Gordon Functional Health Patterns is a theoretical framework for health assessment developed by M. Gordon in 1987. The model provides a comprehensive and systematic approach to nursing assessment to capture an individual’s holistic health status and promote health.
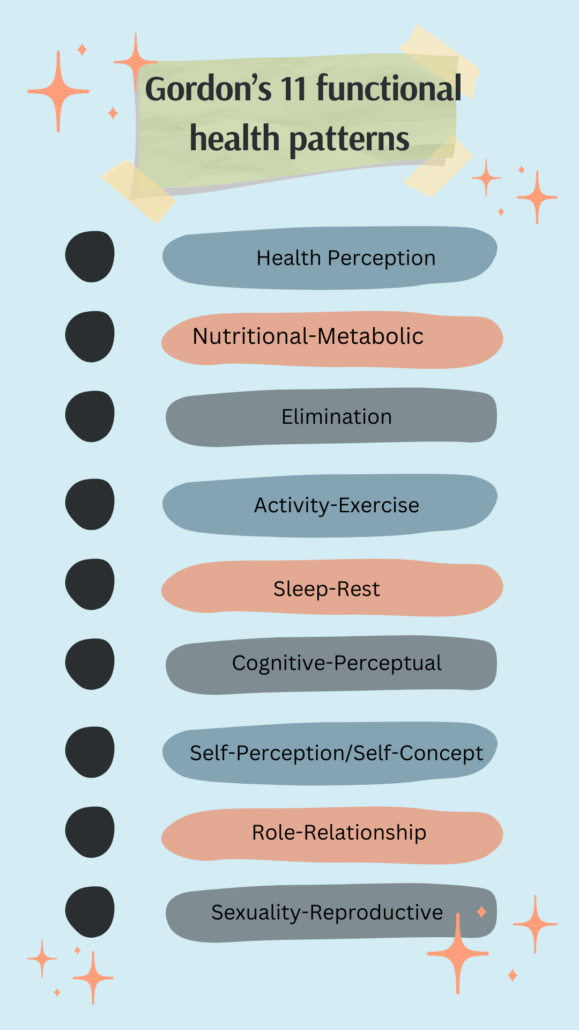
The theory defines 11 functional health patterns, organized into a standardized and universal format for ease of use.
Overview of Gordon’s Functional Health Patterns
When it comes to providing comprehensive and patient-centered care, nurses need a systematic approach to assessment that considers the whole person – their physical, psychological, and social needs.
This holistic perspective is at the heart of Gordon’s Functional Health Patterns, a widely recognized nursing model that serves as a valuable framework for assessment, diagnosis, and care planning.
What are Gordon’s functional health patterns? Definition
Developed by Marjory Gordon in the late 1970s, this model revolutionized the nursing process by introducing a novel concept: functional health patterns.
Unlike traditional medical models that focus solely on disease and dysfunction, Gordon’s approach emphasizes assessing an individual’s integrated patterns of behavior and their ability to meet basic human needs.
The 11 Functional Health Patterns At the core of Gordon’s model are eleven functional health patterns, each representing a crucial aspect of human functioning and well-being:
- Health Perception/Health Management
- Nutritional-Metabolic
- Elimination
- Activity-Exercise
- Sleep-Rest
- Cognitive-Perceptual
- Self-Perception/Self-Concept
- Role-Relationship
- Sexuality-Reproductive
- Coping-Stress Tolerance
- Value-Belief
These patterns are interconnected, and disturbances in one area can have ripple effects on others, underscoring the importance of a comprehensive assessment.
One vital aspect of Gordon’s model is its emphasis on culturally sensitive assessment.
- Gordon recognized that an individual’s functional health patterns are influenced by their cultural background, beliefs, and values.
- By incorporating cultural considerations into the assessment process, nurses can better understand their patients’ perspectives and tailor care plans accordingly.
The Nursing Process with Gordon’s Model Gordon’s Functional Health Patterns
The Nursing Process with Gordon’s Model Gordon’s Functional Health Patterns seamlessly integrates with the nursing process, providing a structured framework for the assessment, diagnosis, planning, implementation, and evaluation of care:
- Assessment: Nurses collect data on each functional health pattern to identify actual or potential problems, strengths, and areas of concern.
- Diagnosis: Based on the assessment findings, nurses formulate nursing diagnoses that capture the patient’s health status and needs.
- Planning: Individualized care plans are developed, addressing identified problems and promoting optimal health patterns.
- Implementation: Nursing interventions are carried out to address the patient’s needs and support their functional health patterns.
