
Transitional Care: Complete Guide to Care Management, Transitional Care Units, and Rehabilitation After Hospital Discharge
Transitional care in nursing is a critical component of modern healthcare, ensuring that patients experience seamless movement across care settings—from hospitalization to home health, rehabilitation facilities, or skilled nursing environments. Just as clinical care pathways guide treatment, transitional care provides a structured approach to coordinating patient care, addressing complex needs, and promoting continuity of care across multiple care settings. Far from being a passive process, effective transitional care in nursing requires deliberate planning, collaboration among healthcare professionals, and engagement of patients and family caregivers to optimize recovery and maintain health outcomes.
At its core, transitional care in nursing focuses on bridging gaps that can occur during hospital discharge and care transitions. This includes coordinating rehabilitation services, managing chronic conditions, and supporting medication management to prevent complications or hospital readmission. Through multidisciplinary collaboration, transitional care helps ensure that patients receive consistent, high-quality care tailored to their individual needs, whether in a transitional care unit, a skilled nursing facility, or during home health visits.
For patients—especially older adults or those with multiple chronic conditions—transitional care in nursing is essential for maintaining functional independence and reducing the risk of adverse events following a hospital stay. Caregivers and family members also play a vital role, as their involvement in discharge planning and ongoing care supports successful recovery and continuity of care.
This guide offers a comprehensive overview of transitional care in nursing, covering the roles of healthcare professionals and caregivers, the structure and function of transitional care units, rehabilitation services, discharge planning, and quality assessment. By understanding the principles and practices of transitional care in nursing, students and healthcare providers can better navigate care transitions, enhance patient outcomes, and contribute to high-quality, coordinated care across the healthcare continuum.
Understanding Transitional Care and Its Role in Continuity of Care
Defining Transitional Care and Transitional Care Services
Transitional Care in Nursing is the structured coordination of patient care as individuals move between different care settings, especially after a hospitalization or period of acute illness. Its primary purpose is to maintain continuity of care, reduce adverse events, and ensure patients receive appropriate support at each stage of recovery. Unlike simple discharge instructions, transitional care services involve a comprehensive approach to preparing patients and caregivers for what comes next in the care continuum.
Transitional care services typically include:
- Assessment of patient needs: Evaluating physical, cognitive, and psychosocial status to identify complex care needs such as multiple chronic conditions. For example, a patient recovering from a stroke may require a functional assessment to determine if home modifications or placement in a rehabilitation facility are necessary.
- Care planning and coordination: Developing individualized care plans that incorporate goals for recovery, medication adherence, and rehabilitation services. This often involves a multidisciplinary team of care providers to ensure that all aspects of recovery are addressed.
- Patient and family education: Preparing patients and family caregivers to manage symptoms, understand medication management, and recognize warning signs. For instance, an older adult discharged after heart failure management may need guidance on daily weight monitoring and when to contact the primary care provider.
- Transition support and communication: Sharing timely information between the acute care team, primary care provider, home health nurses, and rehabilitation staff.
- Monitoring and follow-up: Conducting assessments in the first 30 days after discharge through home visits or telehealth to prevent complications and hospital readmission.
These services ensure that patients experience a smooth transition across care settings, reducing gaps that could compromise safety and recovery.
The Importance of Transitional Care Management
Transitional Care Management (TCM) is the systematic implementation of these principles, ensuring that patients move safely from hospital to home or other care environments. TCM strengthens the interface between hospitalization, home health care, and ongoing primary care by coordinating the efforts of the transitional care team and ensuring individualized attention to each patient’s complex care needs.
Key aspects of TCM include:
- Multidisciplinary collaboration: Effective TCM requires a coordinated care team, including nurses, physicians, social workers, and therapists. Their combined efforts address medical, psychosocial, and functional needs.
- Reducing hospital readmissions: Structured TCM programs have been shown to lower readmission rates and emergency department visits, particularly for patients with multiple chronic conditions.
- Personalized care: TCM provides tailored interventions such as arranging rehabilitation services, reviewing medication management, and offering patient and caregiver education to support recovery.
- Integration across care settings: Information, instructions, and therapy plans are aligned across hospital, rehabilitation facility, and home health care, ensuring continuity of care.
For example, a 75-year-old patient with heart failure and diabetes recovering from a hospitalization may receive:
- A comprehensive assessment of medical, cognitive, and social needs.
- An individualized care plan with scheduled follow-ups, home health visits, and therapy.
- Education for family caregivers on diet, symptom monitoring, and when to seek urgent care.
- Coordination of rehabilitation services in a skilled nursing facility if needed.
- Ongoing monitoring to prevent complications and ensure high-quality transitional care.
Through these measures, transitional care in nursing promotes safer transitions, improved patient outcomes, and reduced healthcare costs by preventing unnecessary hospital readmissions. It demonstrates how effective care coordination across settings can lead to sustained recovery and enhanced patient satisfaction.
