LVN vs RN: What’s the Real Difference Between an LVN, LPN, and Registered Nurse?
Nursing roles vary widely in scope, responsibilities, and educational pathways, shaping the day-to-day experiences of those providing patient care. Among these roles, licensed vocational nurses (LVNs) and registered nurses (RNs) represent two critical positions within the healthcare system, each contributing uniquely to patient outcomes and clinical workflows. While both LVNs and RNs share a commitment to delivering safe, effective nursing care, differences in training, scope of practice, and career opportunities distinguish these professions in meaningful ways.
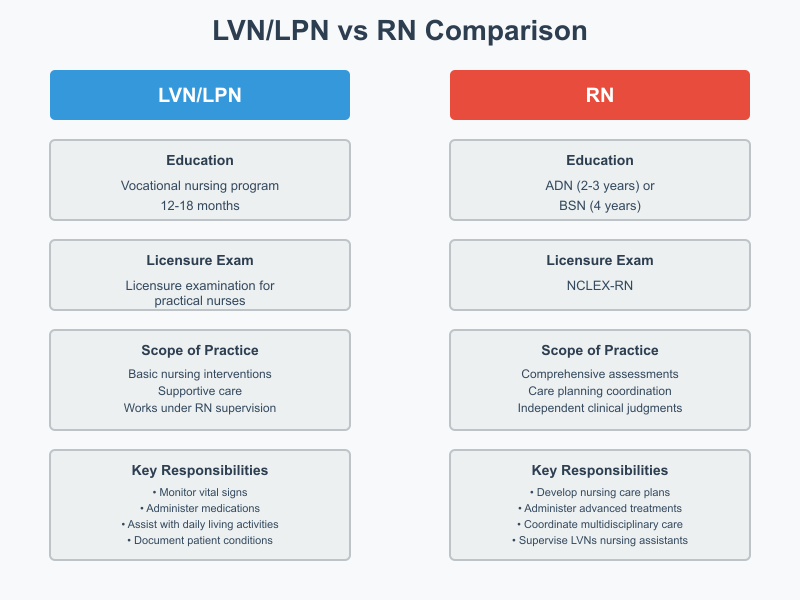
Understanding the distinctions between LVNs, LPNs, and RNs is essential for nursing students making informed decisions about their education and career trajectory. The choice between pursuing a vocational nursing program or an RN-focused pathway, such as an associate degree in nursing (ADN) or a bachelor of science in nursing (BSN), carries implications for clinical responsibilities, opportunities for specialization, and long-term advancement in the nursing field. Moreover, licensing requirements—including the NCLEX-RN for registered nurses and the licensure examination for practical nurses—further delineate the professional boundaries and competencies expected in practice.
This article provides a comprehensive overview of LVN and RN roles, exploring educational pathways, clinical duties, scope of practice, workplace settings, and career advancement opportunities. It examines the factors that nursing students should consider when choosing a nursing program, highlights the differences in patient care responsibilities, and outlines potential career paths for both practical and registered nurses. By understanding these distinctions, aspiring nurses can make evidence-based decisions about their training, clinical focus, and professional development, ensuring alignment with personal career goals and the evolving needs of the healthcare system.
What is an LVN / LPN and how does vocational nursing differ from registered nurse roles?
A licensed vocational nurse (LVN), also known as a licensed practical nurse (LPN) in some states, is a trained healthcare professional who provides essential patient care under the supervision of a registered nurse (RN) or physician. Vocational nurses work across diverse healthcare settings, performing tasks that are foundational to the delivery of safe and effective care, such as monitoring vital signs, administering medications, assisting with hygiene, and documenting patient conditions. Unlike registered nurses, LVNs have a more focused scope of practice, which emphasizes basic nursing interventions and supportive care rather than complex clinical decision-making or care planning.
The primary distinction between vocational nursing and registered nurse roles lies in education, licensure, and responsibility. RNs are trained to conduct comprehensive patient assessments, develop and implement nursing care plans, administer advanced treatments, and coordinate multidisciplinary care. They often hold a bachelor of science in nursing (BSN) or an associate degree in nursing (ADN) and must pass the National Council Licensure Examination (NCLEX-RN) to practice. In contrast, LVNs complete a vocational nursing program, which is shorter in duration, more focused on hands-on skills, and culminates in the licensure examination for practical nurses. While LVNs provide direct nursing care, they do not generally have the authority to perform comprehensive assessments or make independent clinical judgments that fall within the broader scope of practice of RNs.
