Veracity in Nursing: Why Truthfulness Matters for Every Nurse
Veracity in nursing is a fundamental ethical principle that underpins the integrity of the nursing profession. At its core, veracity emphasizes truthfulness and honesty, guiding nurses in their interactions with patients, families, and healthcare professionals. Just as clinical protocols provide structured approaches to patient care, veracity offers nurses a framework for ethical decision-making, ensuring that communication, documentation, and professional conduct remain transparent and trustworthy. Far from being merely a philosophical concept, veracity in nursing shapes daily practice by fostering open dialogue, supporting patient autonomy, and reinforcing the ethical standards set forth by the American Nurses Association (ANA) and the nursing code of ethics.
In practice, veracity requires that nurses are truthful and open when conveying information about diagnoses, treatment options, and potential outcomes, even in complex or emotionally charged situations. Upholding veracity is closely linked with other core ethical principles, including beneficence, nonmaleficence, and fidelity, and plays a central role in establishing and maintaining a trusting nurse-patient relationship. It provides a foundation for informed consent, enabling patients to make decisions about their healthcare that reflect their values, preferences, and best interests.
Understanding veracity in nursing goes beyond compliance with ethical guidelines; it is about cultivating a professional commitment to honesty that informs every aspect of nursing care. From interactions at the bedside to interdisciplinary collaboration, practicing veracity ensures that nurses act consistently with ethical principles, safeguard patient welfare, and strengthen the credibility of the nursing profession. This article explores veracity in nursing comprehensively, detailing its definition, historical context, practical application, relationship to other ethical principles, and the guidance provided by professional codes of ethics. Through real-world examples and case scenarios, readers will gain insight into how nurses can uphold veracity while navigating the ethical complexities inherent in modern healthcare settings.
Understanding Veracity as an Ethical Principle in Nursing
Defining Veracity in Nursing Practice
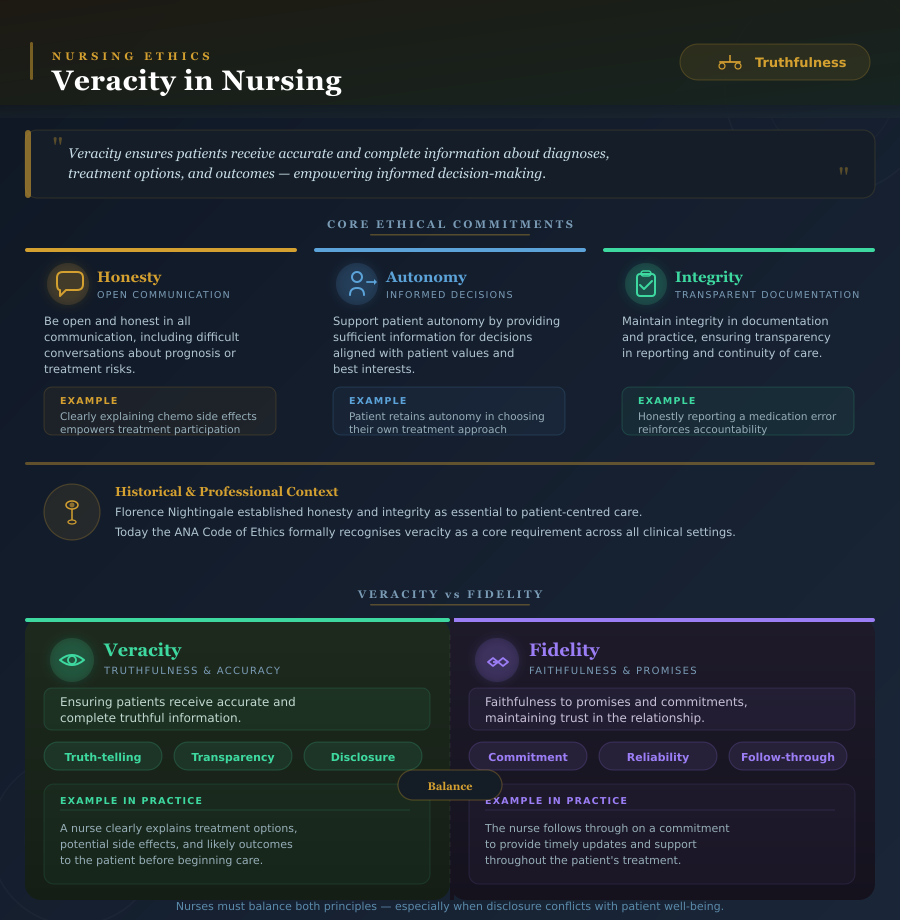
Veracity in nursing is a foundational ethical principle that emphasizes truthfulness, honesty, and transparency in all aspects of patient care. It is central to the nurse-patient relationship, guiding how nurses communicate, document, and collaborate with patients, families, and healthcare professionals. At its core, veracity ensures that patients receive accurate and complete information about their diagnoses, treatment options, and potential outcomes, which allows them to make informed decisions about their healthcare.
