Child and Adolescent Elimination Disorders: Managing Fecal Incontinence and Behavioral Factors
Elimination disorders represent a significant area of concern in pediatric and adolescent nursing, encompassing challenges in both bowel and bladder control that can affect physical health, psychological well-being, and social functioning. These conditions, which include encopresis and enuresis, are not merely behavioral issues—they often reflect a complex interplay of physiological, developmental, and psychosocial factors. A child with encopresis may experience involuntary fecal incontinence or soiling, while children and adolescents with enuresis may struggle with nocturnal or diurnal urine control. Both conditions require careful assessment, understanding of contributing factors, and evidence-based interventions to support continence and promote healthy development.
In clinical practice, understanding elimination disorders in children involves recognizing typical bowel and urinary patterns, identifying deviations that indicate chronic constipation or inappropriate elimination, and appreciating how behavioral and toilet training practices influence outcomes. Pediatric psychology, developmental stage, and familial support also play critical roles in shaping a child’s ability to use the toilet effectively and maintain good bowel habits. Furthermore, the interaction between bladder and bowel function underscores the importance of a holistic assessment, as urinary incontinence and encopresis can frequently co-occur, complicating treatment strategies.
This article provides a comprehensive overview of elimination disorders in children and adolescents, examining clinical presentation, causes, assessment techniques, and evidence-based treatment approaches. By integrating physiological understanding with behavioral and psychosocial considerations, nurses and healthcare providers can implement structured assessment and treatment plans that address both medical and behavioral components of these disorders. Emphasis is placed on practical guidance for managing fecal incontinence, promoting healthy bowel and bladder habits, and supporting children and their families through multidisciplinary interventions. The discussion also highlights the relevance of treatment guidelines, assessment strategies, and outpatient care practices at institutions such as Wolaita Sodo University Comprehensive Specialized Hospital, providing a framework for evidence-based pediatric nursing practice.
Understanding Elimination Disorders in Children and Adolescents
Elimination disorders refer to clinically significant difficulties in the control of bladder or bowel functions that are inappropriate for a child’s developmental level. In pediatric populations, these challenges extend beyond simple accidents—their effects reach into emotional well‑being, family dynamics, and school functioning. A nurse caring for children with elimination disorders must understand not only the physical mechanisms of bladder and bowel control but also the behavioral and psychosocial contexts in which these problems occur.
Elimination involves two fundamental physiologic processes: voluntary control of bowel evacuation and urinary release. Continence develops gradually as neural pathways and behavioral skills mature, usually by early school age. When a child cannot reliably use the toilet in a socially acceptable manner—even in the absence of an underlying medical condition—this warrants further clinical evaluation.
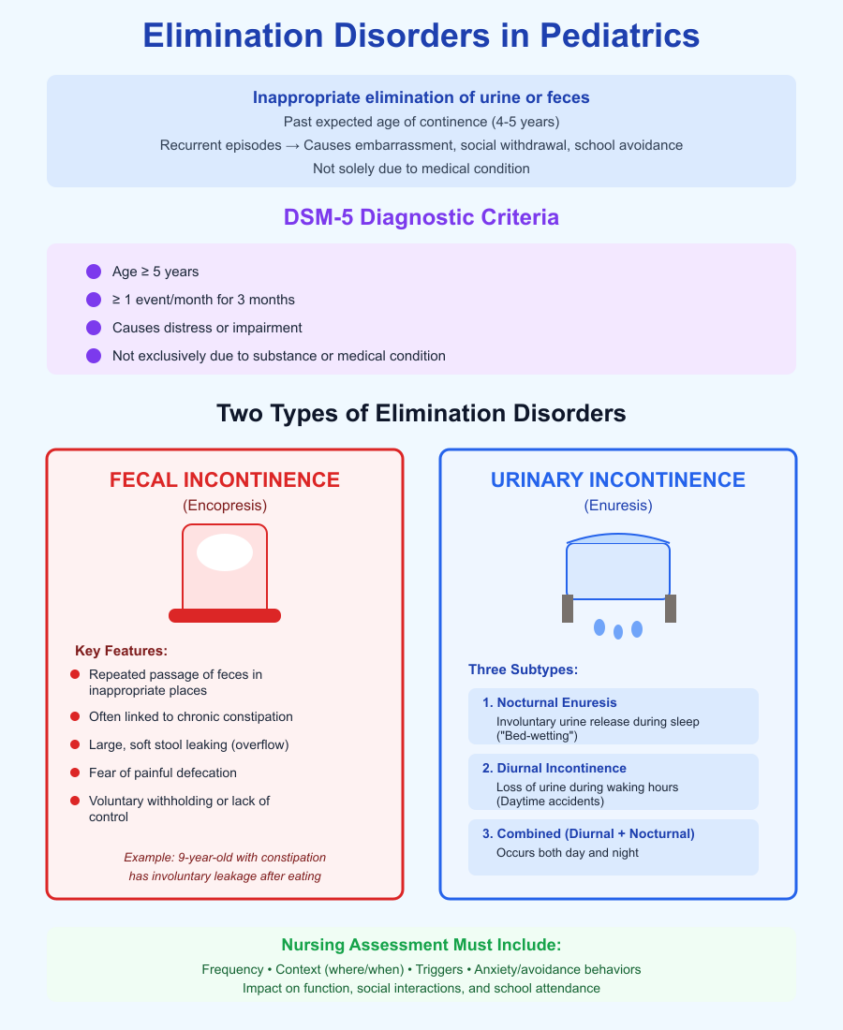
Definition and Clinical Overview of Elimination Disorder in Pediatrics
An elimination disorder in pediatrics includes patterns of inappropriate elimination of urine or feces that are not attributable solely to a medical condition and that persist past the age at which continence is expected.