What does a licensed vocational nurse (LVN) do in patient care?
Licensed vocational nurses are integral to the day-to-day functioning of healthcare settings. Their nursing skills include administering medications, observing patients for changes in condition, assisting with mobility and daily living activities, collecting samples for laboratory tests, and providing emotional support to patients and families. In long-term care settings like nursing homes, LVNs often serve as the primary point of contact for residents, ensuring continuity of basic nursing care and coordinating with registered nurses for more complex interventions. In hospitals or outpatient clinics, practical nurses may support clinical nurses in monitoring patient status, performing wound care, or preparing patients for procedures.
For example, an LVN in a surgical unit may monitor post-operative patients for signs of infection, administer prescribed medications, and report changes to the supervising RN. This role allows vocational nurses to gain hands-on experience, develop critical observation skills, and contribute directly to patient care, while staying within the legal and professional boundaries defined by the nurse practice act in their state.
How does vocational nursing training and LVN program length compare to a nursing program for RNs?
Vocational nursing programs are typically designed to be completed in 12 to 18 months, depending on the institution and state requirements. These programs focus on basic nursing care, pharmacology, anatomy, physiology, and practical skills through supervised clinical rotations. Upon completion, students are eligible to become a licensed vocational nurse by passing the licensure examination for practical nurses.
In comparison, RN programs are longer and more academically rigorous. An associate degree in nursing (ADN) usually takes about 2 to 3 years, whereas a bachelor of science in nursing (BSN) typically requires 4 years of study. These programs provide in-depth education in areas such as advanced nursing care plans, leadership roles, nursing education, community health, research, and evidence-based practice. Graduates must pass the NCLEX-RN to become a registered nurse and are prepared for a broader scope of practice, including care coordination, patient education, and supervisory responsibilities over licensed vocational nurses and nursing assistants.
Where do practical nurses and lvns typically work — nursing homes, clinics, or hospitals?
LVNs and practical nurses are employed across a variety of healthcare settings, each offering unique experiences in nursing care. Common workplaces include:
- Nursing homes and long-term care facilities: LVNs provide daily care, monitor chronic conditions, administer medications, and support residents’ basic nursing care needs.
- Clinics and outpatient facilities: Here, LVNs assist with patient intake, perform basic assessments, administer immunizations, and educate patients on routine care management.
- Hospitals: LVNs often work in medical-surgical units, rehabilitation units, or specialty departments under the supervision of an RN. They may perform wound care, administer IV medications (where permitted), and collaborate in patient monitoring.
The choice of workplace can influence both career goals and skill development. For example, LVNs in hospitals may have greater exposure to complex medical conditions and advanced procedures, preparing them for potential advancement to RN roles through bridge programs like LPN to RN pathways.
What is an RN and how does becoming a registered nurse compare to become an LVN?
A registered nurse (RN) is a licensed healthcare professional who provides comprehensive nursing care, including patient assessments, care planning, and implementation of advanced clinical interventions. Unlike licensed vocational nurses (LVNs), who focus primarily on basic nursing care and hands-on patient support, RNs operate within a broader scope of practice, allowing them to coordinate complex treatments, administer specialized medications, and supervise other nursing staff, including LVNs and nursing assistants.
Becoming a registered nurse typically requires more extensive education and training than pursuing a vocational nursing program. While LVNs complete a program ranging from 12 to 18 months with a focus on bedside skills, RNs can enter the profession through either an associate degree in nursing (ADN) or a bachelor of science in nursing (BSN). Both educational pathways prepare students to pass the National Council Licensure Examination (NCLEX-RN), but a BSN program provides additional coursework in leadership, public health, research, and evidence-based practice, which can open doors to advanced practice nursing roles, including clinical nurse specialists, nurse practitioners, and nurse anesthetists.
What education is required to become an RN — ADN vs bachelor of science in nursing (BSN)?
- Associate Degree in Nursing (ADN):
An ADN program typically takes 2 to 3 years to complete and is offered at community colleges or vocational schools. It focuses on foundational nursing education, clinical rotations, and preparation for the NCLEX-RN. Graduates of ADN programs are qualified to become registered nurses and provide direct patient care in hospitals, clinics, and long-term care settings. - Bachelor of Science in Nursing (BSN):
A BSN program usually requires 4 years of study and includes advanced courses in leadership, healthcare policy, research, and community health. A BSN degree enhances career opportunities and is often preferred for roles in management, specialized care units, and advanced practice nursing. Many hospitals and healthcare organizations increasingly require or prefer RNs with a BSN, citing improved patient outcomes and readiness for leadership positions.
