-making skills, recognize personal responsibility, and understand the link between behavior and need fulfillment.
Building Relationships and Connections at the Bedside
Reality therapy emphasizes the importance of present relationships in promoting behavioral change. In nursing, fostering trust and engagement is critical to therapeutic success:
- Establishing Trust
- Patients are more likely to engage in counseling and psychotherapy techniques when they feel safe and understood.
- Example: A nurse consistently listening to patient concerns without judgment builds rapport, creating a foundation for collaborative problem-solving.
- Collaborative Care
- Nurses involve patients in decisions about care, reinforcing autonomy (freedom needs) and encouraging take control behaviors.
- Example: Allowing a patient to choose the sequence of wound care procedures fosters engagement and ownership of care.
- Supporting Emotional Needs
- Focus on love and belonging needs by maintaining consistent interactions, validating feelings, and encouraging positive social connections.
- Example: In long-term care, facilitating group activities or family visits strengthens connections with others, reduces behavioral withdrawal, and enhances adherence to care plans.
- Modeling Positive Behaviors
- Nurses act as therapists or role models, demonstrating constructive coping, respectful communication, and problem-solving strategies.
- Example: When managing conflict between patients, a nurse demonstrates negotiation and empathy, encouraging patients to emulate these behaviors to meet essential needs.
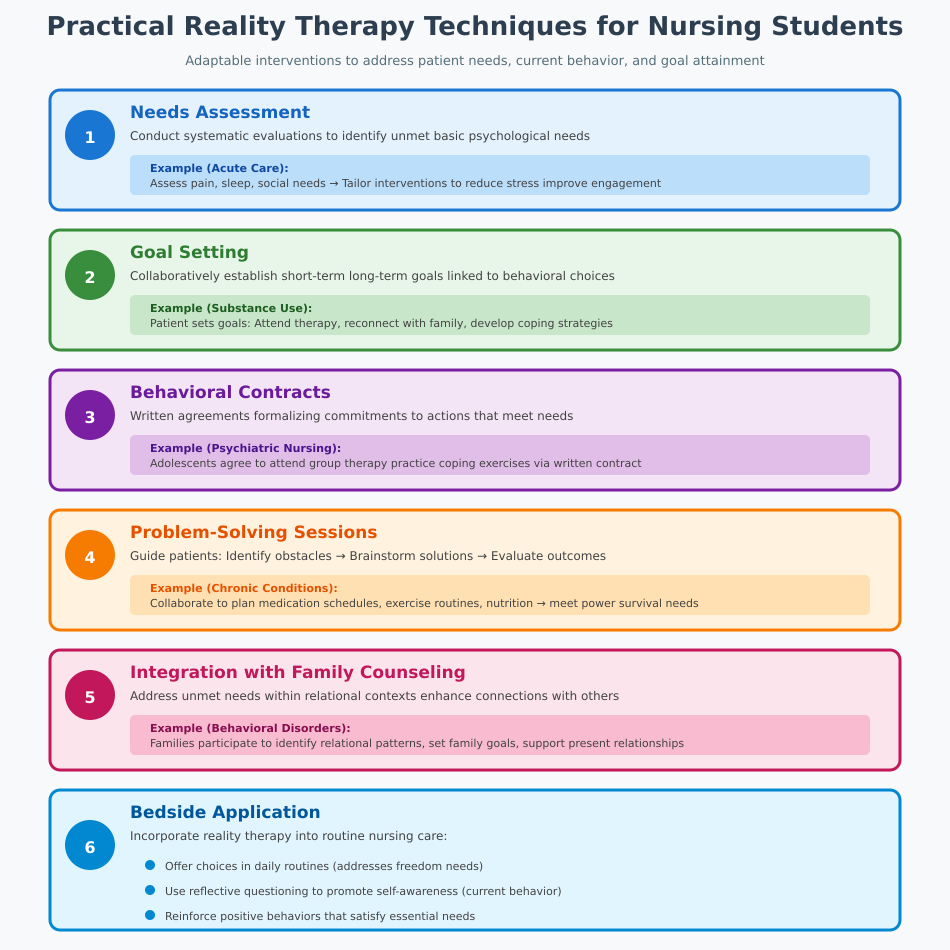
Practical Therapy Techniques for Nursing Students
Reality therapy techniques can be adapted to a variety of clinical scenarios to address patient needs, current behavior, and goal attainment. Key interventions include:
- Needs Assessment:
- Conduct systematic evaluations to identify unmet basic psychological needs.
