Understanding Nursing Theory: From Middle Range Theories to Common Nursing Practice
In nursing, theory is more than academic exercise—it is the framework that shapes what nurses do, how they think, and why certain practices exist. Nursing theory guides not only what is taught in nursing education, but also what gets done at the bedside, in policy, research, and leadership. Without it, many interventions, care plans, and decisions risk being reactive rather than grounded in a coherent understanding of patient needs, environments, and health outcomes.
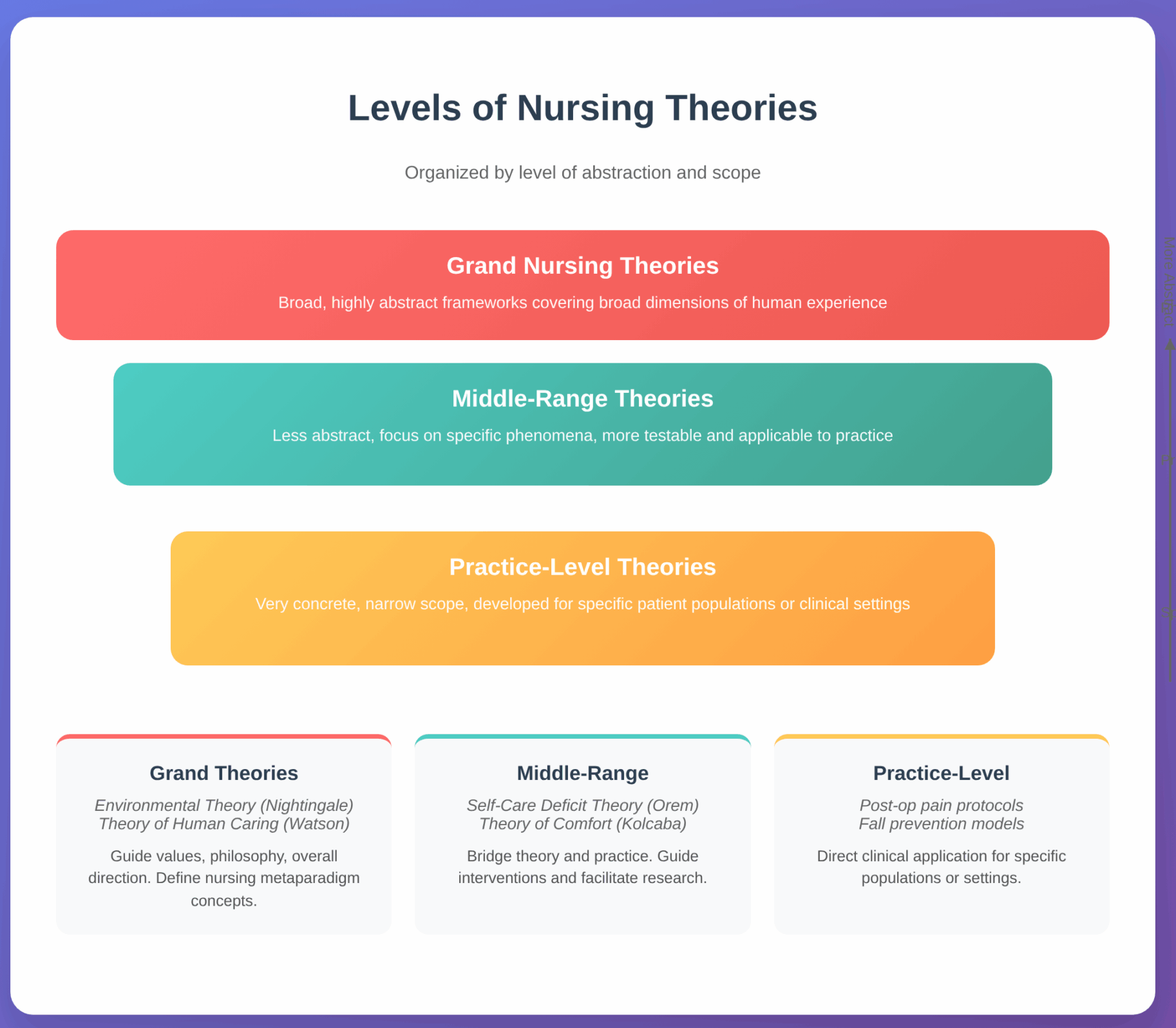
From grand nursing theories that address broad dimensions of human experience, to middle-range nursing theories that focus on more specific phenomena, to practice-level theories (also called low-level or situation-specific) that guide everyday interventions—each level plays a distinct role in the nursing profession. Middle-range theories, in particular, act as bridges: they are concrete enough to inform direct nursing practice and research, yet broad enough to be adaptable to diverse settings.
As students of nursing, becoming familiar with the different levels of theory—what distinguishes them, what their components are, and how they influence real-world nursing care—is essential. Examples like Orem’s Self-Care Deficit Theory or Kolcaba’s Theory of Comfort show how theoretical ideas translate into designing care, assessing patient needs, choosing interventions, and evaluating outcomes. Throughout this article, we will explore what defines different nursing theories, their historical roots, and how middle-range theories can enhance nursing practice, research, education, and patient care.