How does the NCLEX-RN licensure examination differ from the licensure examination for practical nurses?
The NCLEX-RN assesses the knowledge, skills, and abilities essential for safe and effective nursing care at the registered nurse level. It evaluates critical thinking, clinical judgment, and the ability to make independent decisions in complex healthcare scenarios. In contrast, the licensure examination for practical nurses is designed to test competencies in basic nursing care, medication administration, and patient observation. While both exams are regulated by the board of nursing, the NCLEX-RN reflects the broader responsibilities and scope of practice expected of registered nurses, compared to the more task-oriented focus of the practical nurse exam.
What are the steps to become a registered nurse and move from lvn to rn?
For LVNs aspiring to become RNs, the path involves bridging from vocational training to a degree program. Key steps include:
- Completing an RN program: Many LVNs enroll in an LPN/LVN to RN bridge program, which can be either an ADN or BSN pathway. These programs recognize prior nursing education and clinical experience, allowing LVNs to complete the RN curriculum more efficiently.
- Passing the NCLEX-RN: After graduation, candidates must successfully pass the National Council Licensure Examination to obtain RN licensure.
- Obtaining RN licensure: Once licensed, the nurse can legally practice as a registered nurse, gaining access to a broader scope of practice, higher salary, and expanded career opportunities, including supervisory roles over LVNs and practical nurses.
- Continuing education and specialization: Newly licensed RNs can pursue advanced certifications, such as family nurse practitioner or clinical nurse specialist, further extending professional growth and leadership potential within the nursing field.
For example, an LVN working in a nursing home may choose an RN program to advance to a hospital unit, gain autonomy in patient care, and eventually move into nurse manager roles or specialty practice areas, illustrating the practical benefits of bridging from vocational nursing to a registered nurse career.
How do scope of practice and responsibilities differ between LVNs and RNs?
The scope of practice for licensed vocational nurses (LVNs) and registered nurses (RNs) reflects differences in education, licensure, and clinical responsibilities. LVNs primarily provide basic nursing care, such as monitoring vital signs, assisting with activities of daily living, and administering medications under the supervision of an RN or physician. In contrast, RNs have a broader scope of practice that includes independent patient assessments, development of nursing care plans, complex interventions, care coordination, and supervisory responsibilities over practical and licensed vocational nurses.
These distinctions are codified by the nurse practice act in each state, which legally defines the limits of practice for vocational nurses and registered nurses. Understanding these boundaries is essential for ensuring safe patient care and compliance with professional regulations.
What clinical skills and broader scope of practice do rns have compared to lvns?
Registered nurses possess a wider array of nursing skills than LVNs, enabling them to manage more complex patient situations. Examples include:
- Advanced assessments: RNs can perform comprehensive physical and psychosocial evaluations, identify subtle changes in patient condition, and initiate interventions.
- Clinical decision-making: RNs analyze data, interpret lab results, and make independent judgments regarding patient care priorities.
- Care planning: RNs develop, implement, and evaluate nursing care plans tailored to patient needs.
- Specialized procedures: Depending on the clinical setting, RNs may insert intravenous lines, administer blood products, and operate advanced medical equipment.
- Leadership roles: RNs often supervise LVNs and nursing assistants, delegate tasks appropriately, and oversee workflow to ensure patient safety.
For example, an RN in a medical-surgical unit may assess a post-operative patient, adjust pain management protocols, delegate medication administration to an LVN, and update the care plan based on patient progress. This demonstrates the broader scope of practice that RNs hold compared to LVNs, who focus on basic nursing care tasks within defined limits.
Which tasks are typically limited to licensed practical nurses versus registered nurses?
LVNs are generally restricted to routine nursing tasks, including:
- Administering oral, topical, and certain injectable medications (depending on state regulations)
- Assisting with activities of daily living such as bathing, dressing, and feeding patients
- Recording vital signs and patient observations
- Reporting changes in patient condition to supervising RNs or physicians
In contrast, RNs are authorized to perform higher-level interventions, including:
- Conducting comprehensive patient assessments and developing individualized nursing care plans
- Administering IV medications, blood products, and other complex therapies
- Delegating tasks to LVNs and nursing assistants while maintaining accountability for patient outcomes
- Implementing evidence-based interventions and evaluating their effectiveness
By delineating these responsibilities, healthcare organizations ensure that LVNs and RNs work collaboratively while staying within their professional boundaries.