- Evaluation: Nurses continuously evaluate the effectiveness of the care plan and make necessary adjustments
Gordon’s functional health patterns checklist
Health Perception-Health Management Pattern
The health perception-health management pattern assesses an individual’s overall perception of their health status and their health management practices.
This pattern is crucial for understanding a patient’s health beliefs, attitudes, and behaviors, which can significantly influence their willingness to engage in health promotion activities and adhere to treatment plans.
Potential Questions for Nurses:
- How would you describe your current health status?
- What does being healthy mean to you?
- What steps do you take to maintain or improve your health?
- How do you manage any existing health conditions or concerns?
Potential Responses and Nursing Interventions:
- Nurses can reinforce and encourage these practices if a patient exhibits a positive health perception and engages in health-promoting behaviors.
- However, if a patient has a negative perception of their health or engages in risky behaviors, nurses may need education, counseling, and support to help them develop a more proactive approach to health management.
Example:
- A prospective randomized controlled study aimed to investigate the effect of the application of Gordon’s Functional Health Patterns (FHP) model in the nursing care of symptomatic heart failure (HF) patients on the quality of life.
- The study found that HF patients in the group receiving care developed based on Gordon’s FHP model were associated with significantly improved quality of life compared to the control group receiving standard nursing care.
Source: https://doi.org/10.1016/j.apnr.2020.151247
Nutritional-Metabolic Pattern
The nutritional-metabolic pattern focuses on assessing an individual’s dietary intake, eating habits, and metabolic processes.
This pattern is essential for identifying potential nutritional deficiencies or imbalances that may contribute to health problems or impede recovery.
Potential Questions for Nurses:
- Can you describe your typical daily food and fluid consumption?
- How does your food and fluid intake compare to your estimated metabolic needs?
- Do you have any dietary restrictions or preferences?
- Have you experienced any changes in your weight, appetite, or digestion?
Potential Responses and Nursing Interventions:
Based on the assessment findings, nurses may need to provide dietary counseling, recommend nutritional supplements, or collaborate with a dietitian to develop a personalized meal plan.
If a patient has specific metabolic disorders or conditions, such as diabetes or kidney disease, nurses can provide education and support to help manage these conditions through proper nutrition.
Example:
A quasi-experimental study was conducted to assess the effect of the application of Gordon’s FHP model on the nutritional-metabolic pattern in patients with chronic kidney disease.
The study found that patients in the intervention group, who received care based on Gordon’s model, had significantly improved dietary habits and better management of their nutritional needs compared to the control group receiving standard care.
source: https://pubmed.ncbi.nlm.nih.gov/32451005/
Elimination Pattern
The elimination pattern examines an individual’s ability to effectively excrete waste products from the body, including bowel and bladder function. This pattern is crucial for identifying potential issues such as constipation, incontinence, or other elimination problems that can impact overall health and well-being.
Potential Questions for Nurses:
- Can you describe your typical bowel and bladder habits?
- Have you experienced any changes in your elimination patterns?
- Do you have any difficulties or discomfort related to urination or bowel movements?
- Are you taking any medications or supplements that may affect your elimination?
Potential Responses and Nursing Interventions: If a patient reports irregular or problematic elimination patterns, nurses can provide education on proper hydration, fiber intake, and bowel and bladder management strategies. In some cases, nurses may need to implement interventions such as scheduled toileting, catheter care, or bowel retraining programs. Collaboration with a physician or specialist may be necessary for more complex elimination issues.
Example: A study conducted at a school of nursing aimed to investigate the effect of Gordon’s FHP model on the elimination pattern in hospitalized patients.
The study found that patients receiving care based on Gordon’s model had significantly improved bowel and bladder function compared to the control group receiving standard care. The model helped nurses identify and address elimination issues early, leading to better patient outcomes and reduced complications.
Source: https://ncbi.nlm.nih.gov/pmc/articles/PMC5791974/
Activity-Exercise Pattern
The activity-exercise pattern assesses an individual’s level of physical activity, exercise habits, and functional abilities related to activities of daily living (ADLs). This pattern is crucial for identifying potential limitations or barriers to maintaining an active lifestyle, which can impact overall health and well-being.
Potential Questions for Nurses:
- Can you describe your typical daily activities and exercise routines?
- Do you experience any difficulties or limitations in performing ADLs?
- Have you noticed any changes in your energy levels or physical abilities?
- What are your thoughts on the importance of physical activity for your health?
