Virginia Henderson Nursing Theory Explained: A Student Nurse’s Guide to the Needs Theory and 14 Basic Needs
Virginia Henderson’s nursing theory remains one of the most influential frameworks in modern nursing education and practice. Built on the understanding that nursing is centered on meeting the fundamental needs of individuals, her work offers a clear structure for both student nurses and experienced professionals seeking to provide holistic and patient-centered care. Much like how clinical guidelines shape the delivery of evidence-based practice, Henderson’s approach provides nurses with a conceptual foundation to evaluate patient needs, plan interventions, and promote independence wherever possible.
At its core, Henderson’s needs theory emphasizes the importance of addressing both physiological and psychological dimensions of health. By focusing on what patients require to achieve well-being—or to experience a peaceful death when recovery is not possible—her theory highlights the unique function of the nurse: to assist individuals in performing activities essential to life and recovery when they lack the strength, knowledge, or will to do so independently. This makes her framework both practical and adaptable across diverse healthcare settings.
For nursing students, understanding Henderson’s theory is more than an academic exercise; it is a guide to developing professional judgment and applying the nursing process in real-world scenarios. Whether in acute care, community health, or long-term care environments, the framework underscores how structured assessments and interventions can lead to improved health outcomes. It also reinforces the idea that nursing is not limited to tasks but is deeply rooted in the nature of nursing—the responsibility to respond to human needs with knowledge, skill, and compassion.
This article provides a comprehensive exploration of Virginia Henderson’s contribution to nursing theories, including her definition of nursing, the 14 basic needs central to her framework, and the strategies for applying her concepts in nursing practice. It will also discuss the challenges student nurses may encounter and how these can be addressed through education, mentorship, and reflective learning. By engaging with Henderson’s work, student nurses can strengthen their ability to provide safe, effective, and empathetic care—while building a solid foundation for their professional development.
What is Virginia Henderson Nursing Theory?
Virginia Henderson’s nursing theory, commonly referred to as the Needs Theory, is one of the most widely recognized nursing theories for guiding both clinical care and education. The framework is grounded in the belief that the primary role of the nurse is to support individuals in meeting their essential health requirements until they can regain independence. The theory identifies the 14 basic needs of human beings and links them directly to the nursing process, making it a practical model that can be applied to a range of patient populations and clinical environments. Unlike abstract approaches, Henderson’s theory was deliberately designed to reflect the nature of nursing in everyday practice, ensuring that it could be used to organize assessments, structure care plans, and measure outcomes.
The core of this framework is the unique function of the nurse, which Henderson described as assisting individuals—sick or well—in performing activities that contribute to health, recovery, or a peaceful death. These activities are the foundation of basic nursing care, and they recognize that illness, injury, or lack of knowledge can prevent patients from meeting their own human needs. Henderson emphasized that the goal of nursing is not only to restore health but also to help patients maintain dignity and independence whenever possible. This holistic perspective is one reason the model remains highly relevant in both nursing education and advanced nursing practice.
For example, in a rehabilitation ward, a patient recovering from a stroke may lack the ability to eat independently. Guided by Henderson’s nursing need theory, the nurse first identifies this unmet need, then assists with feeding while also teaching strategies to adapt to mobility limitations. This dual approach—assisting while promoting independence—reflects Henderson’s insistence that nursing should not foster dependence but should instead support recovery and adaptation.
Who was Virginia Henderson?
Virginia Henderson was a pioneering nurse theorist who developed her ideas through decades of teaching, research, and writing. She graduated with a diploma in nursing from the Army School of Nursing at Walter Reed Hospital in 1921, an experience that exposed her to both military and civilian health challenges. Later, she pursued higher education at Teachers College at Columbia University, where she earned her bachelor’s and master’s degrees and started teaching nursing. Henderson also worked with the Yale University School of Nursing, where she served as a research associate, contributing significantly to nursing scholarship. She was instrumental in compiling the Nursing Studies Index, an ambitious effort to organize existing literature that eventually became a cornerstone for research in the nursing profession.
Henderson authored and revised major texts, including Principles and Practice of Nursing, which helped shape curricula in nursing schools across the United States and abroad. Her influence was recognized internationally, earning her the title “the first lady of nursing.” She also collaborated with the International Council of Nurses, helping to expand nursing standards globally. Henderson’s legacy endures through her conceptual framework, her definition of nursing, and the ongoing application of her model in both practice and research.