The Transitional Care Team and Care Providers
Effective transitional care in nursing relies on a well-structured, collaborative approach where healthcare professionals, family caregivers, and the transitional care team work together to ensure continuity of care. Coordinating care across settings—from hospitalization to home health care, rehabilitation facilities, or skilled nursing facilities—requires clear roles, communication, and collaboration. The goal is to maintain patient safety, optimize recovery, and reduce hospital readmissions and complications during transitions in care.
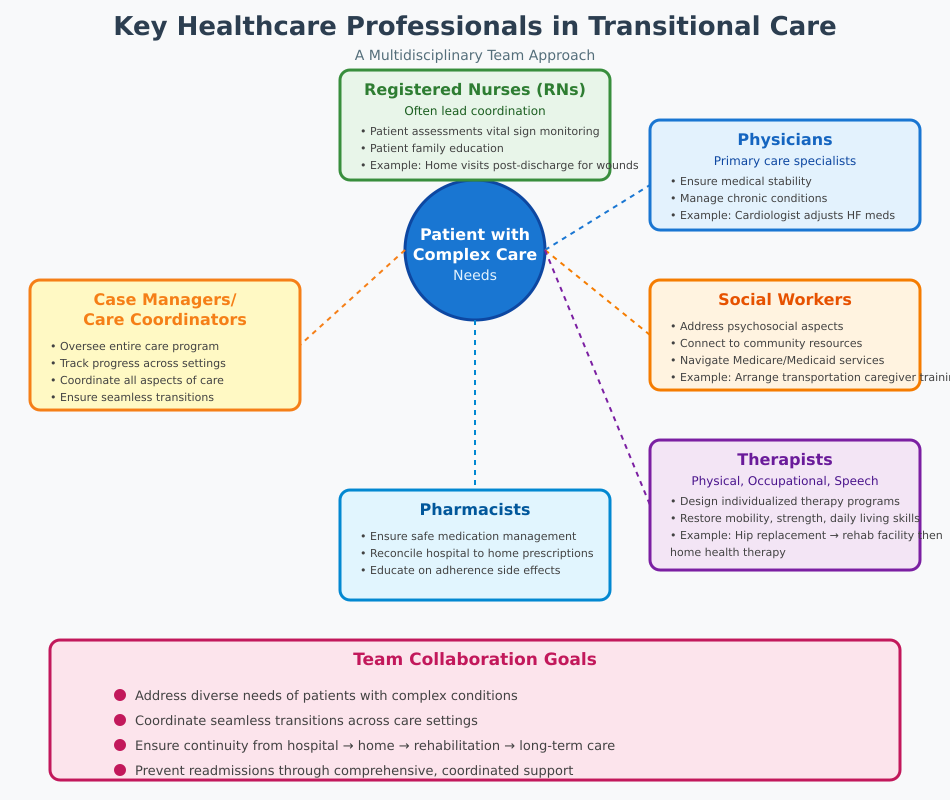
Key Healthcare Professionals in Transitional Care
The transitional care team is multidisciplinary, with each member bringing specialized expertise to address the diverse needs of patients with complex care needs or multiple chronic conditions. Key roles include:
- Registered Nurses (RNs):
RNs often lead the coordination of transitional care services, providing patient assessments, monitoring vital signs, educating patients and family caregivers, and ensuring adherence to care plans. For example, an RN may conduct home visits within the first week after hospital discharge to check wound healing and medication compliance. - Physicians:
Both primary care providers and specialists ensure medical stability, manage chronic conditions, and review medication management plans. For instance, a cardiologist may adjust heart failure medications after reviewing a patient’s hospital stay records and coordinate with home health nurses for follow-up care. - Social Workers:
Social workers address psychosocial aspects, connect patients and families to community resources, and help navigate Medicare or Medicaid services for transitional care management. They may arrange transportation to rehabilitation facilities or support caregiver training. - Therapists (Physical, Occupational, Speech):
Rehabilitation services are critical for patients recovering from acute illness or surgery. Occupational and physical therapists design individualized therapy programs to restore mobility, strength, and daily living skills. Example: After a hip replacement, a patient may attend sessions in a rehabilitation facility before continuing home health therapy under nurse supervision. - Pharmacists:
Pharmacists ensure safe medication management, reconcile prescriptions from the hospital to the home setting, and educate patients and family caregivers on adherence and potential side effects. - Case Managers or Care Coordinators:
These professionals oversee the care program, track progress, and coordinate all aspects of care across care settings, ensuring a seamless transition from hospital to home or transitional care units.
Through multidisciplinary collaboration, these professionals collectively support continuity of care, minimize risks associated with care transitions, and enhance high-quality transitional care outcomes.