In daily practice, veracity in nursing practice extends beyond simply providing factual information. It encompasses an ethical commitment to:
- Be open and honest in communication, including difficult conversations about prognosis or treatment risks.
- Support patient autonomy by providing sufficient information for patients to make informed decisions aligned with their values and best interests.
- Maintain integrity in documentation and nurse practice, ensuring transparency in reporting and continuity of care.
For example, a nurse who communicates clearly about the side effects of chemotherapy not only practices veracity but also empowers the patient to participate actively in their treatment plan. Similarly, when reporting a medication error, a nurse demonstrates veracity by honestly informing the patient and healthcare team, reinforcing ethical standards and accountability in nursing care.
Historical and Professional Context
The emphasis on veracity within nursing ethics is deeply rooted in the profession’s history. Early nursing leaders, such as Florence Nightingale, highlighted honesty and integrity as essential to patient-centered care. While fidelity in nursing—the commitment to keeping promises and honoring professional obligations—was initially a primary ethical focus, over time veracity emerged as a distinct but complementary principle, emphasizing truth-telling and transparency.
Today, veracity is formally recognized in professional guidelines. The American Nurses Association (ANA) Code of Ethics for Nurses highlights that nurses must provide truthful information, uphold ethical standards, and integrate veracity into all facets of nursing care. Veracity is not optional; it is a core requirement within the nursing profession, influencing communication, decision-making, and patient advocacy across clinical settings.
For instance, in modern healthcare, a nurse caring for a patient with a terminal illness must deliver honest updates regarding prognosis while ensuring the patient retains autonomy in choosing treatment approaches. This practice reflects the integration of veracity into both ethical and professional nursing responsibilities.
Veracity versus Fidelity in Nursing Ethics
Although veracity and fidelity are closely related, they serve different purposes in nursing ethics. Veracity is concerned with truthfulness, ensuring patients receive accurate and complete information. Fidelity, on the other hand, emphasizes faithfulness to promises and commitments, maintaining trust in the nurse-patient relationship.
For example, a nurse demonstrates veracity by clearly explaining a patient’s treatment options, potential side effects, and likely outcomes. Fidelity is demonstrated when the nurse follows through on a commitment to provide timely updates or support during treatment. In many situations, nurses must balance both principles, particularly when facing ethical dilemmas where complete disclosure could conflict with patient well-being. For instance, if a patient requests that a serious diagnosis be withheld from family members, the nurse must carefully weigh veracity, fidelity, beneficence, and nonmaleficence to determine the most ethically appropriate course of action.
Understanding the interplay between veracity and fidelity is essential for nurses to practice veracity effectively. By consistently demonstrating honesty while maintaining commitments, nurses strengthen patient trust, enhance nursing care, and uphold the ethical standards of the nursing profession.
Examples of veracity in nursing practice include:
- Providing truthful explanations about prognosis and treatment outcomes.
- Disclosing medical errors or adverse events to patients and healthcare professionals.
- Ensuring accurate and transparent documentation of patient care.
- Engaging in open communication during informed consent discussions to support patient decision-making.
Through these practices, nurses uphold the principle of veracity, reinforcing ethical behavior, supporting patient autonomy, and fostering a culture of trust within healthcare teams.