Potential Responses and Nursing Interventions:
Based on the assessment findings, nurses can provide education and guidance on appropriate exercise programs, energy conservation techniques, or assistive devices to support ADLs.
For patients with mobility limitations or chronic conditions, nurses may need to collaborate with physical therapists or occupational therapists to develop tailored rehabilitation or exercise plans.
Example: A randomized controlled trial was conducted to evaluate the effect of Gordon’s FHP model on the activity-exercise pattern in primary care patients.
The study found that patients in the intervention group, who received care based on Gordon’s model, had significantly improved physical activity levels and better functional abilities compared to the control group receiving standard care.
The model helped nurses identify and address barriers to physical activity, leading to improved health outcomes.
Source: https://doi.org/10.1016/j.apnr.2020.151247
Sleep-Rest Pattern
The sleep-rest pattern assesses an individual’s sleep habits, sleep quality, and ability to achieve restful and restorative sleep. This pattern is crucial for identifying potential sleep disturbances or disorders that can impact overall health, energy levels, and well-being.
Potential Questions for Nurses:
- Can you describe your typical sleep patterns and routines?
- Do you experience any difficulties falling or staying asleep?
- How rested do you feel upon waking up?
- Do you engage in any activities or practices to promote better sleep?
Responses and Nursing Interventions:
If a patient reports sleep disturbances or poor sleep quality, nurses can provide education on sleep hygiene practices, such as maintaining a consistent sleep schedule, creating a conducive sleep environment, and avoiding stimulants before bedtime.
For more persistent sleep issues, nurses may need to collaborate with a physician or sleep specialist to explore potential underlying causes and appropriate interventions, such as medication management or cognitive-behavioral therapy.
Example: A study was conducted to compare Gordon’s FHP model with other nursing models in addressing the sleep-rest pattern in hospitalized patients.
The study found that patients receiving care based on Gordon’s model had significantly improved sleep quality and reduced sleep disturbances compared to those receiving care based on other models.
The comprehensive assessment approach of Gordon’s model helped nurses identify and address factors contributing to poor sleep, leading to better patient outcomes.
[Source: https://doi.org/10.1016/j.apnr.2020.151247]
Cognitive-Perceptual Pattern
The cognitive-perceptual pattern assesses an individual’s cognitive abilities, such as memory, problem-solving, and decision-making, as well as their sensory perception.
This pattern is crucial for identifying potential cognitive impairments or sensory deficits that can impact an individual’s ability to understand and engage in their care.
Questions for Nurses:
- Have you experienced any changes in your memory, concentration, or ability to solve problems?
- Do you have any difficulties with your vision, hearing, taste, or smell?
- How do you typically process and understand health information provided to you?
- Are there any strategies or accommodations that help you better comprehend or remember information?
Responses and Nursing Interventions:
If a patient exhibits cognitive or perceptual impairments, nurses can provide education and support using appropriate communication techniques, such as simplifying information, using visual aids, or involving family members or caregivers.
In some cases, nurses may need to collaborate with specialists, such as occupational therapists or speech-language pathologists, to develop tailored interventions or assistive devices.
Example: A study aimed to investigate the effect of Gordon’s FHP model on the cognitive-perceptual pattern in patients with mild cognitive impairment.
The study found that patients receiving care based on Gordon’s model had significantly improved cognitive function and better engagement in their care compared to the control group receiving standard care.
The comprehensive assessment approach and tailored interventions based on Gordon’s model helped address cognitive and perceptual challenges, leading to improved patient outcomes and quality of life.
Self-Perception and Self-Concept Pattern
The self-perception and self-concept pattern assesses an individual’s self-esteem, body image, and overall sense of self-worth. This pattern is crucial for understanding an individual’s psychological well-being and identifying potential issues related to self-perception that may impact their health behaviours and coping strategies.
Potential Questions for Nurses:
- How would you describe your overall self-esteem and confidence?
- Are there any aspects of your appearance or body that you feel self-conscious about?
- How do you perceive yourself in relation to your roles and responsibilities?
- What factors or experiences have shaped your self-perception and self-concept?
Potential Responses and Nursing Interventions:
If a patient exhibits low self-esteem, negative body image, or a distorted self-concept, nurses can provide counseling, supportive interventions, and referrals to mental health professionals as needed.
For patients with chronic conditions or disabilities, nurses can help facilitate acceptance and adaptation by promoting positive self-perception and providing resources for support groups or counseling services.
Example:
A study was conducted to evaluate the effect of Gordon’s FHP model on self-perception and self-concept patterns in patients with chronic skin conditions. The study found that patients receiving care based on Gordon’s model had significantly improved self-esteem, body image, and overall self-perception compared to the control group receiving standard care.