Roles of Family Caregivers in Transitional Care
Family caregivers are essential partners in transitional care in nursing. Their involvement significantly influences patient outcomes, especially for older adults or patients with chronic conditions. Key contributions include:
- Supporting Recovery and Rehabilitation:
Family caregivers assist patients with rehabilitation services, help maintain therapy routines, and provide physical support during mobility or occupational therapy exercises at home. - Medication and Symptom Management:
Caregivers monitor adherence to medication management plans, track symptom changes, and alert healthcare providers to potential complications, reducing hospital readmissions. - Facilitating Communication with Healthcare Providers:
Family caregivers often serve as liaisons between patients and the transitional care team, ensuring that instructions, appointments, and updates from home health nurses or primary care providers are followed. - Psychosocial Support:
Beyond physical care, caregivers provide emotional support, encouraging adherence to care plans and helping patients navigate the stress of recovery after hospitalization. - Education and Advocacy:
Family caregivers learn to recognize warning signs, advocate for patient needs, and coordinate care services. For example, a caregiver might request a rehabilitation facility referral if the patient is not meeting recovery milestones at home.
Example Scenario: Mrs. J, an 82-year-old patient recovering from a stroke, is discharged to home health care. The RN provides education on exercises, the occupational therapist sets up home adaptations, and her daughter, the family caregiver, ensures she completes daily exercises, monitors her medication management, and reports any new symptoms to the primary care provider. This coordinated effort minimizes complications and avoids hospital readmission.
Benefits of Transitional Care for Patients and Older Adults
Transitional care in nursing is critical for improving outcomes for patients, particularly older adults and those with chronic conditions. By bridging the gap between hospitalization and home or rehabilitation facilities, transitional care ensures continuity of care, reduces complications, and supports optimal recovery. It encompasses both rehabilitation services and the structured coordination of care transitions, providing a safety net during the vulnerable period following discharge from the hospital.
Enhancing Recovery and Rehabilitation Outcomes
One of the primary benefits of transitional care in nursing is its role in enhancing recovery through structured rehabilitation services and individualized care plans. Patients often require targeted interventions to regain functional independence and maintain their quality of life after an acute illness or surgical procedure.
Key mechanisms through which transitional care enhances recovery include:
- Personalized Rehabilitation Services
- Patients discharged from acute care may need ongoing occupational and physical therapy either at a rehabilitation facility or during home health visits.
- Example: An older adult recovering from hip surgery may participate in a structured physical therapy program at a transitional care unit, followed by daily exercises guided by a family caregiver at home.
- Support for Complex Care Needs
- Patients with multiple chronic conditions benefit from a coordinated approach that addresses both medical and functional needs.
- Example: A patient with heart failure and diabetes may require careful medication management, nutritional guidance, and monitoring for signs of hospital readmission, all coordinated by the care team.
- Psychosocial and Educational Support
- Transitional care provides education to patients and family caregivers about managing symptoms, therapy adherence, and safety precautions.
- This support encourages active participation in recovery and strengthens the patient’s confidence, reducing anxiety and improving engagement in rehabilitation.
- Continuity Across Care Settings
- Through care coordination, patients receive consistent guidance from the hospital to home health care or skilled nursing facilities, minimizing disruptions in rehabilitation and maintaining momentum toward recovery.
By integrating rehabilitation services, structured follow-up, and caregiver support, transitional care maximizes functional outcomes and fosters independence, particularly for older adults who may face cognitive or mobility challenges.
Reducing Hospital Readmissions and Emergency Department Visits
Another significant benefit of transitional care in nursing is its proven role in reducing hospital readmissions and unnecessary emergency department care. Post-discharge periods are high-risk for complications, especially for older adults or patients with complex care needs. Transitional care addresses these risks through:
- Comprehensive Discharge Planning
- The transitional care team ensures patients are fully prepared for hospital to home transitions, providing clear instructions on medications, diet, wound care, and follow-up appointments.
- Example: A patient discharged after pneumonia receives home visits from a home health nurse to monitor breathing, oxygen therapy, and adherence to antibiotics, preventing hospital readmission.
- Early Identification and Intervention
- Ongoing monitoring during the first 30 days after discharge allows care providers to identify complications early, reducing the likelihood of returning to the emergency department.
- Example: A patient with chronic obstructive pulmonary disease (COPD) receives daily phone check-ins and symptom tracking, enabling timely interventions for breathing difficulties.
- Engagement of Family Caregivers
- Family caregivers play a pivotal role in ensuring compliance with care plans, monitoring for signs of deterioration, and communicating with primary care providers.
- Example: A caregiver notices fluid retention in a heart failure patient and contacts the transitional care team, preventing a full-blown relapse and avoiding hospitalization.
- Coordination Across Care Settings
- Patients experience seamless integration between hospital discharge, rehabilitation facilities, home health care, and primary care, reducing miscommunication and errors that often lead to readmissions.