- Example: In acute care, assess pain, sleep, and social needs to tailor interventions that reduce stress and improve engagement.
- Goal Setting:
- Collaboratively establish short-term and long-term goals linked to behavioral choices and satisfaction of essential needs.
- Example: A patient with substance use issues sets goals for attending therapy sessions, reconnecting with supportive family, and developing coping strategies.
- Behavioral Contracts:
- Use written agreements to formalize commitments to actions that meet needs and resolve behavioral challenges.
- Example: In psychiatric nursing, adolescents may agree to attend group therapy sessions and practice coping exercises as part of a contract guided by reality therapy techniques.
- Problem-Solving Sessions:
- Guide patients in identifying obstacles, brainstorming solutions, and evaluating outcomes.
- Example: Patients with chronic conditions collaborate with nurses to plan medication schedules, exercise routines, and nutrition strategies that meet power and survival needs.
- Integration with Family Counseling:
- Reality therapy can be extended to family counseling, addressing unmet needs within relational contexts and enhancing connections with others.
- Example: Families of adolescents with behavioral disorders participate in sessions to identify relational patterns, set family goals, and support present relationships.
- Bedside Application:
- Nurses can incorporate reality therapy into routine care:
- Offer choices in daily routines (freedom needs)
- Use reflective questioning to promote self-awareness (current behavior)
- Reinforce positive behaviors that satisfy essential needs
- Nurses can incorporate reality therapy into routine care:
By implementing these practical therapy techniques, nurses actively engage patients in making better choices, enhance adherence to care plans, and support overall behavioral and psychological wellbeing. The approach is adaptable to diverse settings, including acute care, mental health, long-term care, and family counseling, demonstrating the effectiveness of reality therapy in improving outcomes.
Practical Example Across Settings:
- Acute Care: A post-surgical patient struggling with mobility and compliance is guided to set daily physical therapy goals, reinforcing power and freedom needs.
- Mental Health: An adolescent displaying aggression is taught coping strategies, encouraged to reflect on current behavior, and participates in group sessions to meet love and belonging needs.
- Family Counseling: A family of a patient with chronic illness learns collaborative problem-solving strategies to improve communication and foster connections with others.
Evidence and Effectiveness of Reality Therapy in Nursing
The application of reality therapy in clinical settings has been explored in diverse studies, offering insight into how this form of therapy influences behavior, psychological wellbeing, and health outcomes. Grounded in choice theory and reality therapy principles, research examines both the effectiveness of reality therapy itself and how it compares to other psychotherapeutic approaches such as cognitive‑behavioral therapy.
Importantly, although the research base is smaller and less robust than that supporting some other modalities, there is evidence that reality therapy can positively impact patient outcomes in specific clinical contexts. This section reviews empirical findings and evaluates which patient groups have demonstrated benefit when reality therapy is applied in nursing and related care settings.
Research on Reality Therapy in Clinical Settings
Although comprehensive large‑scale randomized controlled trials (RCTs) are limited, several controlled studies and intervention trials point to positive effects of reality therapy interventions on patient behavior, mental health, and treatment adherence.
One randomized controlled trial evaluating a reality therapy training program in patients with Type 2 diabetes mellitus found that structured group reality therapy significantly improved treatment adherence and health indicators compared with control conditions. The intervention—rooted in reality therapy and choice theory—encouraged participants to explore how current behavior aligned with their needs and goals, reinforcing autonomous decision‑making around lifestyle and medication behaviors. The findings suggest that when patients are supported in recognizing and adjusting their behavioral choices, adherence and clinical indicators such as glucose control can improve.