Key elements of this definition include:
- Age‑appropriate expectations: Most children achieve daytime bladder and bowels control by about 4–5 years of age. Persistent loss of control after this age represents a deviation from typical development.
- Frequency and duration: Recurrent episodes—rather than isolated accidents—indicate a pattern.
- Impact on function: These difficulties can lead to embarrassment, social withdrawal, school avoidance, and caregiver stress.
Nurses must assess not only the frequency of accidents but also context—where they occur, associated triggers, and whether the child exhibits anxiety or avoidance behaviors around elimination.
DSM-5 Criteria for Elimination Disorder and Encopresis
The Statistical Manual of Mental Disorders (DSM‑5) provides structured diagnostic criteria for identifying specific elimination disorders.
Criteria for elimination disorders generally include:
- A marked pattern of urinary or fecal elimination that is appropriate for enuresis or encopresis
- Behavior that occurs with sufficient frequency to cause distress or impairment
- Chronological age of at least 5 years
- Exclusion of problems explained solely by a substance or a medical condition
Encopresis (with or without constipation):
- Repeated passage of feces into inappropriate places (e.g., clothing or floor) by a child who has reached the developmental age of 5 years
- At least one such event occurs each month for 3 months
- Either voluntary withholding or lack of control is present
- The behavior is not due exclusively to a medical condition
This systematic framework helps clinicians differentiate between typical developmental variability and clinically significant disorders, guiding assessment and intervention planning.
Types of Elimination: Fecal Incontinence vs Urinary Incontinence
Understanding the distinctions between types of elimination difficulties is essential for accurate nursing assessment and care planning.
1. Fecal Incontinence
Fecal incontinence describes the involuntary passage of stool in children who are developmentally expected to have bowel control. In pediatric practice, this term often refers to persistent soiling associated with chronic constipation or pediatric encopresis.
Clinical features may include:
- Repeated bowel accidents, especially after a child has been toilet trained
- Large, soft stool leaking during the day
- Avoidance of bathroom use due to fear of pain with defecation
Example: A 9‑year‑old boy with a history of constipation in children may have infrequent bowel movements followed by large, involuntary leakage of feces, particularly after eating. Parents may describe soiling in underwear despite attempts at toileting, indicating fecal incontinence due to overflow.
2. Urinary Incontinence
Urinary incontinence refers to lapses in bladder control. It encompasses issues such as diurnal enuresis, nocturnal enuresis, or mixed daytime and nighttime symptoms.
Types include:
- Nocturnal enuresis: Involuntary urine release during sleep; often called “bed‑wetting”
- Diurnal incontinence: Loss of urine during waking hours
- Combined (diurnal and nocturnal enuresis): Occurring both day and night
Example: An adolescent with nocturnal enuresis in children may struggle with bed‑wetting several nights per week, despite being dry during daytime hours. This pattern has substantial psychosocial effects and requires a distinct treatment approach compared with isolated daytime wetting.