What Are Nursing Theories and Why Are Nursing Theories Important?
What Defines a Nursing Theory?
A nursing theory is a coherent set of ideas—concepts, definitions, relational statements, and assumptions—designed to describe, explain, predict, or prescribe nursing phenomena. Theories are not just philosophical statements; they serve as structured frameworks that help define what nursing is, what nurses do, and why those things matter.
Some defining features of a theory in nursing include:
- Concepts & phenomena: Key constructs like person, environment, health, nursing (the nursing metaparadigm) are central. Theories often articulate how these concepts interrelate.
- Scope & abstraction: Theories vary in how abstract vs how concrete they are. Some are very broad (grand) and others very narrow (practice-level).
- Purpose (descriptive, explanatory, predictive, or prescriptive): Theories may simply describe phenomena, explain relationships, forecast patient outcomes, or guide interventions and decision-making.
- Testability & usefulness: Good theories allow for empirical verification (through nursing research), meaningful application in nursing care, and generalizability or adaptability. Theories that are too vague or abstract may be difficult to operationalize.
- Testability & usefulness: Good theories allow for empirical verification (through nursing research), meaningful application in nursing care, and generalizability or adaptability. Theories that are too vague or abstract may be difficult to operationalize.
Understanding Nursing Theory and Why Are Nursing Theories are Important?
Nursing theories are essential in multiple interrelated ways:
- Provide a foundation for nursing practice and action
Theories give nurses and nurse theorists a logical framework to decide what to do in patient care, how to design a care plan, and how interventions should be chosen. For example, Dorothea Orem’s Self-Care Deficit Theory helps nurses determine when patients can be expected to care for themselves and when nursing interventions based on support, education, or assistance are needed. - Define the nature and scope of the discipline (nursing profession and nursing science)
Theories help delineate what is uniquely nursing—what distinguishes it from medicine, psychology, or social work. They clarify values, goals, and roles of nurses, thereby supporting identity, scope of practice, and expectations. - Guide nursing education and curriculum development
Nursing students learn models and theories in school so they can link what they learn theoretically to real patient situations. For instance, the nursing metaparadigm (person, environment, health, nursing) is incorporated into many courses so students see how these abstract concepts translate into care decisions. - Enable evidence-based practice and nursing research
Theories help researchers and clinicians generate hypotheses, structure studies, interpret data, and generalize findings. Middle-range theories particularly are useful in research because they are focused enough for measurable outcomes while still theoretically grounded. - Improve communication, consistency, and quality of care
Having shared frameworks and theory-driven models means that nurses across different settings can communicate more clearly about what should be done, why, and under what conditions. This helps in planning, documenting, and evaluating care. Theories also inform nursing interventions and guide decisions in complicated or novel situations. - Shape policy, leadership, and the future of the field
Grand nursing theories, for example, influence policy, ethics, and high-level strategic priorities. When nursing theory is strong, the discipline commands more respect, autonomy, and clarity in what the role of nursing should be.
How Do Nursing Theories Influence Practice?
Here are ways in which theory translates into day-to-day nursing practice, with examples:
- Assessment and care planning: Theories shape what data nurses collect and how they prioritize. For example, using Self-Care Deficit Theory, a nurse assesses which self-care requisites a patient can fulfil and where deficits exist. The care plan then may include education, assistance, or environmental modification.
- Choosing interventions: Theories help choose which interventions are likely to be effective. Under Kolcaba’s Theory of Comfort (a middle-range theory), nurses might focus on improving environmental comfort and emotional support when physical pain cannot be completely alleviated.
- Evaluating outcomes: Because theories include propositions (e.g. if X intervention, then Y result) or predicted relationships, they help nurses judge whether the interventions have succeeded. For example, in mental health nursing, Theory of Interpersonal Relations (Peplau) helps evaluate how nurse–patient interaction contributes to patient anxiety reduction or adjustment.
- Consistency and standardization: When practice is guided by theory, similar patient problems lead to similar intervention patterns (with adaptations). This supports quality assurance, documentation, and best-practice protocols.
- Innovation and adaptation: Theories allow nurses to adapt practices for new situations. For instance, middle-range theories may be tested for different patient populations or cultural contexts (transcultural nursing theory, for example) leading to innovation in care models.
- Ethical and holistic care: Theories remind nurses to consider more than physical symptoms. For example, many grand theories and conceptual models integrate the environment, interpersonal relationships, spirituality, and other dimensions, so care becomes more holistic.
What Are the Different Levels of Nursing Theories?