Studies have shown that structured transitional care programs reduce hospital readmissions by up to 30% for older adults with multiple chronic conditions, emphasizing the critical role of care coordination and post-discharge support in achieving positive outcomes.
Example Scenario:
Mr. L, a 78-year-old with congestive heart failure and diabetes, is discharged from an acute care hospital to home health care. The transitional care team develops a comprehensive plan:
- Rehabilitation Services: Physical therapy to maintain mobility.
- Medication Management: Ensuring adherence and avoiding interactions.
- Caregiver Education: Teaching his daughter to monitor weight and recognize warning signs of fluid overload.
- Follow-Up Coordination: Scheduling visits with the primary care provider and a cardiologist.
With this coordinated approach, Mr. L experiences improved functional recovery, avoids complications, and does not require readmission to the hospital within the critical first 30 days.
Transitional Care Units and Rehabilitation Programs
Transitional care in nursing extends beyond discharge instructions—it often involves structured care settings designed to support recovery, rehabilitation, and continuity of care. Two essential components in this continuum are transitional care units (TCUs) and skilled nursing facilities (SNFs), both of which provide targeted interventions to meet the needs of patients transitioning from acute care to home or long-term care.
What Is a Transitional Care Unit versus a Skilled Nursing Facility
While both transitional care units and skilled nursing facilities provide post-hospitalization support, there are important distinctions in their purpose, intensity of care, and duration of stay:
- Transitional Care Unit (TCU):
- A TCU is a short-term, hospital-affiliated unit that focuses on intensive rehabilitation services and medical monitoring for patients immediately following hospitalization.
- TCUs are designed to stabilize patients with complex care needs before they return home or transition to another care facility.
- Patients typically stay in a TCU for a defined period, often days after discharge from acute care, depending on recovery progress.
- Example: A patient recovering from cardiac surgery may be admitted to a TCU for monitoring of vital signs, medication management, and initiation of a supervised physical therapy program before discharge home.
- Skilled Nursing Facility (SNF):
- SNFs provide longer-term support, combining medical care with rehabilitation services for patients who require ongoing assistance with daily activities or chronic disease management.
- Unlike TCUs, SNFs are often not hospital-affiliated and may cater to older adults who need extended recovery or long-term care.
- Example: A patient with multiple chronic conditions who has difficulty performing activities of daily living may remain in a SNF for weeks to months, receiving occupational and physical therapy as part of a structured care plan.
Both settings are integral to transitional care in nursing, as they bridge the gap between acute hospitalization and safe home health care, ensuring patients receive the right level of care services at the right time.
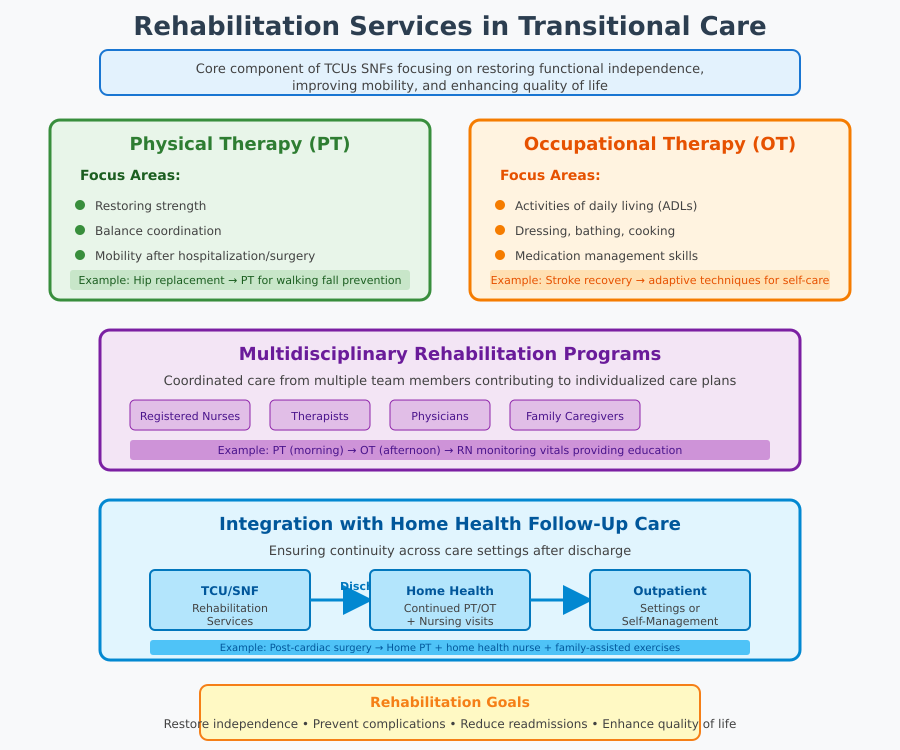
Rehabilitation Services and Occupational/Physical Therapy
Rehabilitation services are a core component of transitional care units and skilled nursing facilities. These services focus on restoring functional independence, improving mobility, and enhancing quality of life for patients recovering from acute illness, surgery, or injury.