What is the significance of Henderson’s theory in nursing?
Henderson’s contribution is significant because it provided a clear conceptual model that unites the nursing process with the practical realities of nursing care. By articulating the 14 components that encompass physical, psychological, social, and spiritual dimensions of health, her theory offered nurses a systematic way to identify the needs of individuals and plan interventions. This structure ensured that care would be comprehensive rather than task-oriented.
In clinical practice, Henderson’s framework has been applied to diverse settings, from acute medical-surgical units to long-term care facilities. For instance, a case study involving elderly patients in a community health program showed that when assessments were structured around Henderson’s 14 needs, nurses were better able to identify unmet nutritional and mobility requirements. Addressing these needs led to improved quality of life and reduced hospital readmissions. This demonstrates the practical application of the theory in improving patient outcomes.
The theory also supports the base for professional nursing practice because it emphasizes both independent and collaborative functions of the nurse. By linking nursing to the fulfillment of basic health needs and require assistance, Henderson clarified the boundaries of nursing while reinforcing its holistic scope. Her work bridged the gap between theory and bedside practice, making her model a touchstone in both nursing education and advanced nursing practice.
How does Henderson define nursing?
Henderson’s definition of nursing remains one of the most cited in the field. She stated that:
“The unique function of the nurse is to assist the individual, sick or well, in the performance of those activities contributing to health or its recovery, or to peaceful death, that he would perform unaided if he had the necessary strength, will, or knowledge.”
This definition captures several essential dimensions of the nature of nursing:
- Assist the individual – Nursing is fundamentally about partnership and support, not simply performing tasks.
- Health or its recovery – Care aims at both restoration and maintenance of wellness.
- Peaceful death – Henderson acknowledged that when cure is not possible, the nurse’s role extends to comfort and dignity at the end of life.
- Strength, will, or knowledge – Patients may lack physical capacity, motivation, or education, and nurses must adapt care strategies accordingly.
For example, in palliative care, a patient with advanced cancer may no longer have the strength to meet hydration and nutritional needs independently. A nurse applying Henderson’s framework would provide fluids and nourishment as needed while also offering comfort measures, emotional support, and education for the family. This approach demonstrates the holistic nature of her model, which attends to both physical and social needs in the context of the patient’s values and choices.
Through this definition, Henderson established nursing as a distinct discipline with its own focus, separate from medicine but complementary to it. Her insistence on independence, dignity, and individualized care has ensured that her theory continues to guide nursing and allied health education, clinical practice, and global professional standards.
Understanding the Concept of Needs in Nursing
What does the term ‘needs’ refer to in Henderson’s theory?
In Virginia Henderson’s nursing theory, the term needs refers to the fundamental requirements every human being must meet to maintain life, preserve health, recover from illness, or experience a peaceful death when recovery is no longer possible. Henderson outlined these in her well-known 14 basic needs, which encompass physiological, psychological, social, and spiritual aspects of life. They range from essential physical functions such as breathing, eating, and eliminating wastes to broader human experiences like communication, learning, and recreation.
Henderson believed that when an individual cannot independently satisfy one or more of these human needs, the unique function of the nurse is to step in—either by doing for the patient, helping the patient to do, or teaching them to regain independence. In this way, the nursing process becomes anchored to needs: assessment identifies which of the 14 components are unmet, planning targets specific interventions, and evaluation measures whether the patient is regaining the ability to perform those activities.
For instance, consider a postoperative patient who cannot move freely because of pain. The unmet need here relates to movement and posture. A nurse applying Henderson’s framework would assess the extent of limitation, implement interventions like pain control and assisted ambulation, and gradually encourage the patient to regain mobility. This example demonstrates how the concept of needs guides both the care plan and the long-term goal of restoring independence.
Why is it important to address patient needs in nursing care?
Addressing patient’s needs is central to the nature of nursing because it transforms care from a task-oriented activity into a holistic, individualized practice. Henderson argued that the goal of nursing is not merely to carry out physician’s orders but to ensure that patients’ basic health needs and require assistance are consistently met. This is important for several reasons:
- Foundation of nursing care. The 14 components provide a structured way to deliver basic nursing care. By focusing on needs such as hygiene, nutrition, communication, and rest, the nurse ensures that no essential aspect of health is overlooked. For example, in long-term care facilities, nurses often use Henderson’s model to check whether residents are eating adequately, maintaining skin integrity, and receiving adequate sleep—needs that, if ignored, can quickly lead to complications.