The comprehensive assessment approach and tailored interventions based on Gordon’s model helped address the psychological and emotional aspects of living with chronic skin conditions, leading to improved quality of life and better coping strategies.
Role-Relationship Pattern
The role-relationship pattern examines an individual’s roles within their family, work, and social circles, as well as the quality of their relationships. This pattern is crucial for identifying potential sources of stress, support systems, or relationship dynamics that can impact an individual’s health and well-being.
Potential Questions for Nurses:
- Can you describe your various roles and responsibilities within your family, work, and social circles?
- How would you describe the quality of your relationships with significant others?
- Do you feel supported or burdened by your roles and relationships?
- Have there been any recent changes or challenges in your roles or relationships?
Potential Responses and Nursing Interventions:
If a patient reports significant role strain, relationship conflicts, or lack of social support, nurses can provide counseling, facilitate communication and conflict resolution strategies, and connect patients with appropriate support resources or services.
For patients facing major life transitions or role changes, nurses can help facilitate adjustment and coping strategies.
Example:
A study was conducted to assess the effect of Gordon’s FHP model on the role-relationship pattern in caregivers of patients with dementia.
The study found that caregivers receiving care based on Gordon’s model had significantly better coping strategies, reduced caregiver burden, and improved relationship quality compared to the control group receiving standard care.
The comprehensive assessment approach and tailored interventions based on Gordon’s model helped address the unique challenges and relationship dynamics faced by caregivers, leading to improved well-being and better care for their loved ones.
Sexuality-Reproductive Pattern
The sexuality-reproductive pattern encompasses not only reproductive health but also intimate relationships and sexual identity.
This pattern is crucial for addressing potential issues related to sexual function, fertility, or gender identity that can impact an individual’s overall well-being and quality of life.
Potential Questions for Nurses:
- Do you have any concerns or questions related to your sexual health or reproductive function?
- How would you describe the quality of your intimate relationships?
- Have you experienced any changes or challenges related to your sexual identity or expression?
- Are there any cultural or personal beliefs that influence your views on sexuality or reproduction?
Potential Responses and Nursing Interventions:
If a patient expresses concerns or issues related to their sexuality or reproductive health, nurses can provide education, counseling, and referrals to appropriate specialists or resources.
For patients facing fertility challenges or gender identity concerns, nurses can offer support, connect them with support groups, and advocate for their needs within the healthcare system.
Example: A study was conducted to evaluate the effect of Gordon’s FHP model on the sexuality-reproductive pattern in patients seeking fertility treatment.
The study found that patients receiving care based on Gordon’s model had significantly improved sexual and reproductive health outcomes, better-coping strategies, and higher satisfaction with their care compared to the control group receiving standard care.
The comprehensive assessment approach and tailored interventions based on Gordon’s model helped address the physical, emotional, and social aspects of fertility treatment, leading to a more holistic and supportive care experience.
Coping-Stress Tolerance Pattern
The coping-stress tolerance pattern evaluates an individual’s ability to manage and adapt to stressful situations, as well as their stress management techniques. This pattern is particularly relevant in today’s fast-paced and demanding world, where stress can contribute to various physical and mental health issues.
Potential Questions for Nurses:
- How would you describe your overall stress levels and ability to cope with stressful situations?
- What strategies or techniques do you use to manage stress?
- Have you experienced any major life stressors or traumatic events that have impacted your coping abilities?
- Do you have a support system or resources to help you cope with stress?
Potential Responses and Nursing Interventions:
If a patient exhibits poor coping strategies, high-stress levels, or has experienced significant life stressors, nurses can provide education on stress management techniques, such as relaxation exercises, mindfulness practices, or cognitive-behavioral strategies.
In some cases, nurses may need to collaborate with mental health professionals or refer patients to counseling services.
Value-Belief Pattern
The value-belief pattern explores an individual’s personal values, religious or spiritual beliefs, and cultural practices. This pattern is essential for providing culturally competent nursing care and fostering a respectful and inclusive healthcare environment.
Potential Questions for Nurses:
- What are your personal values and beliefs that are important to you?
- Do you have any religious or spiritual practices that influence your health perspectives or decisions?
- Do you want us to know or accommodate any cultural traditions or preferences?
- How do your values and beliefs influence your approach to health and healthcare?