Key Distinctions Between Fecal and Urinary Incontinence:
| Feature | Fecal Incontinence | Urinary Incontinence |
|---|---|---|
| Primary substance lost | Stool (feces) | Urine |
| Common contexts | After bowel movements, leakage due to overflow | Sleep (nocturnal) or daytime activities |
| Typical associated condition | Chronic constipation, encopresis | Functional bladder disorders, delayed bladder control |
| Behavioral impact | Avoidance of bathroom, embarrassment | Sleep disruption, social anxiety |
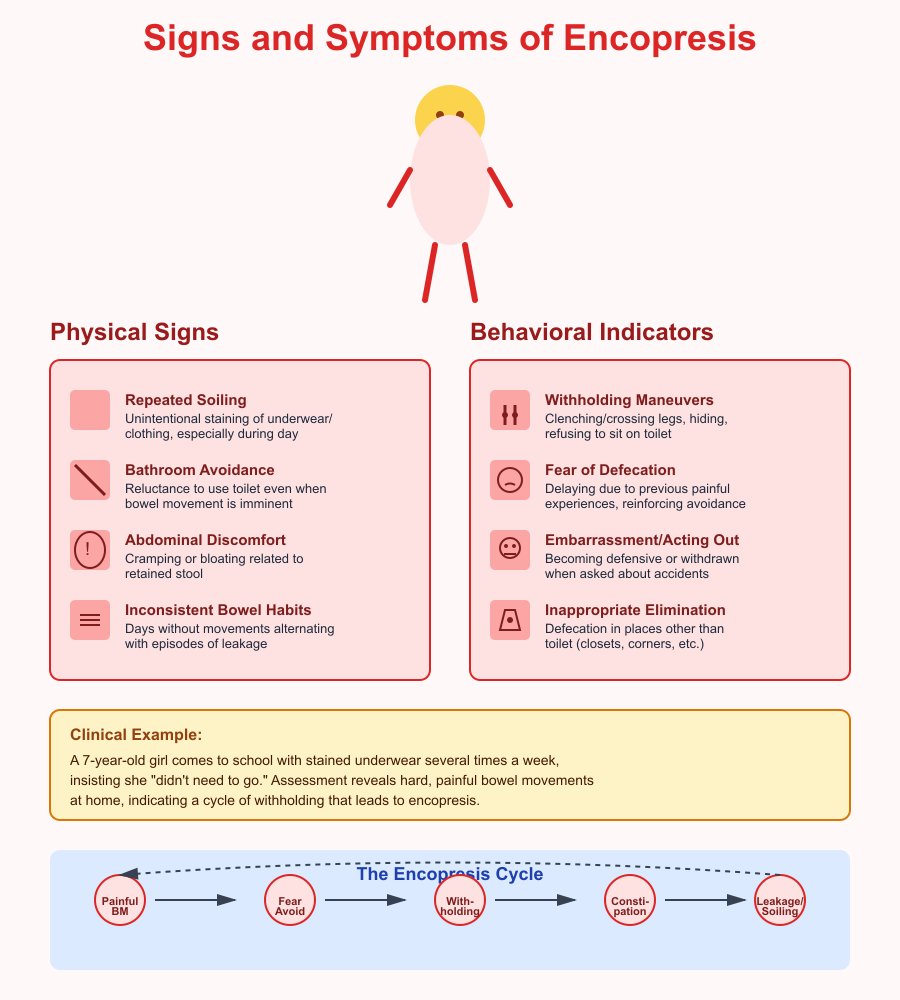
Clinical Presentation of Encopresis in Children
Encopresis is a type of pediatric elimination disorder in which a child with encopresis repeatedly passes feces in inappropriate places (e.g., underwear, floors) after the expected age of continence. Understanding the clinical presentation of encopresis requires careful attention to both physical symptoms and behavioral cues, as well as how chronic bowel dysfunction contributes to involuntary leakage.
Signs and Symptoms of a Child with Encopresis
Children with encopresis may display a range of physical and observable signs. These can appear subtle initially, making early detection dependent on thorough history taking and clinical observation.
Common signs and symptoms include:
- Repeated soiling: Unintentional staining of underwear or clothing with fecal matter, especially during the day.
- Avoidance of the bathroom: Reluctance to use the toilet even when a bowel movement is imminent.
- Complaints of abdominal discomfort: A child may report cramping or bloating related to retained stool.
- Inconsistent bowel habits: Alternating between days without bowel movements and episodes of leakage.
- Pain with defecation: Children may resist bowel movements due to fear of stool pain, contributing to withholding behaviors.
Example: A 7‑year‑old girl may come to school with stained underwear several times a week, yet insist she “didn’t need to go” when asked. Upon assessment, she may describe hard, painful bowel movements at home, indicating a cycle of withholding that leads to encopresis.
Behavioral Indicators and Inappropriate Defecation Patterns
Encopresis is not solely a physical condition—it often involves distinct behavioral patterns that reflect a child’s response to painful or difficult elimination.