- Holistic approach. Needs in Henderson’s model are not limited to the physical body; they include social needs and psychological well-being. A patient who is unable to express fears or concerns may suffer emotionally even if their physical care is optimal. By attending to needs like communication and emotional expression, nurses provide a holistic nature of care that addresses the entire person.
- Independence and dignity. Henderson emphasized that the nurse is to assist individuals only until they are able to meet their own needs. This emphasis on independence respects the patient’s dignity and prepares them for life beyond hospitalization. For example, a diabetic patient may initially depend on a nurse for insulin injections, but through teaching and support, they can learn self-administration—a direct reflection of Henderson’s insistence on promoting independence.
How does meeting patient needs impact health outcomes?
Meeting patient needs has measurable effects on both individual recovery and broader health system outcomes. When the nursing need theory is applied, health outcomes improve in the following ways:
- Reduced complications. By systematically assessing and addressing needs such as mobility, nutrition, and elimination, nurses prevent complications like pressure ulcers, malnutrition, and urinary infections. For example, ensuring adequate hydration and mobility for an elderly patient directly reduces the risk of constipation and pressure injuries.
- Enhanced recovery. When nurses align interventions with the needs of individuals, recovery tends to be faster and more sustainable. A case study in rehabilitation nursing showed that patients recovering from hip fractures regained independence more quickly when their care plans explicitly addressed Henderson’s 14 activities, including movement, hygiene, and communication.
- Improved patient satisfaction. Patients report higher satisfaction when they feel their individual needs are understood and respected. For example, in palliative care, when nurses focus not only on physical comfort but also on emotional and spiritual needs, patients and families perceive care as more compassionate and meaningful.
- Support for the nursing profession. Henderson’s model strengthens the base for professional nursing practice by clearly demonstrating the contribution of nurses to health outcomes. When nurses can show that meeting the 14 fundamental needs results in fewer readmissions and better quality of life, it highlights the unique role of the profession within healthcare teams.
Illustrative example: Imagine a patient recovering from pneumonia. Henderson’s framework prompts the nurse to assess whether the patient can breathe normally (respiratory function), eat and drink adequately (nutrition and hydration), and sleep sufficiently (rest). If the patient struggles with shortness of breath and poor appetite, the nurse applies oxygen therapy, provides small frequent meals, and teaches energy conservation techniques. Over time, these targeted interventions not only address immediate deficits but also promote gradual independence, reducing the likelihood of relapse or readmission.
What are the 14 Basic Needs According to Virginia Henderson?
What are the 14 basic needs outlined by Henderson?
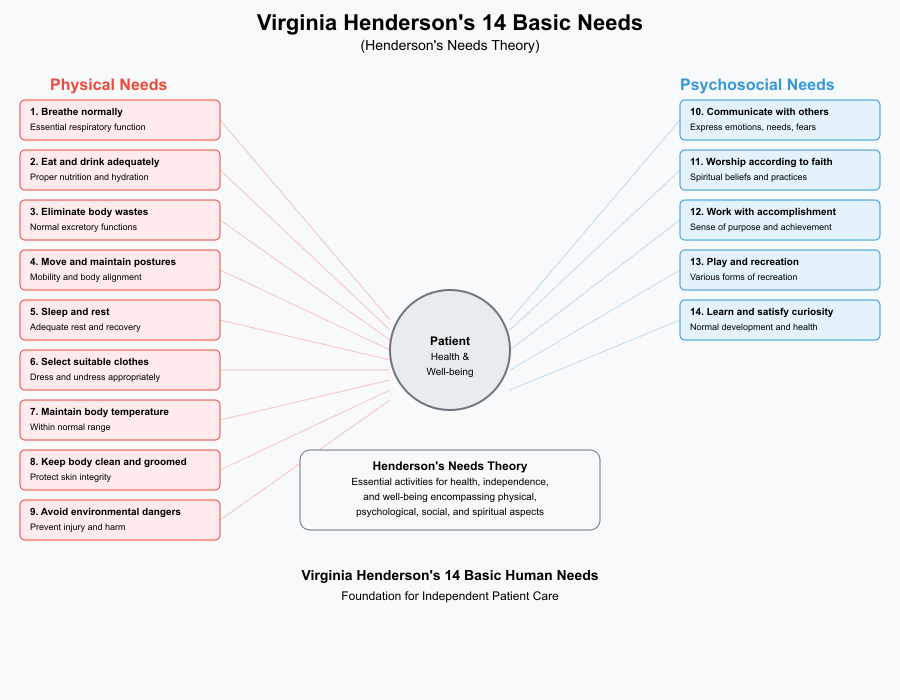
Virginia Henderson’s nursing theory, also known as the needs theory, is most widely recognized for its identification of the 14 basic needs of the patient. These needs form the backbone of her model and represent the activities essential for health, independence, and well-being. They encompass physical, psychological, social, and spiritual aspects of human life:
- Breathe normally
- Eat and drink adequately
- Eliminate body wastes
- Move and maintain desirable postures
- Sleep and rest
- Select suitable clothes—dress and undress
- Maintain body temperature within normal range by adjusting clothing and modifying environment
- Keep the body clean and well groomed and protect the integument
- Avoid dangers in the environment and prevent injury
- Communicate with others in expressing emotions, needs, fears, or opinions
- Worship according to one’s faith
- Work in such a way that there is a sense of accomplishment
- Play or participate in various forms of recreation
- Learn, discover, or satisfy curiosity that leads to normal development and health, and use available health facilities.