Key aspects of rehabilitation in transitional care include:
- Physical Therapy (PT):
- Focuses on restoring strength, balance, coordination, and mobility after hospitalization or surgery.
- Example: A patient recovering from hip replacement may participate in PT sessions to regain walking ability and prevent falls.
- Occupational Therapy (OT):
- Helps patients regain skills necessary for daily living, such as dressing, bathing, cooking, and managing medication management.
- Example: An older adult recovering from stroke may work with an OT to learn adaptive techniques for self-care and home safety.
- Multidisciplinary Rehabilitation Programs:
- Patients often receive coordinated care from RNs, therapists, physicians, and family caregivers, all contributing to a care plan tailored to the patient’s specific needs.
- Example: A transitional care team may schedule PT sessions in the morning, followed by OT in the afternoon, with nurses monitoring vitals and providing education to patients and family caregivers.
- Integration with Home Health and Follow-Up Care:
- Rehabilitation services in TCUs or SNFs are often continued after discharge to home health or outpatient settings, ensuring continuity of care.
- Example: A patient discharged from a TCU after cardiac surgery may continue PT at home with visits from a home health nurse, while family caregivers assist with daily exercises and monitor for complications.
Example Scenario:
Mrs. K, a 79-year-old recovering from a fall resulting in a hip fracture, is admitted to a transitional care unit. Her care plan includes:
- Physical Therapy: Regaining walking ability and balance.
- Occupational Therapy: Practicing safe transfers and self-care at bedside.
- Medication Management: Ensuring proper analgesic use and preventing adverse effects.
- Family Caregiver Education: Training her daughter to assist with exercises at home.
After a 10-day stay in the TCU, Mrs. K transitions to home health care with continued rehabilitation services, maintaining continuity of care and reducing the risk of hospital readmission.
Hospital Discharge and Care Transitions
Effective transitional care in nursing begins at the point of hospital discharge and extends into the first days and weeks after a patient leaves the hospital. Discharge is more than a procedural step—it is a critical period in which careful planning, coordination, and patient education ensure continuity of care, reduce the risk of hospital readmission, and support safe, successful recovery.
Coordinating Discharge Planning and Hospital Discharge
Discharge planning is a multidisciplinary process that ensures patients leave the acute care setting with a clear, actionable plan for continued recovery. Proper coordination involves:
- Comprehensive Patient Assessment
- Evaluating the patient’s medical stability, functional abilities, and psychosocial needs.
- Example: An older adult with heart failure may require a review of fluid status, mobility, cognitive function, and family caregiver readiness to provide support.
- Multidisciplinary Care Team Collaboration
- Physicians, nurses, social workers, therapists, and case managers collaborate to develop an individualized care plan that addresses all aspects of post-discharge needs.
- Example: Nurses coordinate with a physical therapist to schedule rehabilitation services, while social workers ensure access to Medicare or Medicaid services for home support.
- Patient and Family Education
- Educating patients and family caregivers about medications, diet, activity restrictions, warning signs, and follow-up appointments is essential for safe care transitions.
- Example: Providing instruction on medication management and oxygen therapy for a patient discharged after a COPD exacerbation.
- Discharge Documentation and Communication
- Timely, accurate sharing of discharge summaries, lab results, and care instructions with primary care providers, home health agencies, and other care facilities ensures that critical information is not lost.
Practical Example:
Mr. T, a 76-year-old hospitalized for pneumonia, is ready for discharge. His transitional care team ensures:
- His care plan includes oxygen monitoring and daily vital checks.
- Family caregivers are trained on recognizing signs of deterioration.
- Follow-up appointments with his primary care provider and home health nurse are scheduled.
- Lab results and discharge instructions are sent electronically to his home health care provider.
This coordinated process reduces complications, supports continuity of care, and decreases the risk of hospital readmission.
Home Health, Follow-Up Primary Care, and Continuity
Once discharged, patients benefit from structured follow-up and integration into home health services and primary care to ensure ongoing care and high-quality transitional care. Key elements include:
- Home Health Care
- Home visits by nurses or therapists allow monitoring of patient recovery, adherence to care plans, and identification of early warning signs of deterioration.
- Example: A patient recently discharged from a transitional care unit after hip surgery may receive physical therapy at home to continue improving mobility and prevent falls.
- Follow-Up Primary Care
- Regular check-ins with the primary care provider reinforce medication adherence, monitor chronic conditions, and evaluate recovery progress.
- Example: A diabetic patient receives follow-up within 7 days to review blood glucose levels and adjust insulin doses if necessary.