The Role of Veracity in Nursing Care
Veracity in the Nursing Code of Ethics and ANA Guidance
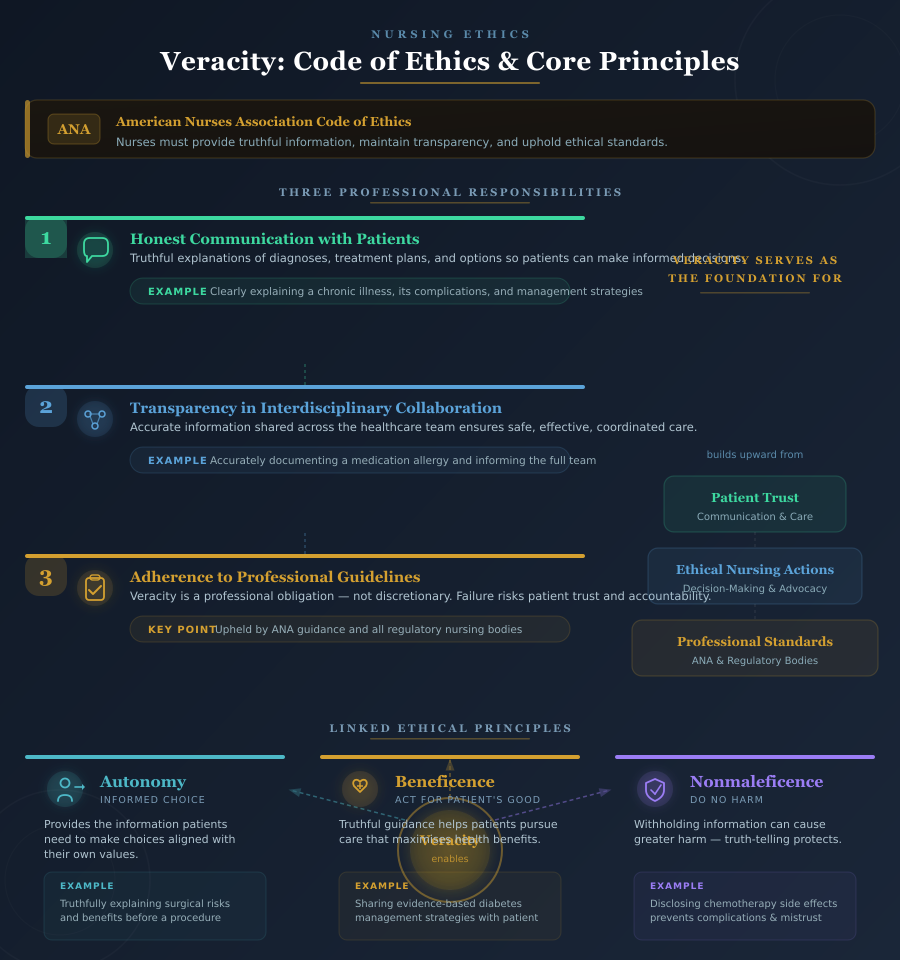
The role of veracity in nursing care is deeply rooted in professional and ethical frameworks. The American Nurses Association (ANA) recognizes veracity as one of the essential principles in nursing, emphasizing the obligation of nurses to practice veracity in all interactions with patients, families, and healthcare professionals. According to the ANA Code of Ethics for Nurses, nurses must provide truthful information, maintain transparency in communication, and uphold ethical standards that protect patient welfare and promote trust in the nursing profession.
Veracity in nursing care is operationalized through multiple responsibilities:
- Honest Communication with Patients: Nurses are required to provide truthful explanations regarding diagnoses, treatment plans, and treatment options. For example, a nurse caring for a patient with a newly diagnosed chronic illness must clearly explain the disease process, potential complications, and management strategies. This ensures the patient can make informed decisions about their healthcare.
- Transparency in Interdisciplinary Collaboration: Nurses must communicate accurate information with the healthcare team, including physicians, pharmacists, and other professionals, to ensure safe and effective patient care. For instance, documenting a medication allergy accurately and informing team members prevents errors and upholds patient safety.
- Adherence to Professional Guidelines: The ANA guidance and nursing code of ethics provide specific expectations for ethical practice, reinforcing that veracity in nursing practice is a professional obligation rather than a discretionary behavior. Nurses who fail to uphold veracity may compromise patient trust, weaken the nurse-patient relationship, and risk professional accountability.
Through these frameworks, veracity serves as a foundation for all ethical nursing actions, aligning nurse practice with the ethical and professional expectations outlined by the ANA and other regulatory bodies.
Upholding Core Ethical Principles in Nursing
Veracity in nursing is intrinsically linked with other ethical principles of nursing, including autonomy, beneficence, and nonmaleficence. Integrating veracity with these principles ensures that nurses make decisions that are ethically sound, patient-centered, and aligned with professional standards.
- Autonomy
- Veracity enables patients to exercise their autonomy by providing them with the information needed to make choices about their healthcare.
- Example: A nurse educating a patient about surgical options must truthfully explain risks and benefits, ensuring the patient can make informed decisions aligned with personal values.
- Beneficence
- Practicing veracity supports beneficence, the ethical obligation to act in the patient’s best interest. Nurses provide truthful guidance to help patients pursue care that maximizes benefits.
- Example: Informing a patient about evidence-based interventions for managing diabetes helps the patient adopt a treatment plan that improves health outcomes.
- Nonmaleficence
- Veracity also aligns with nonmaleficence, the principle of “do no harm.” While truth-telling may sometimes be difficult, withholding information can result in greater harm to the patient.
- Example: A nurse must inform a patient of potential side effects of chemotherapy; failing to do so may lead to unnecessary complications or mistrust in the healthcare system.