Henderson’s framework reflects her belief that the nature of nursing lies in assisting patients to meet these needs when they are unable to do so independently. Unlike some nursing theorists who emphasized abstract conceptual models, Henderson offered a concrete, practical guide for everyday nursing practice.
How can these needs be applied in clinical practice?
The 14 basic needs are not just theoretical—they serve as a conceptual framework for assessing, planning, and implementing nursing care. Here are some examples of their application in practice:
- Acute care setting: A patient admitted with pneumonia may struggle with the first need—breathing normally. Nurses provide oxygen therapy, monitor respiratory rate, and position the patient to improve ventilation. At the same time, they assess whether the patient is meeting the needs of eating, resting, and communicating discomfort.
- Post-surgical recovery: After abdominal surgery, patients often need assistance with elimination of wastes, mobility, and sleep and rest. Nurses support them by providing pain management, encouraging early ambulation, and monitoring bowel function.
- Long-term care: In geriatric nursing, patients may have deficits in personal hygiene, grooming, and maintaining body temperature. Nurses in this setting design care plans that include daily hygiene routines, proper clothing selection, and skin protection.
- Mental health care: For patients with depression, addressing the needs of communication, work with a sense of accomplishment, and play or recreation becomes central. Nurses encourage expression of feelings, introduce therapeutic activities, and guide patients to rediscover interests and hobbies.
- Palliative care: In end-of-life settings, the needs of worship according to faith, avoiding dangers, and maintaining dignity through grooming and hygiene are crucial. Here, nurses not only manage pain but also create conditions that preserve comfort, respect spirituality, and foster a peaceful environment.
Why are these basic needs considered fundamental for patient care?
The 14 basic needs are considered fundamental because they represent the universal building blocks of life and health. Without addressing them, nursing care becomes fragmented and incomplete. Their importance lies in:
- Universality: Henderson designed the needs to apply to all people, regardless of age, culture, or health condition. Whether caring for a premature infant, an adult with chronic illness, or an elderly patient in hospice, these needs provide a common standard.
- Holism: They capture more than just physical health. Needs like communication, worship, recreation, and learning emphasize that nursing is about the whole person—body, mind, and spirit—not just about medical treatment.
- Basis for independence: Henderson defined the role of the nurse as assisting individuals until they can regain independence in meeting their own needs. This principle empowers patients and reduces dependency on health services in the long term. For example, teaching a diabetic patient to manage diet and insulin injections addresses needs of nutrition, learning, and independence, directly improving outcomes.
- Link to outcomes: Meeting these needs reduces complications, accelerates recovery, and improves quality of life. A patient whose mobility needs are addressed early is less likely to develop pressure ulcers or respiratory complications.
- Strengthening the profession: By clearly identifying the unique function of the nurse, Henderson’s framework distinguishes nursing practice from medicine. It highlights how nurses contribute to patient survival, recovery, and well-being through a needs-centered approach.
How to Implement Henderson’s Needs Theory in Nursing Practice?