- Coordination Across Care Settings
- Seamless communication between the hospital, home health care, rehabilitation facilities, and the primary care provider ensures that all team members are aligned.
- Example: Updates from home health nurses regarding wound healing or symptom changes are shared with the transitional care team, who may adjust rehabilitation services or care plans accordingly.
- Engagement of Family Caregivers
- Family caregivers reinforce daily routines, supervise medication management, and provide psychosocial support, bridging the gap between professional care and the patient’s home environment.
- Example: A caregiver ensures the patient adheres to a prescribed exercise program and reports any new symptoms promptly to healthcare professionals.
By combining home health, follow-up primary care, and active caregiver engagement, transitional care ensures continuity of care, promotes independence, and reduces the likelihood of emergency department visits or hospital readmission.
Example Scenario:
Mrs. S, an 80-year-old recovering from a stroke, is discharged to home health care after a 10-day transitional care unit stay. Her transitional care team coordinates:
- Physical therapy sessions at home.
- Daily nursing visits to monitor vital signs and medication management.
- Weekly communication with her primary care provider.
- Family caregiver education to assist with exercises and monitor for signs of deterioration.
This coordinated approach maintains continuity of care, supports recovery, and enhances high-quality transitional care outcomes.
Family Caregivers and Support During Care Transitions
Family caregivers play a pivotal role in transitional care in nursing, serving as the link between hospitalization, rehabilitation, and home health care. Their active involvement ensures continuity of care, reduces the risk of hospital readmission, and supports recovery for patients with complex care needs. Preparing caregivers and providing access to support services are essential components of high-quality transitional care.
Preparing Caregivers for Transitional Care Responsibilities
Transitioning from hospital to home places significant responsibility on family caregivers, who must manage tasks often performed by healthcare professionals in the hospital or transitional care units. Effective preparation focuses on education, skill-building, and ongoing support.
Key strategies include:
- Education on Medical and Rehabilitation Needs
- Caregivers are trained to assist with medication management, wound care, and monitoring for signs of deterioration.
- Example: A caregiver supporting a patient discharged after hip surgery learns proper techniques for safe transfers, mobility assistance, and monitoring for post-surgical complications.
- Understanding the Care Plan and Care Transitions
- Clear instruction on the care plan, including therapy schedules, dietary recommendations, and follow-up appointments with primary care providers, helps caregivers manage daily routines effectively.
- Example: A stroke patient’s family caregiver is instructed on exercises recommended by occupational and physical therapists, as well as when to contact the transitional care team for changes in function or health status.
- Skills for Psychosocial Support
- Caregivers provide emotional support, motivate patients to adhere to rehabilitation services, and help manage anxiety or confusion during recovery.
- Example: Assisting an older adult recovering from heart failure to maintain adherence to fluid restrictions while encouraging independence.
- Safety and Home Environment Preparation
- Caregivers learn to assess the home for hazards, implement assistive devices, and arrange for appropriate care services.
- Example: Installing grab bars, using mobility aids, or arranging a safe space for exercises prescribed during home health visits.
- Coordination with Healthcare Providers
- Family caregivers serve as communication links between patients and the transitional care team, relaying observations and ensuring follow-up appointments are kept.
- Example: Reporting changes in weight or blood pressure for a patient with heart failure to prevent hospital readmission.
Caregiver Support Services and Resources
Supporting family caregivers is critical to preventing burnout, enhancing confidence, and sustaining effective care transitions. Access to structured support services ensures caregivers can meet patient needs without compromising their own well-being.
Key support mechanisms include:
- Training and Education Programs
- Hospitals, home health agencies, and community organizations provide workshops or online modules for caregivers on medication management, rehabilitation exercises, and chronic disease monitoring.
- Example: A caregiver attends a hospital-led session on diabetes management before the patient is discharged to home health care.
- Respite Care Services
- Short-term relief services allow caregivers to rest while maintaining continuity of care for the patient.
- Example: Utilizing a skilled nursing facility for a few days while the caregiver attends to personal obligations.
- Counseling and Peer Support Groups
- Emotional support reduces stress and improves caregiver confidence in handling complex care needs.
- Example: Caregivers of cognitively impaired older adults attend group sessions to share strategies for managing agitation, medication adherence, and therapy routines.
- Resource Coordination
- Social workers and care coordinators connect caregivers with Medicare or Medicaid services, home modification programs, and community-based rehabilitation services.
- Example: Arranging for home health visits, therapy sessions, and durable medical equipment to support safe recovery after hospital discharge.
Practical Scenario:
Mr. P, a 78-year-old recovering from stroke, is being discharged from a transitional care unit to home health care. His daughter, acting as family caregiver, is prepared through:
- Training on safe transfers and medication management.
- A schedule for physical therapy and occupational therapy exercises at home.