Nursing theories are commonly organized according to their level of abstraction or scope. The three main levels are:
| Level | Description | Examples | Characteristic Use |
|---|---|---|---|
| Grand Nursing Theories | Broad, highly abstract frameworks; often philosophical; they cover broad dimensions of the discipline and human experience. These theories are not easy to test directly. | Environmental Theory (Florence Nightingale), Theory of Human Caring (Jean Watson) | Useful for guiding values, philosophy, overall direction in care and education. They inform how nursing defines person, health, environment, and nursing in the metaparadigm. |
| Middle-Range Theories | Less abstract; narrower than grand theories; focus on specific phenomena or concepts; more testable, more directly applicable to practice and research. | Self-Care Deficit Theory (Dorothea Orem), Theory of Comfort (Kolcaba) | Serve as bridges between theory and practice; guide nursing in interventions, facilitate research, adaptable to various contexts. |
| Practice-Level (Low-Level) Theories | Also called practice-level or situation-specific theories; very concrete, narrow in scope; often developed for particular patient populations or clinical settings. | For example, a unit-based protocol developed to reduce post-operative pain in a specific hospital ward; or practical models addressing fall prevention in elderly care. (Less grand in name, more specific in use.) |
What Are Low-Level Nursing Theories in Nursing Care?
Low-level nursing theories (also called practice-level or situation-specific theories) are narrowly focused frameworks that describe, explain, or prescribe nursing approaches for particular patient populations, conditions, or clinical problems. Their level of abstraction is low: they are concrete, context-sensitive, and intentionally limited in scope so that they can be applied directly to bedside decision-making, unit protocols, and outcome evaluation. These theories often arise out of clinical observation, practice innovation, or targeted research and are designed to be readily testable and adaptable to local settings.
What Characteristics Define Low-Level Nursing Theories?
Practice-level theories characteristically:
- Have a low level of abstraction — they focus on specific, observable phenomena rather than broad philosophical ideas.
- Address context and population: they explicitly define the clinical setting (e.g., adult medical-surgical unit, neonatal ICU) and the group of patients or the phenomenon (e.g., postoperative pain, catheter-associated urinary tract infection).
- Emphasize actionable propositions: they describe which specific nursing interventions are likely to influence clearly defined outcomes.
- Are closely tied to research and quality improvement: they are often developed from local data, pilot studies, or translational research and can be tested with measurable indicators.
- Limit generalizability deliberately — the goal is useful guidance for defined situations rather than universal claims.

How Do Low-Level Theories Impact Daily Nursing Practice and Nursing Problems?
Practice-level theories translate theory into concrete steps nurses can follow. Their effects on day-to-day care include:
- Focused assessment: These theories specify what data to collect. For a practice-level pain model this might include pain intensity, functional limitations, analgesic side effects, and sleep disruption — data that directly inform immediate interventions.
- Targeted interventions: Because practice theories propose specific links between intervention and outcome, nurses can choose interventions with plausible, evidence-based effects — e.g., multimodal analgesia plus early mobilization as a bundled approach for post-op pain.
- Outcome measurement and evaluation: Clear, narrow outcomes (e.g., numeric pain score reduction, decreased opioid consumption, time to mobilization) make it possible to evaluate whether an intervention worked and to iterate quickly.
- Local protocol development: Practice theories often become the theoretical basis for unit protocols, checklists, or order-sets (for instance, a pressure-injury prevention bundle tailored to a surgical ward).
- Interprofessional clarity: When nurses use situation-specific frameworks, they can communicate rationale and expected outcomes more clearly to physicians, therapists, and managers, improving coordination of care.
Brief case example (applied): An orthopaedic ward identifies high rates of delayed ambulation after hip arthroplasty. A small mixed-methods study on that unit develops a practice-level model linking early multimodal analgesia, targeted physiotherapy within 12 hours, and discrete patient education to earlier ambulation and shorter length of stay. The unit transforms that model into a protocol, collects immediate outcome data (time to first walk, pain scores), and modifies the protocol based on real-time feedback. This is a classic example of a low-level theory informing practical change.
Can You Provide Examples of Low-Level Nursing Theories?
Because low-level theories are often developed for local problems, many examples are embedded in practice literature rather than classic textbooks. Representative illustrations include:
- Unit-based symptom-management models — e.g., a model for chemotherapy-related nausea on an oncology unit that links timing of antiemetics, hydration status, and nonpharmacologic coping strategies to patient-reported nausea scores.
- Postoperative pain management bundles that specify assessment intervals, multimodal analgesic regimens, and mobility targets (effectively a practice theory for post-op recovery).
- Fall-prevention algorithms created for a specific hospital ward that combine risk screening, environmental checks, hourly rounding, and mobility aids into a testable protocol. (Such algorithms are situation-specific theories when they explicitly state causal links between interventions and fall rates.)
- Symptom-cluster models in palliative or oncology care that guide focused assessment and bundled interventions for fatigue-anorexia-cachexia syndromes.
How to Use a Low-Level Theory at the Bedside (Practical Steps)
- Define the phenomenon and population clearly (who, where, when).
- Specify measurable outcomes (what success looks like).
- Choose interventions supported by local evidence or relevant middle-range theory (why these interventions are expected to work).