How do workplace supervision and delegation work between lvns and rns?
Workplace supervision is a key aspect of vocational nursing practice. LVNs typically work under the supervision of an RN, who provides guidance, reviews patient assessments, and ensures adherence to clinical protocols. Supervision includes both direct oversight in complex care scenarios and general guidance for routine tasks.
Delegation is another critical process in nursing practice. RNs assign specific tasks to LVNs based on their competencies, licensure limitations, and patient needs. For instance, an RN may delegate medication administration, vital sign monitoring, or wound care to an LVN while retaining responsibility for the overall patient outcome. Effective delegation requires clinical judgment, clear communication, and an understanding of each team member’s scope of practice.
In practical terms, a nursing home might employ an RN to oversee the care of residents with complex medical conditions, while LVNs perform hands-on care, monitor patient responses, and report significant changes. This collaborative model maximizes patient safety and ensures that each professional operates within their legally defined scope of practice.

How do salary and career progression compare for LVN/LPN and RN roles?
What does the bureau of labor statistics report about salary differences between lvns and rns?
According to recent data from the Bureau of Labor Statistics (BLS), the median annual wage for licensed practical nurses (LPNs) and licensed vocational nurses (LVNs) was US $62,340 as of May 2024. Meanwhile, registered nurses earned a higher median annual salary of US $93,600 around the same period.
This substantial difference reflects several factors: greater educational requirements for RNs; broader scope of practice; and more complex responsibilities. As such, RNs typically access higher-paying roles, especially in hospitals, specialized units, or advanced care settings.
Beyond base salaries, workplace setting, geographic location, experience, and specialization significantly influence earnings. For instance, RNs with a bachelor‑level nursing degree or those working in high-demand states may earn above the median, while many LVNs work in long‑term care or residential settings where pay may be lower but demand remains steady.
In practical terms, this means that many nursing students choosing between becoming an LVN or RN must consider long-term earning potential: while LVN/LPN offers a quicker route into nursing and stable demand, RN roles generally provide higher earning potential and broader advancement opportunities over time.
How can lvns advance their nursing career to an rn or pursue advanced practice roles?
For LVNs who wish to grow professionally and financially, there are well-established routes to transition into RN roles, often via bridge programs.
Common pathways include:
- Enrolling in an LPN/LVN-to-RN bridge program (either at associate or bachelor’s level) — many institutions offer these specifically to licensed vocational nurses.
- Completing the necessary coursework and clinical hours, then passing the licensure exam for registered nurses. Once licensed as an RN, one gains access to a broader scope, more responsibilities, and higher pay.
- With further education (for example BSN → Master’s or advanced practice), former LVNs can eventually pursue roles such as nurse manager, advanced practice nurse, or specialization in critical care, community health, or other areas.
Because many employers value experience, an LVN transitioning to RN could continue working while studying — often using their real-world patient care experience as a foundation. This makes the transition more practical than starting from scratch.
What are typical career paths and long-term goals for practical and licensed vocational nurses?
Even without immediately transitioning to RN, LVNs/LPNs have viable career paths and opportunities for incremental growth:
- Specialization within vocational nursing: LVNs can specialize in areas like geriatric care, home health, wound care, IV therapy, or long-term care. Over time, experienced LVNs may take on roles such as charge nurse in long-term care facilities or supervisory roles over other practical nurses and nursing assistants.
- Stability in long-term care and home health: Many vocational nurses find steady employment in nursing homes, residential care, home healthcare services, and outpatient clinics. Because of ongoing demand (especially in aging populations), these roles remain in demand.
- Bridge to RN and beyond: For LVNs aiming for growth, the LPN-to-RN bridge is a common long-term strategy. Once becoming an RN, one can aim for advanced practice roles (e.g., nurse practitioner, clinical nurse specialist), leadership roles (unit manager, nurse manager), or specialization in high-demand units (critical care, pediatrics, community health).
- Flexible career trajectory: Some LVNs choose to remain practical nurses but leverage certifications (e.g., IV therapy, gerontology, wound care) to expand responsibilities, take on supervisory or mentoring roles, or work in specialized settings like home care, hospice, or private duty — offering flexibility, work-life balance, and meaningful patient care.