- Guidance on monitoring signs of deterioration and coordinating with the primary care provider.
- Access to respite care and caregiver support groups to prevent burnout.
Through structured preparation and ongoing support, caregivers ensure high-quality transitional care, improve patient rehabilitation outcomes, and help prevent hospital readmission.
Medicare, Reimbursement, and Quality of Transitional Care
Delivering high-quality transitional care in nursing requires not only effective coordination and patient-centered interventions but also a clear understanding of reimbursement mechanisms and quality assessment. Proper funding and monitoring ensure that transitional care management (TCM) services are sustainable, accessible, and effective in reducing hospital readmissions, enhancing continuity of care, and supporting both patients and family caregivers across care settings.
Reimbursement for Transitional Care Management
Transitional care management services are recognized and reimbursed under Medicare, which provides financial support for structured post-discharge care. Understanding reimbursement processes allows healthcare providers and care teams to implement sustainable care models while ensuring patients receive high-quality transitional care.
Key aspects include:
- Medicare Transitional Care Management (TCM) Codes
- Medicare reimburses TCM services using specific billing codes (e.g., CPT codes 99495 and 99496) that account for the complexity of care and level of care coordination.
- Example: A patient discharged after an acute illness with multiple chronic conditions may qualify for a higher reimbursement code due to complex care needs, reflecting additional time spent on care planning, home health coordination, and patient education.
- Eligibility Criteria for TCM Services
- The patient must have been discharged from a hospital, skilled nursing facility, or rehabilitation facility.
- The care team must provide structured follow-up within specified timelines: usually 7 days for moderate complexity and 14 days for high complexity patients.
- Example: A patient recovering from heart surgery receives a home health visit within 7 days of hospital discharge, with documentation of assessment, medication management, and care coordination.
- Components of Reimbursable TCM Services
- Comprehensive review of medications, referrals, and follow-up care.
- Contact with the patient or family caregiver within the first 48 hours to reinforce care instructions.
- Collaboration among healthcare providers to ensure continuity across care settings.
By aligning reimbursement with structured care activities, Medicare patients benefit from consistent post-discharge monitoring, while healthcare providers can sustainably deliver transitional care services.
Measuring Quality and Best Practices for Care Models
Assessing the quality of transitional care is essential for ensuring patient safety, optimizing recovery, and improving health outcomes. High-quality transitional care programs rely on metrics, evidence-based practices, and continuous quality improvement.
Key strategies include:
- Outcome Measurement
- Metrics such as hospital readmission rates, emergency department visits, patient functional recovery, and satisfaction are used to evaluate program effectiveness.
- Example: A hospital implementing a transitional care program tracks 30-day readmission rates for older adults with heart failure and compares outcomes for patients who received structured rehabilitation services versus those who did not.
- Standardized Assessment Tools
- Use of validated tools and checklists ensures that all aspects of transitional care services, including medication management, therapy adherence, and home health coordination, are consistently monitored.
- Example: A transitional care team may use a standardized discharge checklist to document whether family caregivers received education, whether follow-up appointments are scheduled, and whether care plans are communicated to all providers.
- Evidence-Based Care Models
- Programs like the Coleman Care Transitions Intervention or Naylor Transitional Care Model emphasize structured follow-up, patient and caregiver education, and care coordination across settings.
- Example: Implementing a nurse-led transitional care program where RNs provide in-home visits and telephone follow-up has been shown to reduce hospital readmissions by up to 30% in older adults with multiple chronic conditions.
- Integration Across Care Settings
- High-quality transitional care requires seamless communication between transitional care units, home health, primary care providers, and rehabilitation facilities.
- Example: A care team ensures that discharge summaries, therapy plans, and medication lists are shared electronically with home health care providers and the patient’s primary care provider, maintaining continuity of care.
- Continuous Quality Improvement (CQI)
- Care programs review outcomes regularly and implement process improvements.
- Example: Identifying common reasons for hospital readmission (e.g., nonadherence to medication management or missed follow-up appointments) allows the transitional care team to revise education protocols or increase follow-up frequency.
Practical Scenario:
Mrs. D, a 75-year-old patient discharged after a hip fracture, participates in a transitional care program reimbursed under Medicare TCM. Her transitional care team coordinates:
- A home health visit within 48 hours to check wound healing and rehabilitation progress.
- Comprehensive medication management review, ensuring adherence to pain and anticoagulant therapy.
- Scheduled follow-up with her primary care provider within 7 days.
- Documentation and use of a standardized checklist to track outcomes and continuity of care.
The program reduces her risk of hospital readmission, improves functional recovery, and ensures that family caregivers are fully engaged in the care process.
Implementing a Successful One-Care Model Across Care Settings
A One-Care Model is a patient-centered framework that emphasizes seamless integration of transitional care services, care coordination, and rehabilitation across all care settings. By unifying hospital, home health, primary care, skilled nursing facilities, and transitional care units, this model addresses complex care needs, enhances continuity of care, and improves health outcomes for patients, particularly older adults and those with multiple chronic conditions.