Potential Responses and Nursing Interventions: By understanding a patient’s values, beliefs, and cultural background, nurses can tailor their care approach and interventions to align with the patient’s preferences and needs. This may involve accommodating cultural practices, providing education or resources respectful of the patient’s beliefs, or involving spiritual or cultural leaders in the care process.
Example: A study was conducted to evaluate the effect of Gordon’s FHP model on addressing the value-belief pattern in a culturally diverse patient population.
The study found that patients receiving care based on Gordon’s model had significantly higher satisfaction with their care, better adherence to treatment plans, and improved health outcomes compared to the control group receiving standard care.
The comprehensive assessment approach and tailored interventions based on Gordon’s model helped nurses provide culturally sensitive and respectful care, leading to better patient engagement and overall health and well-being.
Assessment of functional health patterns
The functional health patterns model serves as a standard for nursing practice, guiding comprehensive patient assessment, data collection, and the development of individualized care plans.
Assessment using Gordon’s functional health patterns involves a thorough evaluation of each pattern, considering factors that influence an individual’s level of health, health status, and overall health and well-being.
This assessment process incorporates various assessment tools, such as
- health history
- questions asked,
- observations of health practices and daily activities.
For example, in the nursing care of symptomatic heart failure patients, Gordon’s functional health patterns model can be applied to assess the patient’s nutritional-metabolic pattern, including their pattern of food and fluid consumption relative to metabolic needs. This assessment can inform nursing interventions related to dietary modifications and fluid management.
Similarly, the model can be used to evaluate the activity and exercise pattern in primary care settings, identifying barriers to physical activity and developing tailored exercise plans to promote overall health.
Several studies have investigated the effect of application of Gordon’s functional health patterns model in various healthcare settings and patient populations.
- A prospective randomized controlled study conducted at a school of nursing aimed to investigate the effect of Gordon’s FHP model on the quality of life of symptomatic heart failure patients.
- The study found that HF patients receiving nursing care developed based on Gordon’s model were associated with significantly improved quality of life compared to the control group receiving standard nursing care.
- Another randomized controlled trial explored the comparison of Gordon’s functional health patterns model with other nursing models in addressing the cognitive-perceptual pattern.
- The study revealed that patients receiving care based on Gordon’s model had better cognitive function and engagement in their care, highlighting the model’s effectiveness in addressing various aspects of health.
- A quasi-experimental study assessed the impact of Gordon’s model on the coping-stress tolerance pattern in patients with chronic conditions.
- The findings indicated that patients receiving care based on Gordon’s model exhibited improved coping strategies and reduced stress levels, underscoring the model’s value in addressing psychological and emotional well-being.
The assessment of functional health patterns using Gordon’s model is recognized by the North American Nursing Diagnosis Association (NANDA) as a method for comprehensive nursing assessment and care planning.
By incorporating this model into nursing education and practice, healthcare professionals can provide patient-centered care that addresses the multidimensional nature of health and promotes overall well-being.
Importance of the Functional Health Patterns in Nursing Practice:
Functional health patterns are widely used in nursing for data collection, analysis, and documentation. The assessment provides an in-depth understanding of an individual’s health status, which is crucial for formulating an appropriate nursing diagnosis and care plan. Using functional health patterns, nurses can identify health problems, prioritize nursing interventions, and monitor patient outcomes.
The data collected is then organized and analyzed using the 11 functional health patterns, which provide a comprehensive and holistic picture of the patient’s health status.
The functional health patterns framework provides a structured approach to nursing assessment, helping to ensure that all aspects of a patient’s health are considered.
The assessment process involves gathering data from the patient, including their health history, physical examination, and self-reported health behaviors and practices.
Importance of Using Gordon’s Functional Health Patterns
- Enhancing Nursing Assessment – Using the functional health patterns framework, nurses can ensure that all aspects of a patient’s health are considered and addressed in the assessment process. This comprehensive approach to assessment leads to improved accuracy and reliability of the data collected and helps identify health problems and priorities for nursing interventions.
- Improving Patient Outcomes – Using the functional health patterns framework in nursing has improved patient outcomes by providing a patient-centered approach to care. By focusing on the patient’s health behaviors and practices, nurses can identify and address health problems early, leading to improved health outcomes and decreased healthcare utilization.
- Enhancing Interdisciplinary Collaboration – The functional health patterns framework can also improve interdisciplinary collaboration in healthcare by providing a common language and framework for health assessment and patient care planning. This enhanced collaboration improves communication and care coordination, ultimately benefiting the patient.
- Supporting Evidence-Based Practice – The functional health patterns framework promotes evidence-based practice in nursing using a structured and systematic approach to assessment. The data collected and analyzed using the framework can inform nursing interventions and develop best practices in nursing care.
