Week 4: Schizophrenia: Psychosocial and Biological Treatments (Health Disorders)
Schizophrenia
The diagnostic criteria for schizophrenia include delusions, hallucinations, incoherence, and individual disorganization presenting within a month (American Psychiatric Association [APA], 2019). An individual must present at least one or two primary symptoms, i.e., hallucinations, delusions, or incoherence. The individual must have a marked decline in functioning in one or more significant areas compared to their previous level of functioning. The symptoms must persist for at least six months when an individual experiences one or more active symptoms (Health Disorders).
The symptoms must not be attributed to schizoaffective, depressive, or bipolar disorders, substance abuse, or medical conditions. Schizophrenia diagnosis occurs with prominent hallucinations or delusions with a childhood history of communication or spectrum disorder (APA, 2019). The condition’s cause remain specified as the first, multiple, or continuous episodes, and severity assessed using a 5-point scale. The specifier “with catatonia” remain added if catatonia is present. These symptoms must cause significant distress or affect functioning in critical areas. The condition should not remain associated with another medical condition or substance use (Health Disorders).
Antipsychotic medications remain a recommendation for schizophrenia treatment. In this case, Aripiprazole is an evidence-based antipsychotic medication recommended for Schizophrenia (Ribeiro et al., 2018). The safety profile is better compared with other typical and atypical antipsychotic drugs. Antipsychotic medications cause the risk of significant side effects such as tardive dyskinesia.
Hence, recommended to administer the lowest possible dosage of the antipsychotic medications and prescription done cautiously for children and the elderly. In addition, patients experiencing mood disorders (Boland & Verduin, 2021). Regular evaluation of patients taking antipsychotic medication and consideration of medication alternatives are all recommended to minimize side effects (Health Disorders).
Psychotherapy remains essential to schizophrenia treatment, and a combination of pharmacological and psychotherapy remain associated with better health outcomes. Cognitive behavioral therapy (CBT) can effectively treat schizophrenia symptoms, including cognitive distortions, judgemental errors, and distractibility (Boland & Verduin, 2021). Shukla et al. (2021) showed that cognitive behavioral therapy effectively treats auditory hallucinations and cognitive impairments among schizophrenia patients.
References
American Psychiatric Association (APA). (2019). Diagnostic and statistical manual of mental disorders (DSM-5®). American Psychiatric Publishing
Ribeiro, E. L. A., de Mendonça Lima, T., Vieira, M. E. B., Storpirtis, S., & Aguiar, P. M. (2018). Efficacy and safety of Aripiprazole for treating schizophrenia: an overview of systematic reviews. European Journal of Clinical Pharmacology, 74(10), 1215-1233. https://doi.org/10.1007/s00228-018-2498-1
Week 5 Discussions: Diagnostic Criteria for Major Depressive Disorder and Bipolar Disorder
Major Depressive Disorder
The diagnostic criteria for MDD include five or more symptoms presenting within two weeks, characterized by loss of interest in activities or depressed mood. These symptoms include depressed mood, reduced pleasure or interest in activities, unintentional changes in weight or appetite, hypersomnia/insomnia, psychomotor agitation/retardation, fatigue/weakness, excessive guilt/worthlessness, flawed thinking/concentration, and suicide ideation/recurrent thoughts of death (APA, 2019)(Health Disorders).
These symptoms must cause significant distress or affect functioning in important areas. The condition should not be associated with another medical condition or substance use. Careful consideration of the presence of a major depressive episode remain vital in cases of a normal response to a significant loss. A manic or hypomanic episode must not have occurred, and the disorder cannot be better explained by a psychotic disorder (Health Disorders).
Bipolar Disorders
Bipolar I Disorder (BD-I)
The diagnostic criteria for BD-I include the experience of at least one manic episode followed by a major depressive or hypomanic episode. The episode must have lasted for at least one week and involved persistently irritable or elevated mood, increased energy, and three or more additional symptoms, such as racing thoughts, bloated self-esteem, sleeplessness, distractibility, talkativeness, or excessive involvement in potentially harmful activities (APA, 2019) (Health Disorders).
A hypomanic episode remain characterized by typical irritability, elevated mood, and increased energy or activity for at least four successive days. Individuals must have experienced at least three symptoms: overblown self-esteem, distractibility, sleeplessness, talkativeness, racing thoughts, increased goal-directed activity, or engagement in harmful/painful activities (APA, 2019). The changes in behavior remain observable by others with a marked need for hospitalization or impairment and cannot be attributed to substance abuse or other medical conditions.
A major depressive episode remain characterized by at least five symptoms showing a change in previous functioning for at least two weeks. These symptoms include depressed feelings or loss of pleasure in pursuing activities, hypersomnia or insomnia, significant weight loss/gain, psychomotor retardation/agitation, general weakness, worthlessness/excessive guilt, difficulty concentrating/thinking, or persistent suicide ideation and thoughts of death (APA, 2019) (Health Disorders).