By integrating veracity with these ethical principles, nurses ensure that care is not only clinically effective but also ethically robust, balancing patient welfare, safety, and autonomy in every interaction.
Importance of Veracity in Nursing for Patient Care and Decision-Making
The importance of veracity in nursing cannot be overstated. It directly impacts patient care, decision-making, and the nurse-patient relationship, forming the basis of trust and ethical responsibility.
- Facilitating Informed Consent: Informed consent relies on veracity. A nurse ensures that patients receive complete and accurate information about procedures, medications, and treatment options, empowering them to make decisions about their healthcare. For example, before administering a blood transfusion, a nurse explains the risks, benefits, and alternatives so the patient can consent knowledgeably.
- Strengthening Patient Trust: When nurses consistently practice veracity, patients are more likely to trust the nurse and the broader healthcare team. Trust enhances cooperation, adherence to treatment plans, and overall patient satisfaction.
- Supporting Ethical Decision-Making: Veracity provides a foundation for patients and healthcare providers to make ethically sound decisions. By communicating openly about prognosis, care goals, or potential complications, nurses help patients weigh risks and benefits effectively.
Example in Practice: A patient diagnosed with heart failure may receive multiple treatment options, including lifestyle changes, medication adjustments, or surgical interventions. A nurse practicing veracity explains each option honestly, including potential outcomes and limitations, enabling the patient to make informed decisions consistent with their values and best interest.
Practical Application: How Nurses Practice Veracity in Nursing Care
Demonstrating Veracity in Nurse Practice
In nursing practice, demonstrating veracity is an essential responsibility that ensures care is truthful, transparent, and ethically sound. Nurses integrate veracity into daily practice through consistent honesty with patients, families, and healthcare team members, which strengthens the nurse-patient relationship and reinforces trust in the nursing profession.
Ways nurses maintain veracity in practice include:
- Open Communication with Patients: Nurses must provide complete and truthful information about diagnoses, prognoses, and treatment options. This includes explaining potential risks, benefits, and limitations of interventions to enable patients to make informed decisions about their healthcare.
- Engaging Families Transparently: When appropriate, nurses share information with families while respecting patient autonomy and confidentiality, ensuring that communication remains accurate and supportive of the patient’s best interests.
- Collaborating with Healthcare Professionals: Nurses uphold veracity by conveying honest and accurate observations to the broader healthcare team, including physicians, therapists, and pharmacists, to enhance patient safety and ethical nursing care.
For example, a nurse caring for a patient with a chronic illness explains honestly how the condition may progress and what treatment options are available, ensuring the patient can make informed decisions consistent with their values and preferences. By practicing veracity in this manner, nurses demonstrate a commitment to veracity while reinforcing professional integrity.
Documentation and Ethical Standards
Accurate documentation is a critical aspect of practicing veracity in nursing care. Nurses are ethically obligated to maintain precise records that reflect the patient’s condition, interventions provided, and responses to treatment. Accurate charting ensures transparency, supports continuity of care, and aligns with the ethical principles of nursing.
- Reporting Medical Errors: Nurses must be truthful in reporting errors, adverse events, or deviations from standard care practices. This upholds ethical standards, protects patients, and maintains accountability within the healthcare team.
- Transparency in Professional Practice: By maintaining accurate and thorough documentation, nurses uphold core ethical responsibilities, including fidelity and honesty, which are integral to nursing ethics and professional conduct.
For instance, if a medication is inadvertently administered incorrectly, the nurse must immediately document the error and communicate it to the patient, physician, and appropriate members of the healthcare team. This practice reinforces trust, mitigates potential harm, and demonstrates veracity in nursing practice.
Examples of Veracity in Nursing Practice
Practical examples of veracity in nursing illustrate how nurses uphold truthfulness and ethical principles in real-world settings:
- Truthful Disclosure of Prognosis: Informing a patient diagnosed with cancer about the expected course of the disease, while providing emotional support, allows the patient to make informed decisions regarding treatment and personal planning.
- Sharing Test Results Honestly: A nurse communicates laboratory or imaging results directly to the patient, explaining the implications clearly and accurately. This ensures transparency and strengthens the nurse-patient relationship.
- Discussing Treatment Options: Nurses provide objective information on all viable treatment options, including possible side effects, to allow patients to weigh risks and benefits. This practice supports both autonomy and beneficence.
Case Example: Balancing Veracity with Nonmaleficence and Beneficence
Nurses frequently encounter ethical dilemmas where truth-telling must be balanced with the principles of nonmaleficence (“do no harm”) and beneficence (acting in the patient’s best interest). Consider the following scenario:
Scenario: A patient with a terminal illness asks a nurse about the likely outcome of their treatment. The family requests that the nurse withhold certain details to prevent emotional distress.