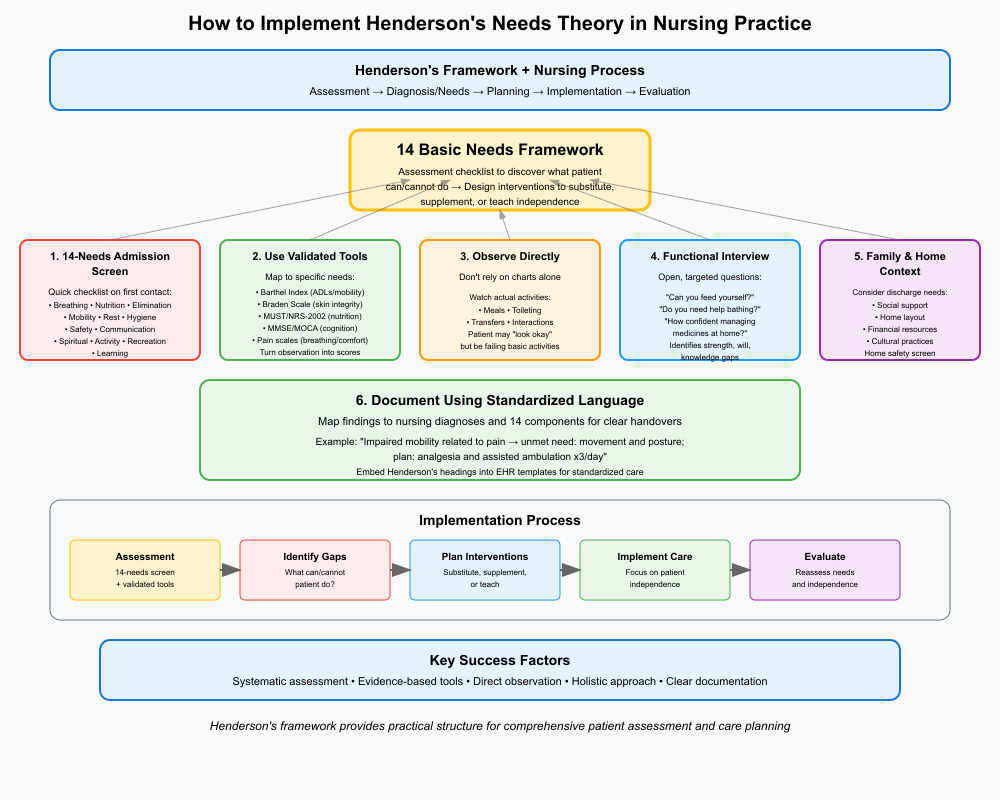
Henderson’s needs theory is deliberately practical: it turns the 14 basic needs into a working assessment framework that links directly to the nursing process (assessment → diagnosis/needs → planning → implementation → evaluation). In practice this means using the 14 components as a checklist to discover what a patient can and cannot do, then designing interventions that either substitute for, supplement, or teach the patient to perform those activities independently. This structure makes Henderson’s model easy to embed into admission assessments, shift handovers and care plans.
What strategies can student nurses use to assess patient needs?
Use these practical, evidence-based strategies to convert Henderson’s conceptual list into usable assessment data:
- Start with a 14-needs admission screen.
- On first contact, run a quick checklist tied to Henderson’s components (airway/breathing; nutrition; elimination; mobility; rest; hygiene; safety; communication; spiritual/religious needs; meaningful activity; recreation; learning). This gives an immediate map of possible deficits to explore in depth. Many clinical educators recommend structuring admission forms and handovers around these domains so nothing essential is missed.
- Use validated tools that map to specific needs.
- ADLs / functional mobility: Barthel Index or Functional Independence Measure (maps to movement, dressing, toileting, eating).
- Skin/integrity risk: Braden Scale (relates to integument protection).
- Nutrition: MUST or NRS-2002 (eating/drinking adequately).
- Cognition and communication: MMSE / MOCA and language screen.
- Pain and breathing: pain scales, respiratory rate/oxygenation (breathing normally).
These tools turn observation into objective scores you can chart, trend and act upon.
- Observe—don’t rely on chart data alone.
- Watch meals, toileting, transfers and interactions. A patient may “look okay” in notes yet be failing several basic activities in reality (e.g., poor intake, ineffective cough). Direct observation is often the most revealing assessment method for Henderson’s needs.
- Interview using open, functional questions.
- Ask questions that target function: “Can you feed yourself?” “Do you need help with bathing?” “How confident are you to manage your medicines at home?” This approach elicits whether needs are being met and whether the patient lacks strength, will or knowledge — Henderson’s three reasons a person might be unable to perform an activity.
- Include family and home context.