Behavioral indicators include:
- Withholding maneuvers: Clenching legs, crossing legs, hiding behind objects, or refusing to sit on the toilet.
- Fear of defecation: A child may delay bowel movements due to previous painful experiences, reinforcing avoidance.
- Acting out or embarrassment: Some children may become defensive or withdrawn when asked about accidents.
- Inappropriate elimination: Defecation in places other than the toilet, such as closets, corners, or underneath furniture.
- Toilet resistance: Refusal or distress when encouraged to sit on the toilet for bowel movements.
These behaviors often develop as coping strategies to avoid discomfort. Pediatric nurses should observe the context of accidents and talk with caregivers to distinguish between voluntary withholding and involuntary loss.
Chronic Constipation and Its Role in Fecal Incontinence
Chronic constipation plays a central role in the pathophysiology of encopresis and related fecal leakage. Chronic constipation involves infrequent or hard bowel movements that cause pain and difficulty during defecation. Over time, this leads to stool retention and stretching of the rectum.
Mechanisms by which chronic constipation contributes to fecal incontinence include:
- Rectal dilation: Persistent stool retention causes the rectum to stretch, reducing sensation and control.
- Overflow leakage: Soft stool may pass around the retained stool mass, leading to unintended soiling.
- Disrupted signaling: Long‑standing stool retention interferes with normal bowel reflexes, making voluntary control more difficult.
Example: A school‑aged boy who experiences painful bowel movements every few days may start to avoid the bathroom. As retained stool accumulates, his rectal muscle stretch reduces normal sensation, and soft stool begins to leak, causing fecal incontinence.
Typical Bowel Movement Patterns and Stool Characteristics
Recognizing normal vs. abnormal bowel patterns is essential for identifying encopresis. A healthy child typically has:
- Regular bowel movements ranging from once daily to once every other day.
- Formed, soft stools that are comfortable to pass.
- No routine pain, straining, or reluctance to go.
In contrast, clinical features suggestive of encopresis include:
- Infrequent movements: Fewer than three bowel movements per week.
- Hard, pellet‑like stool: Indicates prolonged stool transit and dehydration.
- Large, bulky stools: Suggests significant stool retention.
- Sudden leakage of soft stool: Especially when no urge is reported.
Nurses should assess not only frequency but also stool consistency, using caregiver reports and tools like the Bristol Stool Chart to standardize assessment.
Causes and Associated Factors Among Children and Adolescents
Understanding the causes of elimination disorders in both child and adolescent populations is essential for accurate assessment and effective intervention. Encopresis and related patterns of inappropriate elimination often arise from multiple interacting factors—physiologic, developmental, psychosocial, and learned behaviors. Recognizing these contributors helps clinicians and nursing students identify individualized strategies that support continence and overall well‑being.
Gastrointestinal and Medical Factors Contributing to Encopresis
Gastrointestinal functioning plays a central role in many cases of pediatric encopresis. When the normal processes of digestion and bowel transit are disrupted, a child with encopresis may experience stool retention and leakage.
Key medical contributors include:
- Chronic constipation: Persistent difficulty with stool passage slows normal bowel transit and often leads to fecal incontinence.
- Rectal dilation: With continued retention, the rectum stretches and loses sensitivity, making it harder for the child to sense the need for a bowel movement.
- Painful defecation: Hard, dry feces can cause pain, prompting the child to withhold rather than go to the bathroom.
- Physiologic disorders: Conditions like Hirschsprung’s disease or functional constipation alter gut motility.
Example: In constipation in children, hard bowel movements can create a cycle where a child avoids defecation because of fear of pain. This leads to greater retention, rectal stretching, and eventual leakage of softer stool around the blockage.
Behavioral and Toilet Training Factors Among Children
Early experiences with using the toilet can shape long‑term elimination patterns. Poorly timed or overly pressured toilet training may contribute to behavioral avoidance and dysfunctional toilet habits.
Behavioral contributors include:
- Inconsistent training practices: Children who are rushed into toilet training before readiness may develop anxiety about going to the toilet.
- Negative reinforcement: Punishment, shaming, or frustration around toilet use can make a child resistant to elimination routines.
- Withholding behaviors: After painful stooling, a child learns to hold in stool, increasing stool retention and chronic constipation.
Example: A toddler pushed into toilet training “too early” may associate the toilet with stress and delay elimination, leading to encopresis as older children resist going to the bathroom even when physically ready.
Pediatric Psychological Factors Influencing Elimination Disorders
Emotional and cognitive patterns significantly affect elimination control. Pediatric psychology recognizes that anxiety, stress, and emotional regulation difficulties can manifest through bowel and bladder dysfunction.