Ethical Analysis:
- Veracity: The nurse has an obligation to provide truthful information, ensuring the patient understands their prognosis and can make informed decisions.
- Nonmaleficence: Withholding information may protect the patient from immediate emotional harm but could compromise trust and long-term decision-making.
- Beneficence: Providing accurate information allows the patient to take steps that align with their values, such as completing personal affairs or choosing appropriate palliative care.
Nursing Decision-Making:
- The nurse engages in a compassionate discussion, delivering information truthfully while providing emotional support.
- The nurse ensures that the patient has access to counseling or support services to manage emotional distress.
- Collaboration with the healthcare team ensures that ethical standards and institutional policies are followed, maintaining professional integrity and upholding veracity in nursing.
This case illustrates how nurses navigate complex clinical situations, balancing truthfulness, ethical principles, and patient-centered care, while reinforcing the importance of veracity as a principle in nursing.
Veracity and Other Ethical Principles in Nursing Ethics
Veracity and Patient Autonomy
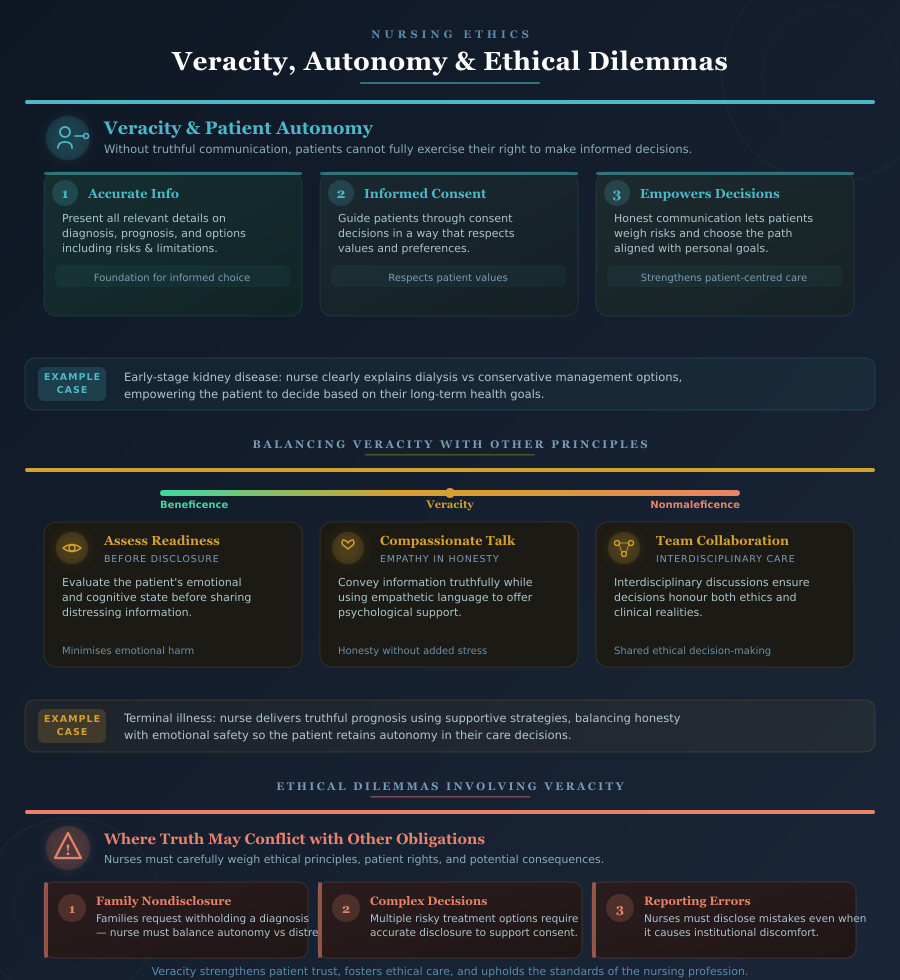
In nursing practice, veracity is intrinsically linked to patient autonomy, one of the core ethical principles in nursing. Patient autonomy refers to a patient’s right to make decisions about their own healthcare based on accurate and complete information. Without truthful communication, patients cannot fully exercise their autonomy, and the nurse-patient relationship may be compromised.
How veracity supports patient autonomy:
- Providing accurate information: A nurse must present the patient with all relevant details about their diagnosis, prognosis, and treatment options, ensuring they understand potential benefits, risks, and limitations.
- Enabling informed consent: Nurses play a pivotal role in the informed consent process, guiding patients to make informed decisions about procedures, medications, or interventions in a way that respects their values and preferences.