In another controlled study focusing on psychosocial outcomes, reality therapy yielded significant improvements in general health, reduced anxiety, and enhanced interpersonal functioning among groups receiving the intervention. While this research was conducted outside strict nursing settings, it demonstrates broader clinical utility for behavior‑oriented outcomes consistent with the goals of patient‑centered care.
A quasi‑experimental comparison study in mothers of children with autism revealed that both cognitive‑behavioral therapy and reality therapy significantly reduced anxiety, with reality therapy showing an even greater impact than CBT. This suggests that, at least in some behavioral health contexts, reality‑based interventions may be as effective—or more effective—than traditional psychotherapeutic approaches for reducing specific psychological symptoms such as anxiety.
In addition, individual case reports and smaller studies have shown promising results using reality therapy techniques to reduce maladaptive behaviors related to post‑traumatic stress and obsessive beliefs, improve psychological flexibility, and enhance mental wellbeing across a range of populations.
Key Takeaways from Clinical Research:
- Reality therapy interventions can improve treatment adherence and some health outcomes in chronic disease management.
- Reality therapy may reduce anxiety and psychological distress in caregivers and family members.
- Group reality therapy has demonstrated benefits on measures of general health and interpersonal functioning.
- Comparisons with cognitive‑behavioral therapy show potential parity or even superior effects on specific outcomes, although broader evidence is limited.
Nevertheless, systematic reviews note that the overall evidence base for reality therapy is somewhat limited compared with more widely studied modalities, and long‑term follow‑ups are scarce.
Patient Populations That Benefit Most
A range of patient groups has shown responsiveness to interventions grounded in reality therapy and choice theory, particularly where the focus is on immediate behavior change, meeting essential needs, and enhancing engagement with care processes.
1. Patients with Chronic Illnesses:
Reality therapy has been used in patients with chronic conditions such as diabetes, where behavioral choices profoundly affect clinical outcomes. By linking behavior to physiological and psychological needs, nurses can help patients make sustainable changes in diet, medication adherence, and self‑management routines.
2. Individuals Experiencing Anxiety and Psychological Stress:
Research in mothers of children with autism showed reductions in anxiety when reality therapy was applied, highlighting its utility in populations dealing with chronic care stress.
Similarly, studies on parents of children with cancer indicate improvements in psychological distress and resilience after reality therapy interventions, likely through enhanced problem‑solving and support in meeting emotional needs.
3. Behavioral and Interpersonal Difficulties:
Reality therapy’s emphasis on present relationships and choice has been effective in settings involving social or behavioral challenges. Group interventions have improved general health, interpersonal relationships, and social functioning in settings where participants struggled with adaptive behaviors.
4. Family Counseling and Support Networks:
Because reality therapy integrates well with choice theory and family dynamics, it has been used in family counseling contexts. Here, the focus on identifying unmet needs, strengthening present relationships, and collaborative problem‑solving helps families navigate complex care situations and enhance collective support structures.
5. Younger Populations with Behavior and Decision‑Making Challenges:
While not strictly clinical nursing populations, research with students and adolescents shows that reality therapy enhances awareness of personal control over behavior, boosts responsibility, and reduces disciplinary incidents.
Comparisons with Cognitive‑Behavioral Therapy
Comparative studies suggest that reality therapy may be as effective as—or in some cases more effective than—cognitive‑behavioral therapy in reducing specific symptoms such as anxiety. These findings underscore the importance of considering patient needs, context, and therapeutic goals when selecting an intervention modality.
However, systematic reviews of psychotherapy generally indicate that CBT has a stronger and more extensive evidence base across anxiety, depression, and some behavioral disorders, reflecting differences in research volume rather than therapeutic superiority per se.
Learning and Implementing Reality Therapy for Nurses
Integrating reality therapy into nursing practice begins with formal and informal learning of theoretical foundations and practical techniques. This section discusses how nurses can learn reality therapy techniques, including structured training pathways such as those offered by the Glasser Institute, and outlines how to apply reality therapy at the bedside to support patient behavior change, needs assessment, and therapeutic relationships.