Bipolar II Disorder(BD-II)
The diagnostic criteria for BD-I include a presentation of at least one hypomanic episode and one major depressive episode with similar symptoms and presentations as in BD-I. An individual must not have a history of manic episodes, and other mental health disorders cannot explain symptoms (Health Disorders).
Cyclothymic Disorder
The diagnostic criteria for cyclothymic include the experience of hypomanic and depressive symptoms that occur over two years. For children and adolescents, the symptoms must present for at least one year. Consequently, these symptoms should not meet the diagnostic criteria for depressive or hypomanic episodes, respectively (Boland & Verduin, 2021). Individuals must experience depressive and hypomanic symptoms for at least half the one or two-year period. The signs should not meet the diagnostic criteria for manic, hypomanic, or depressive symptoms and are not better explained by other schizophrenia and related disorders or attributed to substance abuse or medical conditions.
References
American Psychiatric Association (APA). (2019). Diagnostic and statistical manual of mental disorders (DSM-5®). American Psychiatric Publishing
Boland, R., & Verduin, M. (2021). Kaplan & Sadock’s Concise Textbook of Clinical Psychiatry. Lippincott Williams & Wilkins.
Week 6 Discussions: Psychosocial and Biological Treatments for Major Depressive Disorder and Bipolar Disorders
Major Depressive Disorder
The American Association of Child and Adolescent Psychiatry (AACAP) recommends various evidence-based treatments for children and adolescents diagnosed with MDD. Consequently, the recommended evidence-based treatment recommendations include supportive and psychoeducation interventions. Furthermore,combining CBT and pharmacology is optimal for youth presenting recurrent depressive symptoms. In addition, moderate to severe depression with suicide ideation, significant impairment, or psychosis (Boland & Verduin, 2021) (Health Disorders).
An example of an evidence-based treatment is the combination of Fluoxetine and CBT. Liu et al. (2022) demonstrated that combining Fluoxetine and CBT is effective in treating MDD symptoms compared to medication or CBT alone, with improved depressive symptoms, suicide ideation, and reduced recurrence. Moreover, the combination of Fluoxetine and CBT has a higher safety profile, with reduced adverse reactions. Subsequently, the combination reduces suicide ideation and prevents treatment-related emergence (Health Disorders).
Bipolar Disorders
The first-line treatment for bipolar disorder is monotherapy, recommended for acute and maintenance phases. Consequently, Lithium monotherapy is an effective and safe medication for treating acute mania and mood episodes in children and adolescents diagnosed with bipolar disorder (Amerio et al., 2018). Lithium monotherapy also prevents short-term and long-term relapse in adults (Volkmann et al., 2020) (Health Disorders).

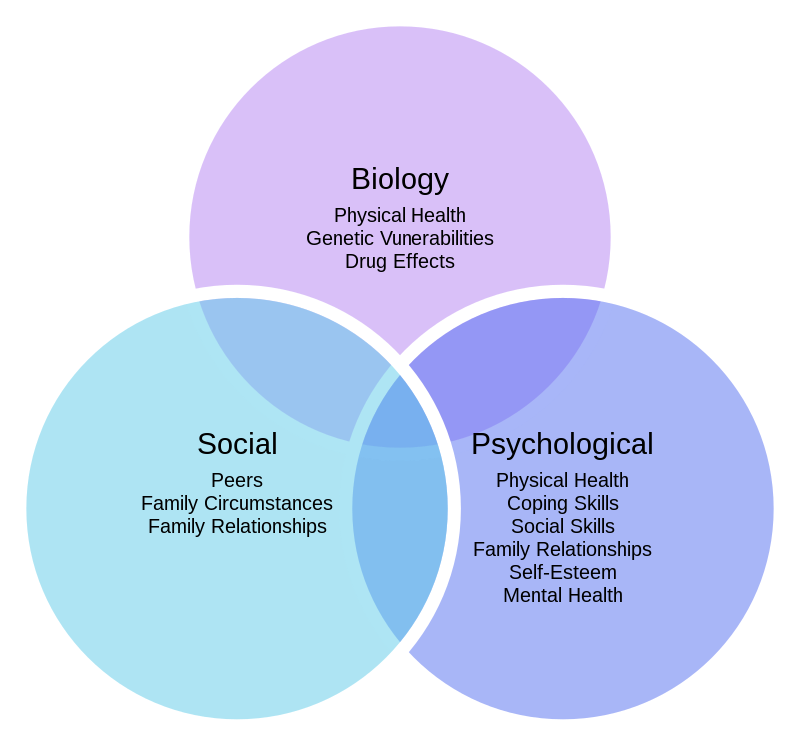
Cognitive behavioral therapy is the recommended psychosocial therapy based on the individual’s biological vulnerability, i.e., stressful interactions and skills deficits, limiting the ability to manage symptoms (Boland & Verduin, 2021). Consequently, Novick & and Swartz (2019) showed that CBT effectively reduces bipolar symptoms and relapse rates among individuals diagnosed with bipolar I and II.