- Empowering decision-making: When a nurse communicates honestly and openly, patients are better able to evaluate options, weigh risks, and choose the care path that aligns with their best interest and personal goals.
Example: A patient with early-stage kidney disease is presented with multiple treatment options, including dialysis or conservative management. A nurse practicing veracity provides clear, unbiased explanations of each option’s outcomes, empowering the patient to make a decision consistent with their autonomy and long-term health goals.
Through this approach, veracity in nursing practice strengthens patient-centered care, fosters trust in the nursing profession, and ensures ethical standards are upheld in everyday clinical interactions.
Balancing Veracity with Beneficence and Nonmaleficence
While veracity promotes honesty and transparency, nurses often encounter situations where truth-telling must be carefully balanced with beneficence (acting in the patient’s best interest) and nonmaleficence (avoiding harm). Navigating these ethical intersections requires clinical judgment, sensitivity, and adherence to ethical standards in nursing.
Strategies for balancing veracity with beneficence and nonmaleficence include:
- Assessing patient readiness: Before sharing potentially distressing information, nurses evaluate the patient’s emotional and cognitive state to ensure disclosure minimizes harm.
- Using compassionate communication: Nurses convey information truthfully while employing empathetic language, supporting patients psychologically while maintaining honesty.
- Collaborating with the healthcare team: Interdisciplinary discussions ensure that decisions respect both ethical principles of nursing and clinical realities.
Example: A patient diagnosed with a terminal illness expresses fear and anxiety about prognosis. The nurse must practice veracity by providing truthful information while using supportive strategies to reduce distress, balancing beneficence and nonmaleficence. By doing so, the patient receives accurate information necessary for decision-making while experiencing care that prioritizes emotional safety.
Ethical Dilemmas Involving Veracity
Nurses frequently encounter ethical dilemmas in which the obligation to be truthful may conflict with patient safety, family requests, or institutional policies. These situations challenge nurses to weigh ethical principles in nursing, patient rights, and potential consequences carefully.
Common scenarios include:
- Family requests for nondisclosure: Families may ask nurses to withhold a diagnosis or prognosis to protect the patient from emotional distress. Nurses must balance veracity with beneficence and nonmaleficence, often engaging in sensitive discussions to uphold the patient’s autonomy.
- Complex medical decisions: Patients may face multiple treatment options, each with risks and benefits. Nurses must convey accurate information, even when the implications may be distressing, to support informed consent and patient-centered decision-making.
- Reporting errors or adverse events: Nurses face the ethical obligation to tell the truth regarding mistakes, even if disclosure may provoke institutional challenges or discomfort among healthcare professionals.
Example: A nurse discovers a critical laboratory error that may affect a patient’s treatment plan. The family requests that the error not be disclosed to the patient. The nurse must uphold veracity in nursing, balancing the ethical principles of beneficence, nonmaleficence, and autonomy, by reporting the error transparently while providing support to the patient and family.
Professional Guidance: Codes, Standards, and Nursing Programs
Role of the ANA and Nursing Code of Ethics in Veracity
Professional guidelines, particularly the American Nurses Association (ANA) Code of Ethics for Nurses, play a crucial role in shaping how nurses uphold veracity in nursing practice. The ANA emphasizes that nurses must be truthful, transparent, and accountable in all patient interactions, reflecting the core ethical principles of the profession. By adhering to these guidelines, nurses are able to integrate veracity systematically into daily nursing care, ensuring ethical, patient-centered practice.
The nursing code of ethics provides:
- Clear expectations for ethical communication: Nurses are instructed to provide accurate information regarding diagnoses, prognoses, and treatment options, ensuring patients can make informed decisions.
- Frameworks for ethical decision-making: The Code of Ethics offers guidance for resolving situations where veracity may conflict with other principles, such as beneficence or nonmaleficence.
- Institutional and policy alignment: By following professional standards, nurses maintain compliance with scope of practice requirements, organizational policies, and legal obligations, reinforcing trust in the nursing profession.
Example: A nurse working in a hospital must disclose a medication error truthfully, in accordance with ANA guidance, while collaborating with the healthcare team to prevent harm and communicate effectively with the patient. By doing so, the nurse demonstrates adherence to ethical standards, accountability, and the principle of veracity.
Fidelity and Veracity in the Nursing Profession
Fidelity in nursing complements veracity by emphasizing faithfulness to professional commitments, trust, and ethical responsibilities. While veracity focuses on truthfulness, fidelity requires that nurses keep promises, honor agreements, and maintain integrity in all aspects of care. Together, these principles reinforce ethical behavior, strengthen the nurse-patient relationship, and foster trust within the healthcare team.