Psychological factors include:
- Behavioral problems: Fearful or oppositional behaviors may delay toilet routines.
- Mental health conditions: Anxiety disorders or psychiatric disorders can exacerbate withdrawal from regular bowel and bladder habits.
- Avoidant behaviors: Children who resist established routines may choose places other than the toilet for elimination.
Example: A school‑aged child with heightened anxiety about social evaluation may avoid using school bathrooms, resulting in withheld stool that contributes to encopresis.
Developmental and Risk Factors in Adolescents
While encopresis is more common in younger children, adolescent physiology and behavior also influence presentations.
Developmental risk factors include:
- Delayed maturation of neuromuscular control: Some older children experience prolonged immaturity of bowel or bladder pathways.
- Social stressors: School demands, peer relationships, and self‑consciousness impact willingness to use public toilets.
- Ongoing constipation: Persistent dysfunctional elimination from earlier years may continue into adolescence without appropriate intervention.
Example: An adolescent experiencing ongoing constipation may report frequent accidents at school, linked to a pattern of avoiding toilets due to embarrassment or fear of peer stigma.
Interaction Between Enuresis and Encopresis
Encopresis often co‑occurs with patterns of urinary elimination dysfunction. The interplay between these conditions—such as enuresis and encopresis—is common, reflecting underlying developmental or behavioral interactions.
Important considerations:
- Concurrent patterns: A child might exhibit both fecal and urinary incontinence, especially during periods of stress or developmental transitions.
- Shared mechanisms: Delayed control of bladder and bowel muscles can result in both diurnal enuresis and encopresis in the same child.
Example: A 10‑year‑old may experience daytime leakage of urine (diurnal enuresis) while also having fecal soiling episodes, pointing to intertwined pelvic floor dysfunction and rhythmic patterns of elimination.
Bladder-Bowel Interactions and Nocturnal Enuresis
The bladder and bowel systems interact closely through shared neural pathways and muscle groups. Dysfunction in one often affects the other.
Key points include:
- Overloaded rectum: A rectum distended by retained stool can compress the bladder, reducing capacity and leading to nocturnal enuresis in children.
- Sleep patterns: Disturbed sleep associated with nocturnal symptoms can impact daytime continence routines.
- Functional overlap: Some children with constipation have secondary urinary symptoms due to local pelvic pressure.
Example: A child with significant fecal retention may experience bed‑wetting at night because the distended bowel puts pressure on the bladder, reducing room for urine storage during sleep.
Assessment of Elimination Disorders in Pediatric Patients
Effective assessment of elimination disorders requires a holistic approach that integrates medical history, observational tools, physical examination, and screening for related conditions. Accurate evaluation enables clinicians to distinguish between patterns such as enuresis, encopresis, and mixed presentations, guiding targeted interventions and improving outcomes for children.
Comprehensive History and Identification of Causes
A thorough history is fundamental to identifying the root contributors to elimination dysfunction. Nurses should gather detailed information from both the child and caregivers.
Key components of the history include:
- Onset and pattern: Establish when symptoms began, frequency of accidents, and whether symptoms are daytime, nighttime, or both.
- Bowel habits: Clarify typical bowel movement frequency, consistency of stool, and any spells of pain with defecation.
- Urinary patterns: Gather information on urine control during day and night.
- Behavioral context: Ask about avoidance of toilet use, reactions to accidents, and child’s attitudes toward going to the bathroom.
- Medical and family history: Explore developmental history, past episodes of constipation, and any family history of similar conditions.
Example: A 6‑year‑old may present with daytime soiling and occasional bed‑wetting. A careful history might reveal infrequent, painful bowel movements with hard stools, suggesting underlying chronic constipation as a primary cause.
Use of Bowel Diaries and Behavioral Tracking
Bowel diaries and behavioral tracking tools are practical, evidence‑based strategies that help quantify elimination patterns and identify triggers.
Benefits of these tools include:
- Objective data collection: Records timing, consistency, and context of bowel and bladder events.
- Pattern recognition: Helps detect links between diet, toilet habits, and episodes of incontinence.
- Behavioral insight: Reveals avoidance behaviors, inappropriate elimination locations, and times of greatest difficulty.
What to track:
- Date and time of each bowel movement and urination
- Stool consistency (e.g., hard, soft, formed)
- Episodes of leakage or accidents
- Behavioral responses (e.g., refusal to use the toilet)
- Diet and fluid intake
Physical Examination and Pediatric Assessment Techniques
A focused physical examination complements historical and diary data. The goal is to identify physical contributors and rule out structural or neurologic abnormalities.