- Implement with simple data collection (pre/post measures, run charts).
- Evaluate and refine — if outcomes aren’t met, re-examine assumptions, measurement, and fidelity.
This pragmatic cycle (define → act → measure → refine) makes practice-level theories “ready-to-wear” tools for improving care in specific clinical contexts.
What Are Middle Range Nursing Theories in Model of Nursing?
Middle-range nursing theories represent a level of abstraction between broad grand nursing theories and highly specific practice-level nursing theories. They were developed to provide more specific nursing practice guidance than could be drawn from abstract concepts like “human adaptation” or “the environment.” These theories focus on clearly defined aspects of the field of nursing, often addressing particular patient experiences, clinical problems, or aspects of the nursing metaparadigm.
Because they are more concrete, middle-range nursing theories are widely used in nursing education, clinical settings, and nursing research. They enable nurses to evaluate patient needs, predict responses, and design interventions. For example, Kolcaba’s Theory of Comfort gives nurses a structured way to assess patient comfort across physical, environmental, sociocultural, and psychospiritual domains, which can then guide a nursing care plan.
What Makes Middle-Range Theories Unique In The Types of Nursing Theory?
What distinguishes middle-range theories from grand theories or situation-specific theories is their level of abstraction. They are not so broad that they become purely philosophical, nor so narrow that they apply only to a single clinical case. Instead, they address nursing phenomena that are common enough to apply across different nursing populations but still concrete enough to guide measurable outcomes.
For instance, Orem’s Self-Care Deficit Nursing Theory is often classified as a broader theory of nursing, but components of it function as middle-range applications. Nurses can use it to identify when a patient is unable to perform self-care, then intervene with teaching, monitoring, or direct assistance. Similarly, the Theory of Chronic Sorrow by Eakes, Burke, and Hainsworth is unique because it explores an ongoing, lived experience—recurring grief in families of children with disabilities—that had been overlooked in earlier grand models in nursing.
How Do Middle-Range Theories Bridge the Gap Between Theory and Practice?
One of the persistent criticisms of theories developed at the grand level is that they can feel too abstract for frontline nurses. Middle-range theories address this gap by providing concepts that can be operationalized into measurable variables for both research and nursing interventions.
For example, in psychiatric mental health nursing, Peplau’s Theory of Interpersonal Relations—often cited as the first nursing theory to emphasize relationships—works well at the middle range because it offers clear roles (stranger, teacher, counselor, resource) that nurses can assume in the therapeutic process. This theoretical framework informs how nurses conduct assessments, establish trust, and deliver care, making it easier to guide nursing practice.
Similarly, Kolcaba’s Theory of Comfort bridges theory and practice by showing that patient comfort is not just a desirable outcome but a measurable variable tied to healing and satisfaction. Nurses can design a care theory-based intervention such as creating a quiet environment for postoperative patients and then evaluate the outcome through patient feedback.
By guiding both bedside practice and nursing research, middle-range theories create a cycle: theories guide interventions, interventions generate outcomes, and outcomes feed back into refining the theory. This illustrates how theory and practice are inseparable in the art and science of nursing.
What Are Some Prominent Middle-Range Nursing Theories?
Several middle-range theories have become foundational to nursing knowledge and remain widely used in both academic and clinical settings:
- Kolcaba’s Theory of Comfort – Focuses on holistic comfort and its impact on health-seeking behaviors. Widely applied in palliative care and oncology nursing.
- Meleis’ Transition Theory – Explores the processes individuals experience during health-related or developmental transitions, such as adolescence, menopause, or end-of-life care. Nurses use this to anticipate patient needs during major life changes.
- Pender’s Health Promotion Model – A model of nursing that operates at the middle-range level by examining behaviors that improve wellness and prevent illness. Nurses apply this in community health programs and health education campaigns.
- Reed’s Theory of Self-Transcendence – Explains how patients expand personal boundaries during times of vulnerability, especially in gerontology and hospice care.
- Theory of Chronic Sorrow (Eakes, Burke, & Hainsworth) – Provides a framework for understanding ongoing grief, helping nurses design interventions for families experiencing long-term caregiving stress.
- Peplau’s Theory of Interpersonal Relations – While originally considered broader, it functions as a practical middle-range theory in nursing practice, offering structured roles and phases for therapeutic nurse-patient interactions.
What Are High-Level Nursing Theories?