How Nurses Can Learn Reality Therapy Techniques
Nurses interested in developing proficiency in reality therapy and choice theory have several training options ranging from introductory workshops to advanced certification programs. These training pathways provide a structured approach to understanding how choice theory explains human behavior and how reality therapy focuses on present behavior, problem‑solving, and need fulfillment.
1. Introductory Training Programs
- Basic Intensive Workshops: Many organizations affiliated with William Glasser International (WGI) offer short courses (often 3–4 days) that introduce participants to the principles and practice of reality therapy and choice theory. These workshops cover key concepts such as the five basic needs, the quality world, and the reality therapy process, and include role‑plays, group discussions, and skill demonstrations. Example: A nurse attends a 4‑day Basic Intensive Workshop where they learn how to evaluate current behavior, distinguish internal from external control, and practice applying reality therapy questions with simulated patient scenarios.
- Short Courses and Introductory Sessions: Some institutes provide one‑day or weekend courses focused on foundations of choice theory and reality therapy that are more accessible for busy health professionals.
These introductory programs equip nurses with foundational knowledge and basic application skills, supporting them in bringing reality therapy techniques into everyday interactions.
2. Certification and Advanced Training
For nurses who wish to specialize or pursue formal credentials, the William Glasser International Certification pathway offers a multi‑stage training program lasting roughly 18 months.
Certification typically includes:
- Basic Intensive Training – Foundational concepts and practice.
- Basic Practicum – Supervised practice and application of techniques.
- Advanced Intensive Training – Deeper exploration of therapeutic skills.
- Advanced Practicum – Further supervised experience.
- Certification Week – Demonstration of competence and knowledge.
This comprehensive track helps nurses and other professionals develop a therapeutic skill set that supports autonomy, relationship building, and effective use of choice theory in clinical care. Mentorship from certified faculty and practicum supervisors during this process reinforces skills and provides feedback on reality therapy process implementation.
3. Professional Development and Peer Learning
- Nurses can also engage in ongoing professional development through seminars, webinars, journal clubs, and local workshops on reality therapy and choice theory psychology offered by institutes like the Glasser Institute.
- Peer learning communities and interdisciplinary forums allow nurses to share case examples and discuss how reality therapy focuses on present behavior and needs in clinical scenarios.
By pursuing structured education and mentorship, nurses deepen their understanding of how human behavior connects with psychological needs and how interventions can promote better choices in patient care.
Applying Reality Therapy at the Bedside
Learning the theory is essential, but the real impact of reality therapy in nursing practice is realized when nurses apply these principles and techniques at the bedside. Implementation involves integrating problem‑solving strategies, needs assessment, and relationship‑focused care into daily patient interactions.
1. Conducting Needs Assessment and Behavioral Evaluation
Nurses begin by assessing the five basic needs of patients to understand drivers of current behavior: survival, love and belonging, power or achievement, freedom, and fun. Identifying unmet needs guides intervention planning.
Example: A nurse notices that a patient with repeated noncompliance around treatment may be seeking control or autonomy. Through discussion, the nurse explores how missed treatments relate to unmet psychological needs and collaboratively develops strategies that align care with patient priorities.
2. Promoting Problem‑Solving and Decision‑Making
Using the reality therapy process, nurses facilitate structured dialogue that helps patients articulate what they want, evaluate their behavior, and plan targeted steps toward achievable goals. This aligns with choice theory and reality therapy by reinforcing personal responsibility and guiding patients to make better choices about their health.
A practical framework often used resembles WDEP (Wants, Doing, Evaluation, Planning), which helps patients clarify:
- What they want.
- What they are currently doing.
- Whether current behaviors are effective.
- What new actions could help satisfy needs.
Example: A patient struggling with smoking cessation may outline their goals, assess how current smoking behavior relates to stress and social needs, and develop a practical quitting plan with rewards and support.
3. Strengthening Therapeutic Relationships
Reality therapy recognizes that strong, trust‑based relationships are essential to effective care. Nurses build rapport by listening without judgement, focusing on present concerns, and engaging patients collaboratively rather than prescribing solutions unilaterally. Fostering a connection helps patients feel understood and supported in adaptive decision‑making.