Examination components include:
- Abdominal evaluation:
- Palpate for distended abdomen or hard stool masses
- Assess for discomfort during palpation
- Perineal inspection:
- Look for signs of irritation
- Evaluate skin integrity around the rectum and genital area
- Neurologic screening:
- Check lower extremity reflexes and sensation
- Observe gait and posture for signs of neuromuscular issues
- Functional toileting assessment:
- Observe the child’s ability to sit on a toilet or commode
- Note any reluctance, fear, or distraction
Example: During examination, a nurse might feel a firm mass in the lower abdomen of a child reporting infrequent bowel movements. This finding supports assessment of fecal retention as a contributor to encopresis and guides further management.
Screening for Concurrent Enuresis and Encopresis
Because bladder and bowel functions are closely linked, screening for both conditions is essential. A child who presents with soiling episodes may also experience urinary incontinence or episodes of nocturnal enuresis without initially reporting them.
Screening strategies include:
- Direct questioning: Ask about nighttime bed‑wetting and daytime dribbling of urine.
- Standardized questionnaires: Use age‑appropriate tools to assess degree of control and impact on daily functioning.
- Observation of voiding routines: Evaluate patterns of voiding, frequency, urgency, and ability to delay urination.
Example: A 9‑year‑old referred for encopresis may be found, upon screening, to also have bed‑wetting episodes 2–3 nights per week. Identifying concurrent enuresis in children informs a more comprehensive, multidisciplinary treatment approach.
Evidence-Based Treatment of Elimination Disorders
Treating elimination disorders in child and adolescent patients requires a multimodal, evidence‑based approach that addresses both the physical aspects (such as chronic constipation and fecal incontinence) and the behavioral patterns that maintain or worsen symptoms. Best outcomes stem from combining medical management, structured behavioral interventions, and coordinated multidisciplinary care. Below is a comprehensive discussion of key treatment strategies, including practical examples and clinical evidence.
Medical Management: Laxatives, Bowel Cleanouts, and Chronic Constipation Treatment
Medical treatment is often the first step, especially when functional constipation underlies chronic encopresis or fecal incontinence.
Core medical interventions include:
- Initial bowel cleanout:
- Using laxatives or enemas to evacuate retained stool and break the cycle of retention and overflow incontinence.
- Cleanouts may involve high‑dose polyethylene glycol or other osmotic agents that draw water into the colon to soften and flush stool.
- Maintenance therapy:
- Once cleanout is achieved, daily osmotic or stool‑softening laxatives maintain regular bowel movements and prevent stool buildup.
- Examples include polyethylene glycol (PEG) products, lactulose, and mineral oil, which allow the child to have soft, easy bowel movements and reduce painful defecation.
Why this matters:
- Addressing constipation medically reduces the physical obstruction that contributes to involuntary leakage, and eases discomfort that might lead to toilet training avoidance.
- In some cases, treating constipation alone can also improve associated urinary symptoms like daytime wetting or even nocturnal enuresis due to reduced rectal pressure on the bladder, emphasizing the bladder‑bowel link.
Example:
A 7‑year‑old referred for frequent soiling is started on polyethylene glycol following fecal impaction. Within weeks, daily soft stools are achieved, reducing episodes of fecal incontinence and promoting more successful attempts to use the toilet regularly.
Behavioral Interventions and Toilet Training Strategies
Medical therapy alone is usually insufficient; behavioral approaches are critical to establish regular, healthy elimination habits and modify patterns that contribute to encopresis and incontinence.
Effective behavioral strategies include:
- Enhanced Toilet Training (ETT):
- A structured protocol combining toileting schedules after meals (to leverage the gastrocolic reflex), rewards for successful attempts, and education on body cues and proper straining technique. This approach has been shown to improve outcomes in children with encopresis when combined with medical management of constipation.
- Toileting routines:
- Encouraging the child to sit on the toilet for 5–10 minutes at the same time each day (often after meals) can help normalize bowel habits and build predictable elimination patterns.
- Positive reinforcement:
- Use of praise or reward systems for sitting on the toilet or having a bowel movement can encourage participation and reduce avoidance behaviors.
- Education:
- Teaching children and families about normal elimination physiology and reducing fear or behavioral problems associated with defecation is essential.
Example:
A 9‑year‑old with long‑standing encopresis is placed on a structured plan where she sits on the toilet for 10 minutes after breakfast and dinner. Combined with softened stools, she begins to have regular toileting success and fewer episodes of inappropriate elimination.