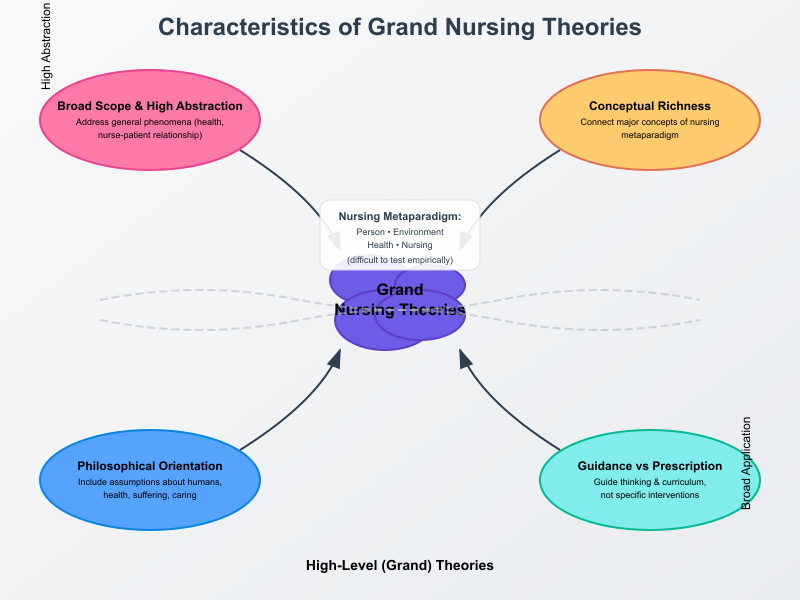
High-level nursing theories — often called grand theories or grand nursing theories — are broad, highly abstract conceptual frameworks that define the scope, values, and major concepts of the discipline. Rather than offering step-by-step instructions for bedside tasks, these theories articulate wide-ranging propositions about personhood, health, environment, and the role of nursing. They shape how the profession thinks about what it does and why, providing a philosophical and conceptual foundation for other levels of theoretical work (middle-range and practice-level).
What Characteristics Define High-Level Nursing Theories?
Grand theories share several defining characteristics:
- Very broad scope and high abstraction. They address general phenomena (for example, what constitutes health or the nurse–patient relationship) rather than narrowly defined clinical problems. Because of this abstraction, grand models are often difficult to test directly using standard empirical methods.
- Conceptual richness. Grand theories introduce and connect major concepts that form the backbone of the nursing metaparadigm (person, environment, health, nursing). These conceptual connections help define the identity of the discipline and clarify its unique perspective among health professions.
- Philosophical orientation. Many grand theories include philosophical assumptions about the nature of humans, health, suffering, or caring; they therefore influence ethical frames and how nurses interpret clinical situations.
- Guidance rather than prescription. Because they are general, grand theories guide thinking and curriculum rather than prescribe specific nursing interventions or protocols; they form the intellectual soil from which more testable, practice-oriented theories grow.
How Do High-Level Theories Inform Nursing Education and Policy?
Grand theories exert influence across three principal domains relevant to students, educators, and leaders:
- Curriculum and pedagogy. Faculty commonly use grand models to frame program philosophy and course sequencing. For example, a curriculum built on a caring paradigm will prioritize therapeutic communication, reflective practice, and relational assessment throughout its coursework. This helps ensure students graduate with a coherent conceptual lens rather than a set of disjointed clinical skills.
- Professional identity and standards. By defining core concepts (who we care for, what health means, and what constitutes nursing action), grand theories inform professional statements, competencies, and core expectations used by regulatory and professional bodies. These conceptual anchors support uniformity in scope-of-practice discussions and license/certification standards.
- Policy, systems design and public health orientation. Historically, grand theoretical ideas have shaped large-scale changes: Florence Nightingale’s environmental emphasis helped catalyze sanitation, hospital design, and early public-health policy reforms; later grand frameworks influenced how care delivery models and quality standards were conceptualized at institutional and national levels. In short, grand theories help leaders translate nursing’s values into organizational priorities and policies.
What Are Notable Examples of High-Level Nursing Theories and Nursing Theorist?
Below are widely cited grand theories, with a note on their defining contribution:
- Florence Nightingale – Environmental (or “Nightingale”) Theory: One of the earliest grand frameworks, Nightingale linked environmental factors (clean air, sanitation, light, diet) to recovery and public-health reform. Her ideas influenced hospital design, infection-control thinking, and the early professionalization of nursing.
- Jean Watson – Theory of Human Caring (Carative Factors / Transpersonal Caring): Watson’s grand framework centers caring relationships, humanistic values, and the moral/ethical dimensions of nursing. It has strongly influenced curricula that emphasize relational care, reflective practice, and patient dignity.
- Sister Callista Roy – Roy Adaptation Model: Roy’s model conceptualizes the person as an adaptive system and defines nursing as an intervention that promotes adaptive responses. It has been influential in shaping assessment frameworks and education for nurses caring for patients with chronic and complex conditions.
- Rosemarie Rizzo Parse – Theory of Human Becoming: Parse’s philosophical, existential approach reframes health and quality of life as lived experiences; it has contributed to curricula that foreground person-centred meaning and narrative approaches in care.
- Imogene King / Other grand models (e.g., King’s Goal Attainment, Neuman’s Systems Model): These models provide broad conceptual systems for understanding client–nurse interactions and systemic stressors, and they continue to inform program design and leadership thinking.
Note on classification: Some historically important frameworks (for example, Orem’s Self-Care Deficit ideas) are classified differently by authors (grand vs middle-range), and classification can depend on how the theory is used in practice or education. The point is not rigid labeling but understanding whether the theory functions at a broad, philosophical level (grand) or a more testable, intervention-focused level (middle-range).