Moreover, CBT helps individuals identify and challenge negative thoughts that influence treatment adherence, engagement in rewarding activities, and stability. CBT is also effective in promoting communication skills among affected individuals (Health Disorders).
Week 7: Diagnostic Criteria for Personality Disorders
Personality disorders
Personality disorders are a group of disorders associated with a persistent pattern of intrinsic experiences and external behavior. More so, that markedly deviates from the cultural expectations of an individual, with onset during adolescence or early adulthood (APA, 2019). Consequently, personality disorders include paranoid, schizoid, schizotypal, antisocial, borderline, histrionic, narcissistic, avoidant, dependent, and obsessive-compulsive personality disorders. Moreover, the DSM-5 provides specific criteria for diagnosing types of personality disorders (Health Disorders).
However, symptoms presented by an individual are not often limited to a particular personality disorder since symptoms tend to overlap. Consequently, symptoms of personality disorders can occur during the episode of another personality disorder. Therefore, a personality disorder diagnosis should be given only when the symptoms affect long-term functioning and are not limited to episodes of another psychiatric disorder, including substance abuse, head trauma, and medical conditions.
Generally, the diagnostic criteria for personality disorders include a persistent pattern of intrinsic experiences and external behavior. More so, that markedly deviates from the cultural expectations of an individual with onset during adolescence or early adulthood (Boland & Verduin, 2021). Moreover, the behavior has a fixed pattern affecting mood and affect, cognitive and perceptual, behavioral and interpersonal domains. Consequently, Individuals manifest the pattern in two or more areas, including impulse control, affectivity, cognition, and interpersonal functioning (Boland & Verduin, 2021) (Health Disorders).
The persistent pattern is pervasive and inflexible across various social and personal situations. Furthermore, the persistent pattern remain stable for an extended period, and the onset retraced to adolescence or early childhood. Subsequently, these symptoms must cause significant distress or affect functioning in essential areas, leading to maladaptive behavior. The condition should not be associated with another medical condition, head trauma, or substance use.
References
American Psychiatric Association (APA). (2019). Diagnostic and statistical manual of mental disorders (DSM-5®). American Psychiatric Publishing
Boland, R., & Verduin, M. (2021). Kaplan & Sadock’s Concise Textbook of Clinical Psychiatry. Lippincott Williams & Wilkins.
Week 8: Treatments for Personality Disorders
Treatment of personality disorders is relatively challenging, considering individuals are often unaware of their condition and seldom seek help. Psychotherapy is the primary treatment of individuals with personality disorders. Psychotherapy promotes character maturation and encourages patients to develop better adaptive solutions (Boland & Verduin, 2021). However, psychotherapy is challenging to implement with individuals presenting self-destructive and risky behaviors, necessitating pharmacological intervention that targets specific symptoms to allow individuals to participate in psychotherapeutic approaches (Health Disorders).
An example of psychotherapy for personality disorders is dialectical behavior therapy (DBT). Heerebrand et al. (2021) showed that DBT reduces symptoms of bipolar disorder, depression, and psychological distress. DBT uses cognitive, supportive, and behavioral skills training to help individuals understand and manage their behavior. DBT can be delivered in person or remotely, individually or in a group, to reduce self-destructive behavior and improve interpersonal skills based on the assumption that every behavior is learned and patients can reinforce or reward their maladaptive behavior.
However, a combination of psychotherapy and pharmacotherapy is recommended for effective treatment. In clients presenting maladaptive behaviors, implementing psychotherapy alone is challenging as clients present self-destructive behaviors, unstable effects, or risky behaviors (Boland & Verduin, 2021). Consequently, pharmacotherapy interventions are recommended to achieve prompt control of a client’s behavior and affect. Pharmacological interventions improve symptomology allowing seamless implementation of psychotherapy (Health Disorders).
Examples of recommended pharmacological interventions include selective serotonin reuptake inhibitors, serotonin-norepinephrine reuptake inhibitors, monoamine oxidase inhibitors, lithium, beta-blockers, psychotics, and antipsychotics (Boland & Verduin, 2021). These medications target specific symptoms of personality disorders allowing clients to undergo psychotherapy (Health Disorders).
References
Boland, R., & Verduin, M. (2021). Kaplan & Sadock’s Concise Textbook of Clinical Psychiatry. Lippincott Williams & Wilkins.
Heerebrand, S. L., Bray, J., Ulbrich, C., Roberts, R. M., & Edwards, S. (2021). Effectiveness of dialectical behavior therapy skills training group for adults with a borderline personality disorder. Journal of Clinical Psychology, 77(7), 1573-1590. https://doi.org/10.1002/jclp.23134
A Page will cost you $12, however, this varies with your deadline.
We have a team of expert nursing writers ready to help with your nursing assignments. They will save you time, and improve your grades.
Whatever your goals are, expect plagiarism-free works, on-time delivery, and 24/7 support from us.
Here is your 15% off to get started.
Simply:
- Place your order (Place Order)
- Click on Enter Promo Code after adding your instructions
- Insert your code – Get20
All the Best,
Cathy, CS