Limitations of Gordon’s Functional Health Patterns
Despite these limitations, Gordon’s Functional Health Patterns model remains a valuable and widely used framework for holistic nursing assessment and care planning.
However, ongoing evaluation, adaptation, and integration with other evidence-based practices may be necessary to address its limitations and enhance its effectiveness in various healthcare settings and populations.
Gordon’s Functional Health Patterns model, while widely recognized and used in nursing practice, has certain limitations that should be considered:
- Lack of prioritization: The model presents all 11 patterns as equally important, but it does not provide guidance on how to prioritize assessments or interventions when time or resources are limited. This can be challenging in acute care settings or situations requiring rapid decision-making.
- Limited applicability in certain populations: While the model aims to be comprehensive, its applicability may be limited in certain patient populations, such as critically ill patients, individuals with cognitive impairments, or those with specific medical conditions or disabilities. Some patterns may be less relevant or require modification in these contexts.
- Limited Cultural Relevance – One criticism of Gordon’s functional health patterns is that they are irrelevant to all cultures and populations. Some aspects of the model, such as focusing on Western health beliefs and practices, may only apply to some diverse cultural groups. This can limit the effectiveness of the assessment and lead to inaccurate data collection and analysis.
- Lack of evidence-based validation: While the model is widely used and accepted, there is a relative lack of robust, evidence-based research validating its efficacy and outcomes compared to other nursing assessment models or frameworks.
- Subjectivity in interpretation: The assessment and interpretation of functional health patterns can be subjective and may vary among different nurses or healthcare providers. This subjectivity can lead to inconsistencies in the identification of nursing diagnoses and the development of care plans.
- Potential overlap among patterns: Some patterns may overlap or have redundant elements, leading to duplication of assessment efforts and data collection. For example, aspects of the self-perception pattern may overlap with the coping-stress tolerance pattern or the role-relationship pattern.
- Time-consuming nature: Assessing all 11 patterns in depth can be time-consuming and may not be practical in certain healthcare settings with limited resources or time constraints.
- Limited guidance on pattern interrelationships: While Gordon recognized the interrelationships among the patterns, the model does not provide specific guidance on how to assess or address these interrelationships in a systematic manner.
- Lack of integration with standardized nursing terminologies: The model does not directly incorporate or align with standardized nursing terminologies, such as NANDA-I, NIC, and NOC, which are widely used in nursing documentation and care planning.
- Lack of Integration with Other Theories – Another criticism is that the functional health patterns framework needs to be better integrated with other theories in nursing and healthcare. This can limit its effectiveness as a tool for guiding nursing practice and may result in a fragmented approach to patient care.
Criticism of the 11 Patterns Functional Health Patterns
There has also been criticism of the 11 patterns themselves, particularly regarding the categorization and organization of the patterns.
Some argue that the patterns are too broad and need to be more specific to capture all aspects of health and that the assessment process may overlook essential health behaviors and practices.
While Gordon’s Functional Health Patterns model has been widely adopted and used in nursing practice, it has also received some criticism and scrutiny over the years. Here are some potential criticisms or limitations of the model:
- Complexity and Time-Consuming: The comprehensive nature of assessing all 11 patterns can be time-consuming and may not be practical in certain healthcare settings, especially those with limited resources or time constraints. Some nurses may find the model overwhelming or too complex to implement effectively.
- Overlapping Patterns: There is potential overlap or redundancy among some of the patterns, which can lead to duplication of assessment efforts and data collection. For example, aspects of the self-perception pattern may overlap with the coping-stress tolerance pattern or the role-relationship pattern.
- Cultural Considerations: While Gordon emphasized the importance of considering cultural factors, some critics argue that the model does not provide sufficient guidance or frameworks for addressing cultural diversity and incorporating culturally sensitive assessments and interventions.
- Limited Application in Specific Populations: The model may not be as applicable or suitable for certain populations, such as critically ill patients, individuals with specific disorders or disabilities, or those in acute care settings. Some patterns may be less relevant or require modification in these contexts.
- Subjectivity and Interpretation: The assessment and interpretation of functional health patterns can be subjective and may vary among different nurses or healthcare providers. This subjectivity can lead to inconsistencies in the identification of nursing diagnoses and the development of care plans.
- Limited Evidence-Based Support: While the model is widely used, some critics argue that there is a lack of robust, evidence-based research supporting the efficacy and outcomes of using Gordon’s Functional Health Patterns compared to other nursing assessment models or frameworks.