For example, an LVN working in a long-term care facility might over time become a charge nurse supervising other LVNs and nursing assistants; later, she might enroll in a bridge program to become an RN, then aim for a hospital position or specialty unit — dramatically changing her earning potential and career scope.
Which nursing program should I choose — LVN/LPN program, ADN, or BSN?
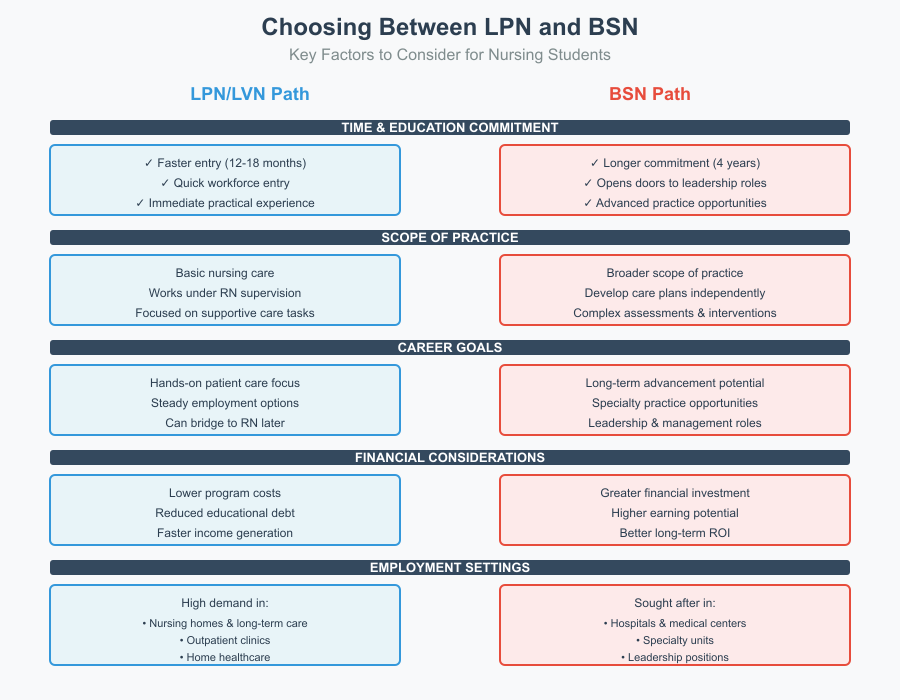
Choosing the right nursing program is a critical decision for aspiring nurses, as it impacts career path, scope of practice, earning potential, and long-term opportunities. Students must weigh the benefits of entering the workforce quickly as a licensed vocational nurse (LVN) or pursuing a more extensive education such as an associate degree in nursing (ADN) or a bachelor of science in nursing (BSN).
How long is an lvn program versus an associate degree in nursing or bachelor of science in nursing?
LVN programs are generally designed to be completed in 12 to 18 months, depending on the institution and state requirements. These programs focus on basic nursing care, patient observation, pharmacology, anatomy, physiology, and clinical rotations in settings such as nursing homes, outpatient clinics, and hospitals. Upon completion, graduates are eligible to become a licensed vocational nurse after passing the licensure examination for practical nurses.
In contrast, ADN programs typically take 2 to 3 years, providing a broader foundation in nursing education, clinical decision-making, and patient care planning. BSN programs require approximately 4 years, combining in-depth study of leadership, research, public health, and evidence-based practice with clinical experiences. BSN-prepared registered nurses often have enhanced opportunities in specialty care, management, and advanced practice roles, including family nurse practitioner or clinical nurse specialist.
What factors should nursing students consider when choosing between quick entry as a licensed practical nurse and pursuing a bsn?
When deciding between a vocational nursing program and a BSN, students should consider several factors:
- Time and Education Commitment: LVN programs allow for faster entry into the workforce, ideal for those seeking immediate employment and practical nursing experience. A BSN requires a longer educational commitment but opens doors to advanced practice nursing, leadership roles, and higher salary.
- Scope of Practice: LVNs provide basic nursing care under the supervision of an RN, whereas BSN-prepared RNs have a broader scope of practice, can develop nursing care plans, and perform complex assessments and interventions.
- Career Goals: Students aiming for long-term advancement, specialty practice, or leadership roles may benefit from pursuing a BSN initially. Those interested in hands-on patient care and steady employment may begin as LVNs, then plan to bridge to RN programs later.