Key aspects of fidelity and veracity in nursing include:
- Maintaining honesty and trust: Nurses uphold veracity by providing truthful information and fidelity by following through on professional promises.
- Supporting ethical nursing practice: Fidelity ensures that nurses act consistently in alignment with institutional policies, professional standards, and patient expectations.
- Enhancing patient-centered care: Patients are more likely to trust nurses who demonstrate both truthfulness and reliability, which promotes adherence to care plans and improves outcomes.
Example: A nurse promises a patient to provide updates regarding test results by a specific time. Following through on this commitment demonstrates fidelity, while sharing the actual results truthfully demonstrates veracity. Both principles work together to build trust and support ethical nursing practice.
Seven Ethical Principles in Nursing
Veracity is one of the seven core ethical principles in nursing, which guide professional conduct and inform clinical decision-making. Understanding its relationship with other principles helps nurses navigate complex ethical situations and provide care that is patient-centered, transparent, and ethically sound.
The seven ethical principles in nursing include:
- Autonomy: Respecting the patient’s right to make decisions based on truthful, comprehensive information. Veracity empowers patients to exercise autonomy in their healthcare choices.
- Beneficence: Acting in the patient’s best interest by providing honest guidance and care that maximizes benefit.
- Nonmaleficence: Avoiding harm while delivering truthful information, carefully balancing disclosure with patient safety.
- Fidelity: Maintaining commitments, trust, and professional promises while being honest and transparent.
- Justice: Ensuring fairness in providing information and access to care, including equitable communication with all patients.
- Veracity: Truth-telling in all aspects of nursing care, promoting transparency and ethical integrity.
- Accountability: Taking responsibility for one’s actions, including honest reporting of errors, accurate documentation, and adherence to ethical standards.
Example in Practice: A nurse caring for a patient with multiple comorbidities must provide truthful explanations of the risks associated with treatment options (veracity), ensure the patient’s choices are respected (autonomy), recommend interventions that benefit the patient (beneficence), avoid unnecessary harm (nonmaleficence), and follow through on promises to monitor symptoms or provide updates (fidelity). By integrating all seven principles, nurses ensure ethical, high-quality care that aligns with professional standards.
Addressing Challenges and Lack of Veracity in Nursing Practice
Recognizing Lack of Veracity in Nursing
Despite its foundational role in nursing ethics, veracity can be compromised in clinical settings, sometimes intentionally, other times due to systemic pressures. Recognizing instances of lack of veracity in nursing is critical for maintaining ethical standards and ensuring patient-centered care.
Situations where honesty may be compromised include:
- Communication Breakdowns Among Healthcare Professionals: Errors in reporting vital patient information or miscommunication during handoffs can create scenarios where truthfulness is not fully maintained. For example, if a nurse inaccurately documents a patient’s allergy or fails to disclose changes in lab results, this undermines veracity in nursing practice.
- Institutional or Policy Pressures: Sometimes, organizational culture may inadvertently encourage withholding information from patients to avoid complaints or reduce perceived risk. For instance, a unit may discourage full disclosure of errors to prevent liability, which creates an ethical conflict for nurses.
- Family or Patient Requests: Families occasionally request that nurses withhold information from the patient to prevent emotional distress. While well-intentioned, complying with such requests without ethical consideration can lead to lack of veracity and compromise patient autonomy.
- Inconsistent Adherence to Ethical Standards: Nurses under high workload, burnout, or inadequate training may unintentionally fail to practice veracity, such as by glossing over critical details during informed consent discussions or documentation.
Recognizing these situations allows nurses to proactively address ethical challenges and reinforce truthfulness as a core principle in nursing care.
Steps to Uphold Veracity in Nursing Career
Maintaining veracity in nursing practice requires active strategies that integrate ethical principles, professional accountability, and advocacy. Nurses can uphold veracity throughout their nursing career by employing the following approaches:
- Advocacy for Patients: Nurses serve as patient advocates by ensuring that all information shared is truthful and transparent. This includes communicating risks, benefits, and alternatives in a manner that enables patients to make informed decisions.
- Reporting Ethical Breaches: When encountering situations where colleagues or systems compromise veracity, nurses must take action by documenting the issue, notifying supervisors, or consulting ethics committees. For example, if a nurse observes a team member providing misleading information about treatment options, the nurse has an ethical obligation to intervene.
- Utilizing Ethical Frameworks: Applying professional frameworks such as the ANA Code of Ethics, principles of autonomy, beneficence, nonmaleficence, and institutional guidelines ensures nurses make decisions that uphold core ethical standards even in complex or pressured environments.
- Continuous Ethical Reflection: Nurses should regularly evaluate their practice, reflecting on instances where veracity might be compromised and identifying opportunities to strengthen truthfulness, honesty, and ethical integrity.