- Need for Ongoing Training and Education: Effective implementation of the model requires ongoing training and education for nurses to ensure a consistent understanding and application of the patterns and assessment criteria. This can be a challenge in healthcare settings with high staff turnover or limited resources for professional development.
Despite these criticisms, many nurses and nursing educators continue to find value in Gordon’s Functional Health Patterns model as a comprehensive and holistic approach to patient assessment and care planning. However, ongoing evaluation, adaptation, and evidence-based refinement of the model may be necessary to address its limitations and enhance its effectiveness in various healthcare settings and populations.
Gordon’s Functional Health Patterns Nursing diagnosis
Gordon’s Functional Health Patterns provide a comprehensive framework for assessing a patient’s health and identifying potential nursing diagnoses across various domains. Here are some key points about nursing diagnoses related to the 11 functional health patterns:
- Health Perception-Health Management Pattern: This pattern can lead to nursing diagnoses related to health behaviors, adherence to therapeutic regimens, and risk factors. Examples include Ineffective Health Maintenance, Ineffective Therapeutic Regimen Management, Risk-Prone Health Behavior, and Readiness for Enhanced Therapeutic Regimen Management.
- Nutritional-Metabolic Pattern: Assessments in this pattern can identify nursing diagnoses related to nutritional imbalances, fluid and electrolyte disturbances, and metabolic disorders. Examples include Imbalanced Nutrition: Less Than Body Requirements, Deficient Fluid Volume, Risk for Unstable Blood Glucose, and Impaired Tissue Integrity.
- Elimination Pattern: Evaluations of elimination patterns can lead to nursing diagnoses related to bowel and bladder function, such as Constipation, Diarrhea, Urge Urinary Incontinence, and Risk for Constipation.
- Activity-Exercise Pattern: Assessments in this pattern may reveal nursing diagnoses related to physical mobility, energy levels, and respiratory function, such as Impaired Physical Mobility, Activity Intolerance, Ineffective Breathing Pattern, and Risk for discharge syndrome.
- Sleep-Rest Pattern: Disturbances in sleep patterns can result in nursing diagnoses like Insomnia and Sleep Deprivation.
- Cognitive-Perceptual Pattern: This pattern may identify nursing diagnoses related to cognitive impairments, sensory deficits, and pain management, such as Acute Confusion, Chronic Pain, and Disturbed Sensory Perception.
- Self-Perception-Self-Concept Pattern: Assessments in this pattern can lead to nursing diagnoses related to self-esteem, body image, and emotional well-being, such as Disturbed Body Image, Situational Low Self-Esteem, and Risk for Loneliness.
- Role-Relationship Pattern: Evaluations of roles and relationships may reveal nursing diagnoses like Caregiver Role Strain, Impaired Social Interaction, and Risk for Complicated Grieving.
- Sexuality-Reproductive Pattern: This pattern can identify nursing diagnoses related to sexual health and reproductive concerns, such as Sexual Dysfunction and Ineffective Sexuality Patterns.
- Coping-Stress Tolerance Pattern: Assessments in this pattern may identify nursing diagnoses related to stress management and coping abilities, such as Ineffective Coping, Stress Overload, and Risk for Post-Trauma Syndrome.
- Value-Belief Pattern: Evaluations of values and beliefs can lead to nursing diagnoses like Impaired Religiosity, Spiritual Distress, and Risk for Spiritual Distress.
By thoroughly assessing each of the 11 functional health patterns, nurses can identify actual or potential nursing diagnoses that encompass the patient’s physical, psychological, social, and spiritual well-being. These diagnoses then guide the development of individualized nursing care plans to address the patient’s specific needs and promote overall health and well-being.
Gordon’s functional health patterns sample questions
Here are some sample questions that nurses could ask patients when assessing each of Gordon’s 11 functional health patterns:
- Health Perception-Health Management Pattern:
– How would you describe your current health status?
– What does being healthy mean to you?
– What steps do you take to maintain or improve your health?
– How do you manage any existing health conditions or concerns? - Nutritional-Metabolic Pattern:
– Can you describe your typical daily food and fluid intake?
– Have you experienced any changes in your weight, appetite, or digestion?
– Do you have any dietary restrictions or preferences?
– Are you taking any supplements or vitamins? - Elimination Pattern:
– Can you describe your typical bowel and bladder habits?
– Have you noticed any changes in your elimination patterns?
– Do you experience any difficulties or discomfort related to urination or bowel movements?
– Are you taking any medications that may affect your elimination? - Activity-Exercise Pattern:
– Can you describe your typical daily activities and exercise routines?