Multidisciplinary Care and Outpatient Clinic Referral at Wolaita Sodo University Comprehensive Specialized Hospital
Complex cases of elimination disorders—especially those involving co‑occurring psychological or behavioral challenges—benefit from multidisciplinary intervention. At specialized centers such as the outpatient clinic at Wolaita Sodo University Comprehensive Specialized Hospital, clinicians can integrate medical, psychological, and parental support to optimize care.
Key elements of multidisciplinary care may include:
- Pediatricians and gastroenterologists to manage constipation and discharge planning
- Nurses and continence specialists to support routine building and toileting habit development
- Pediatric psychologists who can address underlying behavioral or emotional barriers to progress
- Parent education programs to improve parenting practices, as poor supervision and low toilet training skills are associated with higher risk of persistent elimination disorders in children and adolescents.
Referral to such outpatient settings is recommended when:
- Symptoms are resistant to initial management
- There is significant emotional or psychosocial stress associated with the disorder
- The child shows concurrent behavioral challenges affecting toileting routines
This collaborative model promotes holistic care, reducing stigma and improving adherence to treatment.
Developing a Treatment Plan Combining Bowel Management, Behavioral Therapy, and Education
An individualized treatment plan should blend medical and behavioral strategies, family education, and regular follow‑up.
Components of an effective treatment plan:
- Medical component:
- Initiate bowel cleanout as needed
- Implement and adjust laxative regimen based on daily stool patterns
- Regularly monitor progress and side effects
- Behavioral component:
- Build a toilet routine with consistent timing and positive reinforcement
- Use tools like reward charts, bowel diaries, and scheduled toilet sits
- Incorporate education about sensations and cues related to elimination
- Family and educational support:
- Provide clear guidance to parents and caregivers about expectations, normal patterns, and strategies to reduce avoidance
- Empower children and their families to participate actively in the plan
- Ongoing monitoring:
- Frequent evaluation of symptoms, accidents, and compliance helps refine the plan
- Adjust strategies if goals are not being met or as new challenges arise
Example:
A school‑aged child with encopresis and associated stool withholding is given a phased plan that starts with a bowel cleanout, transitions into daily PEG for maintenance, and incorporates a post‑meal toileting routine paired with a reward chart. Caregivers receive education about avoiding punishment and recognizing stool cues, while periodic follow‑ups ensure progress and allow adjustments.

Follow-Up, Monitoring, and Prevention Strategies
Effective follow‑up and prevention are essential components of care for children with elimination disorders. After initiating assessment and treatment, nurses must ensure ongoing evaluation, adjust interventions based on progress, support children and their families, and integrate structured treatment guidelines into everyday pediatric practice. These strategies help sustain gains, prevent recurrence, and address emerging concerns promptly.
Ongoing Assessment and Treatment Adjustments
Maintaining continence and promoting healthy elimination patterns require structured follow‑up and continuous evaluation. Monitoring should be tailored to the child’s developmental level and specific needs.
Key elements of ongoing monitoring include:
- Regular review of symptoms:
- Track episodes of fecal leakage, daytime wetting, or nighttime accidents to identify patterns over time.
- Use standardized tools and diaries to objectively capture progress and setbacks.
- Evaluation of interventions:
- Assess whether current laxatives or behavior plans remain effective.
- Collaborate with caregivers and the child to refine schedules and goals.
- Growth and development appraisal:
- Monitor for changes associated with age, especially in older children and adolescent patients whose routines and responsibilities evolve.
- Attention to co‑occurring issues:
- Observe for health conditions such as iron deficiency anemia or urinary tract infections that may influence elimination patterns.
- Adjustment of education and support:
- Reinforce teaching about good bowel habits and proper positioning for elimination with every visit.
Example:
A school‑aged child initially managed for encopresis may show improvement but begin having more accidents during school exams. A follow‑up visit could reveal performance anxiety affecting toileting routine, prompting adjustment of the behavior plan to include coping strategies and scheduled bathroom breaks.
Preventing Relapse and Maintaining Continence in Children and Adolescents
Prevention of relapse is as important as initial management, especially because elimination patterns are sensitive to stress, routine changes, and evolving psychosocial contexts.
Strategies to support sustained progress include:
- Structured routines:
- Encourage consistent timing for meals and toileting to regulate bowel movement patterns.
- Reinforce regular opportunities to use the toilet, particularly after meals when the gastrocolic reflex is strongest.
- Education on triggers and cues:
- Help children and caregivers recognize early signs of stool retention or urinary urgency.