- Financial Considerations: LVN programs are generally less expensive and shorter, which may reduce educational debt. BSN programs require a greater financial investment but offer higher earning potential and access to advanced roles over time.
- Employment Settings: LVNs are in high demand in nursing homes, outpatient clinics, and home healthcare, while BSN-prepared RNs are often sought in hospitals, specialty units, and leadership positions.
Can lvns bridge to rn programs and what are common LVN to RN options?
For students who start with an LVN career but wish to become registered nurses, bridge programs are widely available. These programs recognize prior education and experience, allowing LVNs to complete the RN curriculum more efficiently. Common options include:
- LPN/LVN-to-ADN Programs: These programs allow LVNs to earn an associate degree in nursing, often in 1–2 years, and then take the NCLEX-RN to obtain RN licensure.
- LPN/LVN-to-BSN Programs: Designed for LVNs seeking a bachelor of science in nursing, these programs provide advanced coursework in leadership, research, and community health. Completion typically takes 2–3 years, depending on prior credits and clinical experience.
- Bridge Program Advantages: Students gain clinical experience, continue earning income as LVNs while studying, and benefit from a smoother transition to the broader scope of practice and higher salary associated with RNs.
For example, an LVN working in a long-term care facility might enroll in an LPN-to-BSN program while continuing to provide patient care, gradually expanding skills, knowledge, and career opportunities. After completing the program and passing the NCLEX-RN, the nurse can move into hospital or specialty roles, pursue leadership positions, or continue toward advanced practice nursing.
What certifications, licensure, and continuing education are needed for LVNs and RNs?
What is the licensure examination for practical nurses and requirements for lpn/lvn licensure?
For a nurse to become a licensed vocational nurse (LVN) or licensed practical nurse (LPN), they must complete a state‑approved vocational nursing program and then pass the national licensure exam: the NCLEX-PN (National Council Licensure Examination for Practical Nurses).
Key licensure requirements for LVN/LPN include:
- Completion of an approved vocational nursing program (often 12–18 months) including classroom theory and supervised clinical practice.
- Passing the NCLEX-PN, which tests foundational competencies: safe and effective care, health promotion, psychosocial integrity, and physiological integrity.
- Application for licensure through the state board of nursing, which may include background check and fees.
- Some states require periodic license renewal (e.g., every two years for LVNs), which may include mandated continuing education or contact hours.
In addition to basic licensure, LVNs may choose to obtain voluntary specialty certifications, such as IV therapy, gerontology, wound care, or long-term care — depending on employer preference or personal career goals.
These optional credentials allow vocational nurses to highlight advanced competencies beyond entry-level skills, potentially improving employability or allowing more responsibilities within the licensed vocational role.
What ongoing continuing education and specialty certifications can rns pursue, such as nurse practitioner or clinical nurse specialist?
For a registered nurse (RN), licensure typically demands graduation from an accredited nursing program (such as an associate degree or bachelor’s degree), followed by passage of the NCLEX-RN, and submission of an application to the relevant state board of nursing.
Once licensed, RNs have a broader legal and clinical scope of practice compared to vocational nurses. But beyond initial licensure, many RNs pursue continuing education and specialty certifications to advance their careers. Some of these include:
- Certifications for advanced practice roles (e.g., as a Nurse Practitioner, Clinical Nurse Specialist, nurse anesthetist, or other advanced practice nursing roles), provided regulatory and educational requirements are satisfied.
- Specialty certifications in areas like critical care, pediatrics, community health, geriatrics, oncology, and more, depending on interest, experience, and further training.
- Continuing education (CE) requirements vary by state: many states require RNs to complete a set number of CE contact hours for license renewal. For instance, some jurisdictions mandate one contact hour per month of non-practice, or a defined number of hours if returning to practice after a break.
- For RNs pursuing advanced practice or leadership, additional academic degrees (e.g., master’s or doctoral degrees) may be necessary, alongside national certifications recognized by regulatory bodies.
Continuing education and specialty certification help RNs stay current with evolving clinical standards, expand their competencies, and qualify for advanced or specialized roles — thus supporting long-term career goals and professional development.
How do state regulations affect rn scope of practice and licensed vocational nurse duties?