– Do you experience any difficulties or limitations in performing daily activities?
– Have you noticed any changes in your energy levels or physical abilities?
– What are your thoughts on the importance of physical activity for your health? - Sleep-Rest Pattern:
– Can you describe your typical sleep patterns and routines?
– Do you experience any difficulties falling or staying asleep?
– How rested do you feel upon waking up?
– Do you engage in any activities or practices to promote better sleep? - Cognitive-Perceptual Pattern:
– Have you experienced any changes in your memory, concentration, or ability to solve problems?
– Do you have any difficulties with your vision, hearing, taste, or smell?
– How do you typically process and understand health information provided to you?
– Are there any strategies or accommodations that help you better comprehend or remember information? - Self-Perception and Self-Concept Pattern:
– How would you describe your overall self-esteem and confidence?
– Are there any aspects of your appearance or body that you feel self-conscious about?
– How do you perceive yourself in relation to your roles and responsibilities?
– What factors or experiences have shaped your self-perception and self-concept? - Role-Relationship Pattern:
– Can you describe your various roles and responsibilities within your family, work, and social circles?
– How would you describe the quality of your relationships with significant others?
– Do you feel supported or burdened by your roles and relationships?
– Have there been any recent changes or challenges in your roles or relationships? - Sexuality-Reproductive Pattern:
– Do you have any concerns or questions related to your sexual health or reproductive function?
– How would you describe the quality of your intimate relationships?
– Have you experienced any changes or challenges related to your sexual identity or expression?
– Are there any cultural or personal beliefs that influence your views on sexuality or reproduction? - Coping-Stress Tolerance Pattern:
– How would you describe your overall stress levels and ability to cope with stressful situations?
– What strategies or techniques do you use to manage stress?
– Have you experienced any major life stressors or traumatic events that have impacted your coping abilities?
– Do you have a support system or resources to help you cope with stress? - Value-Belief Pattern:
– What are your personal values and beliefs that are important to you?
– Do you have any religious or spiritual practices that influence your health perspectives or decisions?
– Are there any cultural traditions or preferences that you would like us to be aware of or accommodate?
– How do your values and beliefs influence your approach to health and healthcare?
These sample questions can help nurses gather relevant information about each functional health pattern and identify potential areas of concern or strengths that may impact the patient’s overall health and well-being.
Gordon’s functional health patterns Example
Gordon’s functional health patterns Example 2
Gordon’s functional Health Patterns pdf – Family Health Assessment Questionnaire
Gordon’s 11 functional health patterns sample
Gordon’s Functional Health Patterns Case Study
The functional health patterns framework developed by M. Gordon provides a comprehensive and systematic approach to nursing assessment and health promotion.
Despite some criticisms and limitations, the model continues to be widely used in nursing practice and has significantly impacted the field of nursing.
The functional health patterns provide a holistic approach to health assessment and promote a patient-centered approach to care.
By using the framework, nurses can identify health problems, prioritize nursing interventions, and monitor patient outcomes, leading to improved patient care and outcomes.
The functional health patterns framework continues to evolve and be refined, and future directions for the theory may include increased cultural relevance and integration with other nursing and healthcare theories.
This will further enhance the framework’s usefulness as a tool for nursing practice and improve patient outcomes.
Gordon’s 11 Functional Health Patterns FAQ
What is Gordon’s approach to nursing?
Gordon’s approach to nursing revolves around the concept of functional health patterns. It is a model and standard in nursing care that helps in comprehensive health assessment, nursing diagnosis, and effective nursing care for patients.
How many health patterns are included in Gordon’s model?
Gordon’s model includes a total of 11 functional health patterns. These patterns cover various aspects of an individual’s health and well-being, providing a holistic approach to nursing care. They include;
Health Perception/Health Management
Nutritional-Metabolic
Elimination
Activity-Exercise
Sleep-Rest
Cognitive-Perceptual
Self-Perception/Self-Concept
Role-Relationship
Sexuality-Reproductive
Coping-Stress Tolerance
Value-Belief
What is the purpose of the functional health pattern?
The purpose of functional health patterns is to help healthcare professionals assess and interpret a patient’s health status systematically. It aids in identifying areas that need attention and potential nursing interventions to promote health and manage illness effectively.
How many functional patterns are there according to Gordon?
According to Gordon’s model, 11 functional health patterns are essential for a comprehensive health assessment and nursing care delivery. These patterns cover a wide range of aspects from health perception to coping-stress tolerance.