- Social support, home layout, finances and cultural practices determine whether the patient’s needs can be met after discharge. Include a quick home-safety and support screen during assessment.
- Document using standardised language.
- Map findings to nursing diagnoses (or problem statements) and to the 14 components so handover and multi-disciplinary teams understand the gap (e.g., “Impaired mobility related to pain → unmet need: movement and posture; plan: analgesia and assisted ambulation x3/day”). Embedding Henderson’s headings into EHR templates or nursing notes helps standardise care and handovers.
How can you prioritize needs in a nursing care plan?
Prioritisation turns a long list of unmet needs into a sequence of safe, practical actions. Use a simple, defensible approach:
- Immediate threats first (ABCs / risk of harm).
- Always give absolute priority to needs that affect survival or can cause rapid deterioration: breathing normally, airway, circulation, severe bleeding, acute safety threats. Example: a patient who is hypoxic (breathing compromised) must get oxygen/positioning and rapid escalation before addressing grooming or recreation.
- Prevent avoidable complications next (high-risk needs).
- Needs that if ignored will cause harm within hours/days: poor nutrition leading to dehydration, immobility increasing pressure-injury risk, inability to clear secretions risking pneumonia.
- Functional restoration and independence (rehabilitative priority).
- Intervene to restore ability in activities that enable discharge: eating, dressing, toileting, medication management. Use time-bound SMART goals—e.g., “Patient will perform sit-to-stand with minimal assistance by day 3” — that map to Henderson’s movement and self-care components.
- Psychosocial/spiritual needs and learning (ongoing and parallel).
- Communication, learning and spiritual needs run alongside physical care and often influence adherence and recovery. E.g., teaching about wound care should be scheduled when the patient is rested and pain-controlled.
- Incorporate patient values and goals.
- If a patient prioritises a particular need (e.g., attending a cultural ceremony), negotiate care around that value where clinically safe. Henderson’s model supports patient-centred prioritisation because it emphasises the individuality of needs.
- Make delegation and sequencing explicit.
- Use care bundles: what the nurse must do vs what can be delegated (e.g., morning hygiene tasks assigned to assistant while nurse focuses on analgesia and mobilization). Document who does what and when, with measurable outcomes.
Case example — prioritisation in practice:
A frail postoperative patient has low oxygen saturation, poor oral intake and is confused at night. Prioritise:
(1) breathing (oxygen, positioning, respiratory assessment)
(2) delirium/medication review (safety, prevent falls)
(3) short-term nutrition plan (small frequent feeds, oral supplements)
(4) sleep hygiene and family involvement for reorientation.
Each item maps to Henderson’s needs and is sequenced by risk and likely impact on recovery.
Practical frameworks used in practice include ABCs + risk screening + functional goals (a hybrid that blends medical urgency with Henderson’s needs and Maslow-style priorities). Literature on integrating nursing theory into care pathways shows that using clear prioritisation tied to a conceptual model improves consistency of care and handovers.
What role does communication play in addressing patient needs?
Communication is the mechanism by which needs are discovered, negotiated and met. Good communication supports assessment accuracy, patient learning, safety and teamwork.
- Therapeutic communication with the patient
- Use open questions, active listening and empathy to explore needs that are not immediately visible (fears, spiritual concerns, learning needs). Example: asking “What worries you most about going home?” can reveal learning and social needs that must be addressed in the care plan.
- Teach-back for learning and independence
- After education (wound care, medication administration), ask the patient to demonstrate or explain back the steps. Teach-back reduces errors and confirms the need for further teaching — directly supporting Henderson’s emphasis on restoring knowledge and independence.
- Clear handover (SBAR or structured nursing notes)
- When integrating the 14 needs into handover, use SBAR (Situation, Background, Assessment, Recommendation) but map the Assessment to Henderson domains: e.g., “Assessment: breathing OK on 2L O₂; mobility: needs two people to transfer; learning: requires wound-care teaching.” Standardising handover language reduces omissions and speeds team responses.
- Interdisciplinary communication
- Many needs require a team approach (physiotherapy for movement, dietetics for eating, chaplaincy for spiritual care). Communicate assessed needs and explicit referrals so other disciplines can act. Document referrals and expected follow-up in the plan of care.
- Cultural and language sensitivity
- Use interpreters, involve family where appropriate, and adapt health education to cultural beliefs. Communication that misses cultural context can leave critical needs unmet (for example, dietary advice that conflicts with cultural food practices).