The roles, responsibilities, and allowed practices of both LVNs and RNs are governed by state-specific laws, often defined under the state’s Nurse Practice Act (or similar regulatory statutes) and enforced by the state board of nursing.
For LVNs, state regulations typically limit their scope to basic nursing care and supportive tasks under supervision of an RN or physician. LVNs are not permitted to perform many of the advanced assessments, independent clinical decisions, or invasive procedures that RNs can legally undertake.
State-to-state variation can also affect:
- What medications or treatments an LVN may administer. Some states permit certain IV therapy or medication administration by LVNs or LPNs under defined protocols; others do not.
- The requirements for continuing education and license renewal. For example, some states mandate a set number of CE hours within a renewal cycle or require reactivation education after a period of non-practice.
- The privileges and responsibilities of advanced practice RNs or specialty RNs (e.g., nurse practitioners) — which often require additional certification, credentialing, and adherence to scope limitations defined by law.
For example, in some states, an LVN cannot administer IV push medications or blood products — tasks reserved for RNs. Meanwhile, an RN may supervise LVNs or nursing assistants, delegate duties appropriately, and take full responsibility for patient care outcomes. Institutional policies — in addition to regulatory law — may further define or limit practice based on facility type (nursing home, hospital, clinic) or patient acuity.
Conclusion
Understanding the differences between LVNs/LPNs and RNs is essential for aspiring nurses to make informed decisions about their nursing career. While both roles play vital parts in patient care, the scope of practice, educational requirements, responsibilities, and opportunities for advancement vary significantly. Licensed vocational nurses provide foundational basic nursing care, often working under the supervision of an RN, and can enter the workforce quickly through vocational nursing programs. Registered nurses, by contrast, pursue more extensive education—whether through an associate degree in nursing (ADN) or a bachelor of science in nursing (BSN)—which equips them with a broader scope of practice, complex nursing skills, leadership opportunities, and access to advanced practice roles such as nurse practitioner or clinical nurse specialist.
Salary differences reported by the Bureau of Labor Statistics highlight the financial advantages of RN licensure, while bridge programs and continuing education provide LVNs pathways to expand their scope and transition into RN roles. State regulations and the nurse practice act further shape the responsibilities and limitations of each profession, ensuring that patient care remains safe, ethical, and evidence-based.
Ultimately, the choice between pursuing an LVN/LPN program or committing to an RN path depends on individual career goals, desired responsibilities, long-term growth, and personal circumstances. Whether entering the field as a vocational nurse or registered nurse, both paths offer meaningful opportunities to impact patient outcomes, contribute to healthcare teams, and develop a fulfilling career in nursing. By understanding the differences, scope, and progression opportunities, aspiring nurses can strategically navigate their education and professional journey toward rewarding roles in healthcare.
Frequently Asked Questions
What is the difference between LPN, LVN, and RN?
- LPN (Licensed Practical Nurse) and LVN (Licensed Vocational Nurse) are essentially the same; the term depends on the state—LVN is commonly used in California and Texas. Both provide basic nursing care under the supervision of an RN or physician, including monitoring vital signs, administering medications, and assisting with daily patient needs.
- RN (Registered Nurse) has a broader scope of practice, can perform advanced clinical assessments, develop nursing care plans, administer complex treatments, supervise LVNs and nursing assistants, and pursue advanced roles like nurse practitioner or clinical nurse specialist.
What is the difference between the role of the RN and the role of the LPN in the nursing process?
- LPNs/LVNs participate in the nursing process primarily by implementing care plans, observing pati Is it better to do LPN to RN or just RN?
- If you want quick entry into nursing, starting as an LPN/LVN can provide practical experience while earning a salary. Later, you can bridge to RN through LPN-to-RN programs.
- If your goal is long-term advancement, broader scope of practice, higher salary, and eligibility for advanced practice roles, enrolling directly in an RN program (ADN or BSN) is often the faster and more strategic choice.
- RNs are responsible for assessing patients, diagnosing nursing problems, planning care, implementing interventions (including delegating tasks to LPNs), and evaluating outcomes, making them accountable for the full nursing process.
Which best describes the difference between a licensed practical nurse (LPN) and a nursing assistant?
- LPN/LVN: Provides basic nursing care, administers medications, monitors vital signs, and assists in patient assessments under RN supervision.
- Nursing Assistant (CNA): Focuses on direct patient support, such as bathing, feeding, assisting with mobility, and reporting changes to nurses, but does not administer medications or perform nursing assessments.