How Do Middle-Range Nursing Theories Enhance Nursing Practice?
Middle-range nursing theories enhance day-to-day clinical work by translating abstract ideas into usable concepts, measurable variables, and testable relationships that directly inform assessment, intervention and evaluation. Because they occupy the space between grand nursing theories and situation-specific models, middle-range theories give clinicians a practical language and structure for solving problems that recur across patient groups and settings.
Practical impact examples
- Assessment focus. Kolcaba’s Theory of Comfort asks nurses to assess physical, psychospiritual, environmental and sociocultural sources of discomfort — this focused assessment yields data that directly determine which nursing interventions to prioritize (e.g., repositioning, environmental modifications, spiritual support). Research mapping interventions grounded in comfort theory has demonstrated consistent improvements in reported comfort and related outcomes.
- Intervention selection. Orem’s Self-Care Deficit ideas help nurses identify specific self-care capabilities and deficits (mobility, nutrition, medication management) and then select teaching, assistive devices or direct care as appropriate; randomized and quasi-experimental studies show self-care education based on Orem improves quality of life and self-management in chronic conditions.
- Program design. Pender’s Health Promotion Model has been used to design community and primary care programs (smoking cessation, dietary change, breastfeeding support) by identifying determinants of health-promoting behaviors and targeting them in interventions; systematic reviews and integrative studies document its utility in diverse primary-care interventions.
What Role Do Middle-Range Theories Play in Evidence-Based Practice?
Middle-range theories are central to evidence-based nursing because they:
- Generate testable hypotheses. Their clearly defined concepts and relationships make it possible to design studies that evaluate specific interventions or mechanisms (for example: “If nurses implement a comfort bundle, then patient sleep quality will improve”). This bridges conceptual reasoning and empirical testing.
- Provide conceptual frameworks for study design and measurement. Middle-range constructs become variables, guiding selection of instruments, timing of measurement, and definition of outcomes (e.g., comfort scales, self-care ability indices). This improves the rigor and interpretability of nursing research.
- Support translation of research into practice. When studies grounded in middle-range theories show benefit (for example, comfort-based interventions reducing pain or anxiety), those findings can be more readily adapted into protocols and care plans because the mechanisms and target constructs are already explicit. Systematic mappings of Kolcaba-based interventions, and multiple trials applying Orem’s principles, illustrate how mid-range theory–driven evidence accumulates and becomes practice guidance.
How Can Nurses Integrate Middle-Range Theories into Their Nursing Care Plan?
Integration is practical and follows a reproducible process. Below is a stepwise approach with examples:
- Select an appropriate theory for the problem. Match the phenomenon (pain, comfort, self-care, transition) to a middle-range theory (e.g., Theory of Comfort for symptom relief; Self-Care Deficit for chronic disease education).
- Operationalize key concepts. Define measurable indicators for the theory’s constructs (e.g., comfort → numeric comfort scale; self-care ability → ADL checklist). Use validated instruments when available.
- Design interventions aligned with the theory. Choose nursing interventions that logically follow from the theory (Kolcaba → establish quiet time, control lighting, offer relaxation; Orem → tailored self-care teaching modules). Pilot the intervention to test feasibility.
- Embed theory in the nursing process and documentation. Integrate theory-based assessment templates and nursing care plans so that interventions and expected outcomes are recorded in a consistent, auditable way (e.g., a comfort care plan with intervention-outcome pairs).
- Collect outcomes and evaluate. Use pre/post measures, run charts, or small trials to evaluate whether the theory-based intervention produces the predicted change. If outcomes align with predictions, scale up; if not, refine the operational definitions or intervention fidelity.
- Share findings and iterate. Publish QI reports, present at staff meetings, and incorporate lessons into unit protocols so the practice-level theory informed by mid-range constructs becomes sustainable.
Concrete example (integration in practice): An oncology unit adopts Kolcaba’s Theory of Comfort to reduce chemotherapy-related nausea. Nurses operationalize comfort (physical: nausea intensity; psychospiritual: anxiety score), implement an intervention bundle (timed antiemetics + relaxation training + environmental control), and track outcomes. Demonstrated reductions in nausea scores lead to formal protocol adoption and staff training cycles.
What Benefits Do Middle-Range Theories Offer Patients and Healthcare Systems in Deliberative Nursing Process?
For patients
- Improved outcomes that matter to patients. Theory-driven interventions frequently target patient-centered outcomes (comfort, self-management, reduced symptom burden). Reviews and trials show measurable improvements (comfort levels, quality of life, self-care competence).
- More holistic and consistent care. Middle-range theories often require attention to multiple domains (physical, emotional, social), producing more comprehensive care that aligns with patient preferences and psychosocial needs.
For healthcare systems
- Better standardization and reproducibility. Because middle-range theories define mechanisms and measurable outcomes, they allow services to create protocols that are replicable across units and facilities — improving reliability of care.