- Documenting conversations and preferences
- Record advance care preferences and spiritual wishes (important in palliative situations where “peaceful death” is an aim). Clear documentation ensures the whole team honours patient goals.
Research emphasises that strong communication skills bridge the gap between recognising needs (including spiritual needs) and delivering acceptable, evidence-based care — poor communication commonly explains why identified needs remain unmet.
Challenges in Applying Henderson’s Theory
What are common obstacles faced by student nurses when using this theory?
While Virginia Henderson’s nursing theory offers a clear and structured guide to meeting the 14 basic needs, many student nurses find it challenging to translate the framework into day-to-day nursing practice. Some of the common obstacles include:
- Complexity of patient care
- Patients rarely present with just one unmet need. For example, a stroke patient may simultaneously struggle with breathing, mobility, nutrition, communication, and hygiene. For novice nurses, this complexity can feel overwhelming, making it difficult to know how to apply the needs theory systematically.
- Time constraints and workload
- In busy clinical environments, students often feel pressured to complete tasks quickly. Activities like thorough assessment of all 14 basic needs may be replaced with task-oriented care, which risks overlooking less obvious but equally important needs (e.g., recreation, learning, or spiritual care).
- Limited clinical experience
- Without prior exposure, it may be difficult for students to recognize how unmet needs manifest. For example, a patient’s refusal to eat may reflect not just appetite loss but also unmet emotional or spiritual needs. Identifying these nuances requires both experience and mentoring.
- Documentation challenges
- Many electronic health records (EHRs) are structured around medical diagnoses rather than Henderson’s conceptual model. Students may find it hard to align the nursing process and nursing care plans with the 14 components when documentation tools don’t directly support them.
- Misunderstanding of Henderson’s purpose
- Some students interpret Henderson’s work as a rigid checklist rather than a holistic definition of nursing. This narrow view can reduce its effectiveness, as the model was intended to emphasize patient individuality and independence rather than prescriptive task completion.
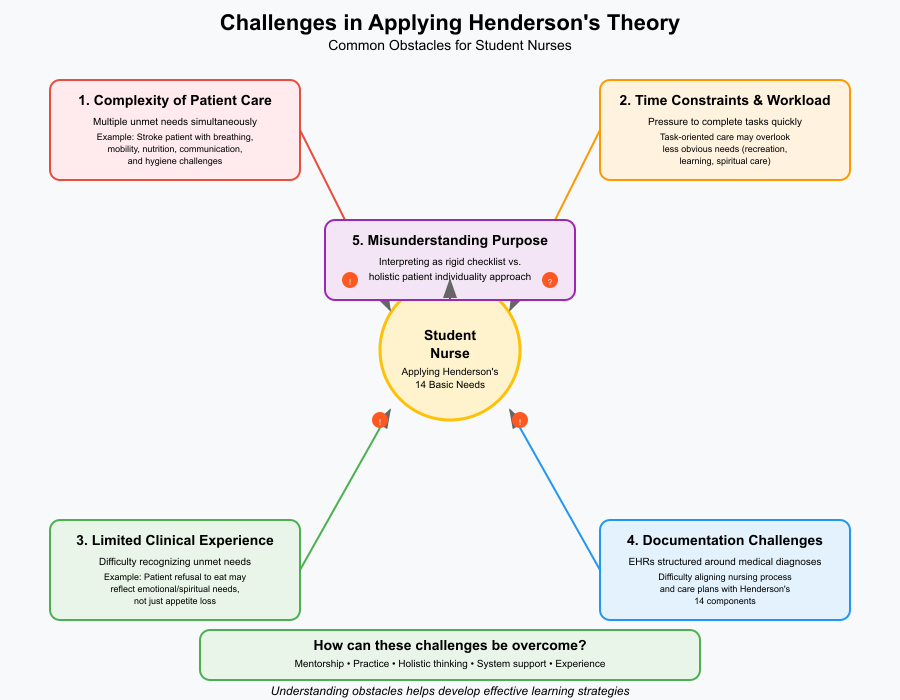
How can these challenges be overcome?
- Prioritization frameworks
- Applying Maslow’s hierarchy alongside Henderson’s model helps students distinguish urgent physiological needs (breathing, circulation, nutrition) from longer-term psychosocial ones (recreation, learning, spirituality). For instance, when caring for a post-operative patient, airway management takes precedence, but recreation and communication remain important as recovery progresses.