- Reinforcement of healthy habits:
- Promote balanced hydration and dietary fiber to prevent constipation in children
- Use reward systems that celebrate small successes without pressuring the child.
- Support through transitions:
- Anticipate changes such as school entry, puberty, or changes in caregiver routines that may disrupt habits.
- Address psychosocial contributors:
- Because elimination disorders are common in boys and may be linked with broader mental health conditions, maintain awareness of emotional stressors that can precipitate regression.
Example:
An adolescent who has achieved continence may begin to experience daytime leakage after starting a new sport. Identifying that fluid intake timing and bathroom access are inconsistent allows adjustment of fluid schedules and planned toilet breaks to maintain continence.
Integrating Treatment Guidelines in Pediatric Nursing Practice
Nursing practice benefits greatly from the consistent application of evidence‑based protocols and treatment guidelines. These frameworks standardize care while allowing personalization based on individual response.
Best practices for integration include:
- Use of standardized care pathways:
- Adopt clinical guidelines that specify assessment frequency, criteria for escalating care, and indicators for referral.
- Documentation and communication:
- Record monitoring data systematically to inform clinical decisions and share with the broader care team, including physicians and therapists.
- Education and training:
- Ensure that pediatric nursing staff are familiar with interventions such as internet intervention for pediatric encopresis tools, toileting schedules, and reinforcement techniques.
- Family partnership:
- Engage children and their families in setting realistic goals and understanding the rationale behind each part of the care plan.
- Clinic collaboration:
- When indicated, refer to specialized services such as the outpatient clinic at Wolaita Sodo University Comprehensive Specialized Hospital or related pediatric continence programs for advanced evaluation and support.
Example:
A nurse implementing a guideline‑driven follow‑up schedule ensures that every child who has achieved continence is seen at regular intervals. Notes from these visits help guide timely adjustments and identify when specialized referral—for instance to the clinic at Wolaita Sodo University—is necessary due to persistent or complex symptoms.
Conclusion
Elimination disorders in child and adolescent populations, including encopresis and enuresis, represent complex conditions that intertwine physiological, behavioral, and psychosocial factors. A child with encopresis may experience fecal incontinence due to chronic constipation, learned withholding behaviors, or underlying medical or developmental conditions, while urinary incontinence and nocturnal enuresis in children frequently co-occur due to the close interaction between the bladder and bowel systems.
Effective management requires a comprehensive, evidence-based approach. Nursing assessment—including detailed history-taking, physical examination, and use of bowel diaries and behavioral tracking—enables clinicians to identify underlying causes and monitor progress. Treatment plans that combine medical management (such as laxatives and bowel cleanouts) with structured behavioral interventions, toilet training, and family education have been shown to improve continence, reduce episodes of involuntary elimination, and foster good bowel habits among children and adolescents.
Moreover, integrating multidisciplinary care through specialized centers, such as the outpatient clinic at Wolaita Sodo University Comprehensive Specialized Hospital, ensures that children receive holistic support addressing both physical and psychological contributors. Continuous follow-up, monitoring, and prevention strategies are essential to sustain gains, prevent relapse, and maintain long-term continence, while embedding treatment guidelines into pediatric nursing practice enhances standardization, efficiency, and safety of care.
Ultimately, the nursing role extends beyond symptom management: it encompasses education, advocacy, and support for families, enabling children to navigate elimination challenges with confidence and dignity. By understanding the multifactorial causes of elimination disorders, applying evidence-based encopresis in children strategies, and maintaining vigilant follow-up, nurses can improve patient outcomes, promote healthy bowel and urinary habits, and contribute to the overall well-being and development of children and adolescents.
Frequently Asked Questions
What are elimination disorders?
Elimination disorders are conditions in children and adolescents characterized by involuntary or inappropriate control of urine or feces, including enuresis (urinary incontinence) and encopresis (fecal incontinence). They can result from medical, behavioral, psychological, or developmental factors affecting bowel and bladder function.
What is the main cause of bedwetting?
The most common cause of nocturnal enuresis in children (bedwetting) is delayed maturation of bladder control, often combined with a genetic predisposition, reduced nighttime urine concentration, and sometimes behavioral factors.
What are elimination problems?
Elimination problems refer to difficulties in controlling urine or feces, which can include daytime urinary incontinence, bedwetting, fecal soiling, constipation, or resistance to going to the bathroom at appropriate times. They often interfere with daily activities and psychosocial development.
What is the commonest cause of enuresis in children?
The most common cause of enuresis in children is functional or primary nocturnal enuresis, typically due to immature bladder control and delayed arousal from sleep, rather than an underlying medical condition.