Example: A nurse discovers that a patient’s lab results were delayed and could influence treatment timing. By promptly informing the patient and collaborating with the healthcare team to correct the situation, the nurse demonstrates commitment to veracity, protects patient safety, and reinforces professional integrity.
Sustaining Core Ethical Standards in Nursing Programs
Long-term adherence to veracity in nursing is reinforced through structured nursing education and professional development programs. Nursing programs and ongoing training focus on cultivating ethical practice, emphasizing the importance of truthfulness and fidelity in clinical care.
Key strategies include:
- Ethics Curriculum Integration: Nursing programs incorporate nursing ethics, ethical principles of nursing, and professional codes into their curriculum. Students learn to apply veracity alongside principles like autonomy, beneficence, nonmaleficence, and fidelity, ensuring they understand both theory and practice.
- Simulation and Case-Based Learning: Practical exercises, such as simulated patient scenarios, allow nursing students to practice veracity in nursing practice, navigating ethical dilemmas such as balancing disclosure with patient safety.
- Mentorship and Role Modeling: Experienced nurses and clinical instructors demonstrate how to uphold veracity in real-world settings, highlighting strategies for transparent communication, documentation, and collaboration.
- Continuing Professional Development: Registered nurses and nursing staff are encouraged to attend workshops, ethics rounds, and professional seminars to reinforce ethical practice, develop advanced decision-making skills, and maintain adherence to ethical standards in nursing.
Example: A nursing program may use a scenario where a patient’s family requests nondisclosure of a terminal diagnosis. Students practice strategies to uphold veracity, facilitate informed consent, and maintain ethical integrity, preparing them to navigate similar situations in their future nursing career.
Conclusion
Veracity in nursing is far more than a theoretical concept—it is a core ethical principle that shapes the very foundation of patient care, decision-making, and professional integrity. By consistently practicing veracity, nurses uphold truthfulness, honesty, and transparency, which are essential for fostering trust in the nurse-patient relationship, enabling patients to make informed decisions, and reinforcing the ethical standards of the nursing profession.
Throughout nursing practice, veracity intersects with other ethical principles, including autonomy, beneficence, nonmaleficence, and fidelity, creating a framework for ethical decision-making that balances truth-telling with patient safety and well-being. Nurses encounter complex ethical dilemmas where maintaining veracity requires careful judgment, compassionate communication, and collaboration with the healthcare team to ensure that patients’ rights and interests remain central.
Professional guidance from the American Nurses Association (ANA) and the nursing code of ethics provides nurses with clear expectations and strategies for upholding veracity, while nursing programs and continuing education foster long-term adherence to ethical principles and support the development of ethical competence in real-world practice. By recognizing challenges, addressing lapses in honesty, and embedding truthfulness into daily nursing care, nurses reinforce both patient safety and professional credibility.
Ultimately, veracity in nursing practice is an active commitment that permeates every aspect of the nursing profession—from bedside interactions to interdisciplinary collaboration, documentation, and advocacy. Upholding veracity ensures that care remains patient-centered, ethically grounded, and professionally responsible, strengthening the integrity of the nursing profession and enhancing the quality of patient care across all healthcare settings. For nurses, embracing veracity is not simply a duty—it is a profound expression of respect, compassion, and accountability that defines the essence of ethical nursing practice.
Frequently Asked Questions
What is the ethical principle of veracity in nursing?
The ethical principle of veracity in nursing refers to the obligation of nurses to be truthful, honest, and transparent with patients, families, and the healthcare team. It ensures patients can make informed decisions, fosters trust, and upholds professional integrity in the nursing profession.
What are the 7 ethical principles in nursing?
The seven ethical principles in nursing include:
- Autonomy – respecting the patient’s right to make decisions about their own care.
- Beneficence – acting in the patient’s best interest.
- Nonmaleficence – avoiding harm to patients.
- Justice – providing fair and equitable care.
- Fidelity – maintaining trust, honesty, and professional commitments.
- Veracity – being truthful and transparent in all aspects of nursing care.
- Accountability – taking responsibility for one’s actions and decisions in patient care.
What are some examples of veracity?
Examples of veracity in nursing practice include:
- Truthfully explaining a patient’s prognosis or diagnosis.
- Disclosing test results accurately and in a timely manner.
- Informing patients about all treatment options and potential risks.
- Reporting medical errors honestly to the healthcare team.
Which statement defines the ethical principle of veracity?
Veracity is the ethical obligation of nurses to be truthful and transparent with patients, families, and healthcare professionals, ensuring honesty in all aspects of nursing care and supporting informed decision-making.