Example: In a medical‑surgical unit, a nurse builds trust with a patient in pain by acknowledging discomfort, exploring how pain influences daily choices, and co‑creating pain‑management strategies that respect patient autonomy and goals.
4. Integrating Behavioral Contracts and Follow‑Up
Reality therapy techniques include designing behavioral contracts, where nurses and patients agree on specific actions the patient will take to advance toward goals. These contracts are not punitive but structured agreements emphasizing accountability, clarity, and measurable progress.
Example: A patient with diabetes agrees to a daily glucose monitoring schedule, diet plan, and activity goals with regular check‑ins to evaluate progress and adjust the plan as needed.
Conclusion
Reality therapy and choice theory offer a structured, evidence-based approach to nursing practice that emphasizes understanding current behavior, identifying unmet needs, and supporting patients in making better choices to meet their essential needs. By recognizing the importance of present relationships, nurses and reality therapists can build trust, foster engagement, and guide patients toward healthier decision-making and goal achievement.
The principles of reality therapy, including the focus on the five basic needs—survival, love and belonging, power, freedom, and fun—serve as a framework for assessing behavior, designing interventions, and evaluating outcomes. Nurses who integrate reality therapy techniques into bedside care can support patient autonomy, strengthen therapeutic connections, and enhance problem-solving skills, all while promoting psychological needs and overall wellbeing.
Research demonstrates the effectiveness of reality therapy across diverse populations, including patients with chronic illnesses, behavioral challenges, and families requiring family counseling. Studies indicate that reality therapy can complement or, in some contexts, offer outcomes comparable to cognitive-behavioral therapy, particularly in addressing behavioral and relational concerns.
Learning and applying reality therapy through formal programs, mentorship, and practical application allows nurses to implement therapeutic interventions that are both patient-centered and goal-oriented. Ultimately, the integration of reality therapy and choice theory in nursing practice not only enhances clinical decision-making and patient outcomes but also empowers patients to take control of their behaviors, reconnect with their quality world, and move closer to achieving their personal health and life goals.
By embracing this approach, nurses can transform routine care interactions into opportunities for meaningful behavioral change, relationship building, and holistic patient support—truly helping patients achieve their goals while reinforcing professional, compassionate, and effective nursing practice.
Frequently Asked Questions
What is reality therapy and choice theory?
Reality therapy is a form of therapy developed by William Glasser that focuses on helping individuals take control of their current behavior to meet essential needs. It emphasizes personal responsibility, problem-solving, and improving present relationships. Choice theory underpins reality therapy, explaining that all human behavior is purposeful and aimed at fulfilling one or more of the five basic needs—survival, love and belonging, power, freedom, and fun. Together, reality therapy and choice theory guide individuals to understand their behavior, make better choices, and work toward meaningful goals.
What are the goals when applying a choice reality therapy approach?
The goals of applying a reality therapy and choice theory approach are to:
- Help individuals recognize how current behavior affects their ability to meet basic psychological needs.
- Encourage take control actions, enabling patients to make better choices that align with their essential needs.
- Strengthen present relationships and improve social and interpersonal functioning.
- Support problem-solving and decision-making to achieve personal and health-related goals.
Which is a goal of reality choice therapists as they assess a client’s total behavior?
A key goal of reality choice therapists is to evaluate a client’s total behavior—including thoughts, actions, feelings, and physiological responses—to identify areas where unmet needs may be driving maladaptive behaviors and to guide the client in making choices William Glasser’s model would consider constructive for fulfilling those needs.
What are the benefits of reality therapy?
The benefits of reality therapy include:
- Improved behavior through goal-directed choices and problem-solving.
- Enhanced psychological wellbeing by addressing unmet needs and strengthening present relationships.
- Increased patient engagement and participation in care by fostering autonomy and responsibility.
- Practical applicability across settings such as acute care, mental health, and family counseling, making it a versatile therapy process for nurses and other healthcare professionals.
- Supports long-term habit and behavior change by focusing on actionable strategies rather than dwelling on past issues, enhancing the effectiveness of reality therapy in clinical practice.