- Integrating the model into the nursing process
- Students should map assessments and care plans directly to the 14 basic needs. For example, “Impaired mobility related to surgical pain” links to Henderson’s fourth component (movement and posture). By practicing this mapping, students internalize the model and strengthen clinical reasoning.
- Simulation-based learning
- Clinical simulation labs can be used to role-play scenarios where multiple needs overlap. A patient mannequin programmed with respiratory distress, anxiety, and communication barriers allows students to practice prioritizing interventions while still considering holistic care.
- Mentorship and guided reflection
- Experienced nurses can demonstrate how they apply Henderson’s theory in real-world situations. Reflective debriefings after clinical placements help students evaluate how many of the 14 needs they addressed and where gaps occurred.
- Simplifying documentation
- Even if electronic systems don’t explicitly use Henderson’s categories, students can structure their notes to reflect the needs (e.g., “Need 1: Breathing—O₂ sat 92% on 2L” or “Need 10: Communication—difficulty expressing pain”). This habit reinforces Henderson’s language and keeps care patient-centered.
What support systems are available for student nurses?
- Nursing schools and curricula
- Many nursing schools deliberately integrate Henderson’s theory into coursework, case studies, and skill labs. Structured learning around the 14 components ensures students see how the theory underpins both fundamental and advanced nursing practice.
- Mentorship and preceptorship programs
- Hospitals often pair student nurses with experienced staff who model theory-based nursing care. Preceptors can guide students through the practical application of Henderson’s needs theory, showing how it influences decision-making in busy wards.
- Professional organizations and resources
- The International Council of Nurses promotes resources on nursing theories and global standards for care. Henderson herself was connected with the ICN, and students can draw upon their publications and frameworks to deepen understanding of the nature of nursing.
- Learning tools and technology
- Mobile apps and digital learning platforms now include case studies and interactive modules based on Henderson’s nursing theory. For example, students can work through virtual scenarios where they must assess which of the 14 needs are unmet and design appropriate interventions.
- Peer support and study groups
- Discussing patient cases with peers allows students to identify gaps and share strategies for applying Henderson’s theory. For instance, one student may recognize a spiritual need that another overlooked, highlighting the importance of collaboration in holistic care.
Conclusion
In summary, while Virginia Henderson’s nursing need theory offers one of the most practical and holistic frameworks in nursing practice, its application is not always straightforward for student nurses. The reality of complex patient conditions, competing demands in clinical settings, and documentation systems that may not align with the 14 basic needs often create barriers. However, these challenges also present valuable learning opportunities. By combining theory with tools such as prioritization frameworks, simulation exercises, reflective practice, and mentorship, students can transform these obstacles into stepping stones toward competence.
Support systems—ranging from nursing education programs to peer collaboration and professional resources—ensure that student nurses are not left to struggle alone. Ultimately, overcoming these challenges reinforces Henderson’s central vision: that the role of the nurse is not only to address immediate needs but also to empower patients toward greater independence. For students, learning to bridge the gap between theory and practice is an essential milestone in their professional development and a foundation for delivering safe, compassionate, and person-centered nursing care.
Frequently Asked Questions
What are the 14 basic needs according to Virginia Henderson?
Virginia Henderson identified 14 basic needs that nurses must address to support patient independence. These include breathing normally, eating and drinking adequately, eliminating body wastes, moving and maintaining posture, sleeping and resting, selecting appropriate clothing, maintaining body temperature, keeping the body clean, avoiding dangers, communicating, practicing faith or values, working toward accomplishment, engaging in recreation, and learning for health and development.
What is the Virginia Henderson theory of nursing needs?
Henderson’s nursing need theory emphasizes that the unique role of the nurse is to assist individuals—sick or well—in performing activities that contribute to health, recovery, or a peaceful death. These activities align with the 14 basic needs, and the ultimate goal is to help patients gain independence as quickly as possible.
What are the four main concepts of Henderson’s theory?
The theory is grounded in the nursing metaparadigm concepts:
- Person – the individual with basic needs who requires assistance.
- Health – the ability to function independently and meet basic needs.
- Environment – external factors that influence health and nursing care.
- Nursing – assisting individuals to meet needs and regain independence.
Who developed the 14 basic needs nursing theory?
The 14 basic needs nursing theory was developed by Virginia Henderson, an American nurse theorist, educator, and researcher, often referred to as the “First Lady of Nursing” for her profound contributions to the profession.