- Stronger linkage between practice and research. Theories support practice-based evidence: interventions that are theory-driven are easier to evaluate and scale when proven effective, shortening the research-to-practice pipeline.
- Potential cost and efficiency gains. When theory-based interventions reduce symptom burden, readmissions, or length of stay (for example, effective self-care education reducing uncontrolled hypertension complications), systems can realize downstream savings; while direct cost-effectiveness analyses are still emerging, many clinical studies report resource gains (shorter LOS, fewer complications) when interventions are grounded in tested middle-range models.
- Professional development and accountability. Embedding theory in care plans and documentation strengthens clinical reasoning, makes nursing contributions visible, and supports quality assurance and accreditation processes.
What Challenges Are Associated with Nursing Theories in the History of Nursing?
While nursing theories are critical to advancing the nursing profession, they present challenges in terms of application, adaptation, and acceptance. One major challenge is the level of abstraction in many grand nursing theories. These broad frameworks are valuable for shaping the foundation for nursing, but they are often too theoretical and lack the concrete steps that nursing students or clinicians need in daily nursing practice. For example, Florence Nightingale’s Environmental Theory introduced the importance of sanitation and environment in health, yet modern healthcare complexities like technology integration or chronic disease management require more specific frameworks.
Another challenge is the gap between theory and practice. While nursing theories provide a framework for understanding nursing phenomena, frontline nurses often feel pressured by heavy workloads, limited resources, and time constraints, leaving little room for applying theoretical frameworks in decision-making. In addition, the diverse types of nursing theories—from practice-level nursing theories to middle-range nursing theories—can make it difficult for practitioners to determine which model best fits a particular patient situation.
Lastly, the history of nursing shows that some theories, such as Henderson’s Need Theory or Peplau’s Theory of Interpersonal Relations, were developed decades ago. While still foundational, they may not fully address modern issues like cultural diversity, advanced technology, or evolving population health needs. This creates tension between preserving classical ideas and adapting to contemporary demands in the field of nursing.
What Barriers Do Nurses Face in Applying Common Nursing Theories?
There are several practical barriers:
- Limited education and training. Many nursing school curricula introduce nursing philosophies and theoretical models, but students often report difficulty translating these concepts into specific nursing practice once in clinical settings. New graduates may feel unprepared to use theories to guide nursing practice.
- Organizational culture and priorities. Healthcare institutions frequently emphasize efficiency, cost-saving, and task-oriented nursing care over theory-driven decision-making. For instance, using Kolcaba’s Theory of Comfort to design holistic interventions may conflict with time-limited protocols.
- Complexity of theories. Some nursing model frameworks are perceived as abstract or overly complex, making them less appealing for busy clinicians. The theory of chronic sorrow or Casey’s Model of Nursing requires deep reflection and adaptation, which may be difficult in high-stress environments like mental health nursing or emergency care.
- Lack of support for nursing research. To evaluate and refine theories, nursing research is essential. However, limited funding, staffing shortages, and insufficient support for scholarly work hinder the continuous validation and development of theories are essential to advancing nursing science.
How Can Nurses Overcome These Challenges?
Nurses and educators can adopt strategies to bridge theory and practice:
- Integrating theory into the nursing process. Embedding frameworks such as Orem’s Self-Care Deficit Nursing Theory or Leininger’s Transcultural Nursing Theory into care pathways and nursing care plans ensures theory directly informs patient assessment, interventions, and evaluation.
- Strengthening nursing education. Nursing programs should teach not only theories describe but also how to apply them in simulations and clinical rotations. For instance, students can practice Peplau’s therapeutic communication techniques in simulated psychiatric settings.
- Organizational support. Hospitals and clinics can promote understanding of nursing theories by including them in policies, documentation systems, and quality improvement projects. This creates a culture where theory was developed into practical tools that help nurses make consistent, evidence-based decisions.
- Encouraging reflective practice. Reflection sessions allow nurses to analyze patient cases through theoretical lenses, reinforcing how theories guide nursing and enhance critical thinking. For example, debriefing after a case using Kolcaba’s model highlights holistic dimensions of care that might otherwise be overlooked.
- Investing in nursing research. Expanding research on modern nursing challenges, such as digital health or population-based care, helps refine situation-specific theories that address emerging issues.
What Future Trends Are Emerging in Nursing Theory Development?
The future of theory in nursing points toward adaptation, integration, and innovation:
- Expansion of situation-specific theories. As healthcare becomes more specialized, theories are narrower in scope but highly applicable. For example, the theory of chronic sorrow continues to evolve for families coping with long-term illness, and newer models are being tailored for palliative and geriatric care.
- Integration of technology. With electronic health records and AI decision-support tools, nursing systems are increasingly data-driven. Future nursing theories important will likely incorporate technology into frameworks for patient safety, remote monitoring, and predictive analytics.
- Global and cultural perspectives. The growth of transcultural nursing highlights the importance of culturally competent nursing interventions. As globalization increases, theories like Leininger’s will expand to address multicultural, migrant, and refugee health contexts.
- Interdisciplinary collaboration. New models in nursing science are expected to integrate insights from psychology, sociology, and public health, creating comprehensive frameworks that respond to complex nursing problems and social determinants of health.
- Theory as a framework for policy. Policymakers are increasingly recognizing how nursing theories help justify practice standards, staffing models, and patient safety initiatives. Future trends may include aligning nursing ideas with health policy to strengthen the visibility of the art and science of nursing in shaping healthcare systems.
Conclusion: Why Understanding Nursing Theories Is Essential for Nursing Students
Nursing theories form the intellectual backbone of the nursing profession, shaping how nurses define their roles, understand patient needs, and deliver holistic nursing care. From the early contributions of Nightingale’s Environmental Theory to the development of middle-range nursing theories like Kolcaba’s Theory of Comfort or Peplau’s Theory of Interpersonal Relations, the evolution of theoretical frameworks demonstrates the ongoing effort to unify the art and science of nursing. These theories are not abstract academic exercises; they provide a foundation for nursing practice, education, and research, helping to clarify what makes nursing unique within the healthcare system.
At every level of abstraction, theories serve different but complementary purposes. Grand nursing theories establish broad philosophical perspectives and articulate the values of the nursing metaparadigm, while middle range theories provide practical, evidence-based strategies for clinical care, and practice-level nursing theories translate those ideas into concrete steps in the nursing process. Together, they create a continuum that connects theory and practice, ensuring that every nursing intervention rests on a solid conceptual base.
For nurses in training, developing an understanding of nursing theories is more than an academic requirement—it is preparation for real-world challenges. When nursing students learn how the Self-Care Deficit Nursing Theory or the Theory of Chronic Sorrow applies to patient experiences, they build a mindset that goes beyond task-oriented care. This mindset enables them to critically analyze patient situations, create individualized nursing care plans, and contribute to advancing nursing knowledge.
In clinical settings, theories offer tools to guide nursing practice and improve outcomes. For example, using transcultural nursing theory helps nurses deliver culturally sensitive care, while applying Pender’s Health Promotion Model supports preventive health in community settings. Theories not only help nurses structure decision-making but also give them a common professional language to advocate for resources, design research, and influence policy.
The challenges of applying theory—such as limited time, organizational barriers, or perceptions of complexity—are real. Yet these can be addressed through stronger integration of theory into nursing education, ongoing reflective practice, and institutional support for nursing research. As healthcare evolves, so too must theoretical frameworks, with future trends pointing toward situation-specific theories, technology integration, and interdisciplinary collaboration.
Ultimately, nursing theories are essential because they guide nursing practice, strengthen professional identity, and ensure care is both evidence-based and patient-centered. They remind us that nursing is not only about tasks and procedures but about addressing nursing phenomena in ways that honor the human experience of health and illness. By engaging deeply with theory, nurses safeguard the legacy of the first nursing theory, adapt to the needs of modern nursing, and shape the future of the nursing career as both a scientific discipline and a caring profession.
Frequently Asked Questions
What are the 4 levels of nursing theory?
The four recognized levels are grand nursing theories, middle-range theories, practice-level nursing theories, and situation-specific theories. Grand theories are highly abstract and address broad perspectives of the nursing metaparadigm. Middle-range theories are narrower, addressing specific nursing phenomena relevant to nursing practice. Practice-level theories provide direct guidance for bedside care, while situation-specific theories are even more focused on particular patient populations or contexts.
What are middle-range theories in nursing practice?
Middle-range nursing theories occupy a middle ground between abstract grand theories and concrete practice models. They focus on defined aspects of nursing care—such as comfort, adaptation, or interpersonal relationships—and are designed to help nurses apply theory to measurable outcomes. For example, Kolcaba’s Theory of Comfort and Peplau’s Theory of Interpersonal Relations provide practical frameworks that guide nursing interventions and improve patient outcomes.
How do grand nursing theories differ from middle-range and practice-level nursing theories regarding their scope and application in nursing practice?
Grand nursing theories have the broadest level of abstraction, offering general perspectives on the theory of nursing, such as Orem’s Self-Care Deficit Theory or Roy’s Adaptation Model. They guide overall thinking but may lack immediate applicability. In contrast, middle range theories are narrower in scope, addressing specific nursing problems and linking theory and practice through testable concepts. Practice-level nursing theories are the most concrete, designed for direct application in specific nursing practice, such as creating a nursing care plan for wound care or pain management.
What is the difference between mid range theory and practice theory?
A middle range theory (or mid-range theory) addresses defined but broad aspects of nursing knowledge, such as transitions, comfort, or chronic sorrow, and can be applied across settings. In contrast, a practice theory (or practice-level nursing theory) is narrower, designed to guide a specific nursing intervention or patient care situation. For example, Reed’s Theory of Self-Transcendence is a middle-range theory, while a theory guiding pain management in postoperative care would be classified as a practice-level theory.