Implementing a successful one-care approach requires structured processes, collaborative transitional care teams, and active engagement of patients and family caregivers.
Strategies for Effective Care Coordination
Effective care coordination is the backbone of the One-Care Model. Strategies include:
- Multidisciplinary Team Collaboration
- Integration of RNs, physicians, therapists, social workers, and case managers ensures that care plans are comprehensive and individualized.
- Example: A patient discharged after a stroke benefits from collaboration between occupational and physical therapists, home health nurses, and the primary care provider, ensuring therapy, medication management, and monitoring of functional recovery are aligned.
- Standardized Communication and Documentation
- Electronic health records (EHRs) facilitate sharing of discharge summaries, rehabilitation services plans, and follow-up instructions across care settings.
- Example: Updates from a transitional care unit are transmitted to the home health care nurse and primary care provider, ensuring everyone has access to the same care plan.
- Patient and Family Caregiver Engagement
- Active involvement of family caregivers and patients in care transitions improves adherence to therapy, medication management, and monitoring of recovery.
- Example: Training a caregiver to track wound healing, manage medications, and report changes promptly reduces the risk of hospital readmission.
- Care Transition Checkpoints
- Implement structured checkpoints during hospital discharge, rehabilitation, and home health care phases to identify gaps and prevent errors.
- Example: A nurse-led home visit 48 hours after discharge ensures that therapy exercises are performed correctly and complications are detected early.
- Integrated Care Across Acute and Long-Term Settings
- Ensuring seamless handoffs between acute care, transitional care units, and skilled nursing facilities maintains continuity of care.
- Example: A patient recovering from hip surgery transitions from acute care to a TCU for short-term rehabilitation services, then continues therapy at a skilled nursing facility or home health care setting.
Lessons Learned and Future Directions in Transitional Care
Implementing a One-Care Model has provided several key lessons for optimizing transitional care in nursing:
- Early Planning Improves Outcomes
- Initiating discharge planning and care coordination early during hospitalization reduces complications and shortens recovery times.
- Example: Patients whose care team begins planning on admission demonstrate better functional recovery and lower hospital readmission rates.
- Family Caregivers Are Essential Partners
- Engaging family caregivers in transitional care services ensures adherence to care plans, early recognition of complications, and improved rehabilitation outcomes.
- Technology Enhances Continuity
- Use of telehealth, remote monitoring, and electronic documentation strengthens care coordination, supports home health care, and facilitates communication across care settings.
- Example: Telemonitoring a patient with congestive heart failure allows the transitional care team to adjust medications proactively, preventing emergency visits.
- Focus on High-Risk Populations
- Patients with multiple chronic conditions, cognitive impairment, or limited social support benefit most from a structured one-care approach.
- Example: Older adults discharged from skilled nursing facilities may require intensive rehabilitation services, frequent home visits, and continuous caregiver support to prevent hospital readmission.
- Data-Driven Continuous Improvement
- Monitoring quality of transitional care through metrics such as readmission rates, therapy adherence, and patient satisfaction informs refinements to care programs.
- Example: Hospitals implementing feedback loops in a transitional care program adjust therapy intensity and caregiver training based on outcome data to improve effectiveness.
Future Directions:
- Expansion of Telehealth and Home-Based Care to reach patients in rural or underserved areas.
- Integration of Predictive Analytics to identify patients at high risk for readmission or poor recovery.
- Personalized Care Models that tailor rehabilitation and complex care services to patient-specific needs.
- Policy and Reimbursement Alignment with Medicare and Medicaid services to incentivize high-quality, coordinated transitional care programs.
Practical Scenario:
Mr. H, a 72-year-old with heart failure and diabetes, is discharged from an acute care hospital to a transitional care unit and then home. A One-Care Model approach ensures:
- The transitional care team develops a comprehensive care plan including rehabilitation services and medication management.
- Family caregivers are trained to monitor vital signs and symptoms.
- Home health visits and follow-up primary care appointments are scheduled.
- Telehealth monitoring tracks daily weight and blood pressure to prevent hospital readmission.
As a result, Mr. H experiences improved recovery, fewer complications, and a smooth transition across multiple care settings.
Conclusion
Transitional care in nursing is a critical component of modern healthcare, bridging the gap between hospitalization, rehabilitation, and home health to ensure patients experience safe, coordinated, and effective recovery. Throughout the continuum of care, structured interventions—ranging from transitional care units and skilled nursing facilities to home health services and follow-up primary care—support patients with complex care needs, including older adults and those with multiple chronic conditions.
The success of transitional care programs relies on a multidisciplinary care team working collaboratively to develop individualized care plans, deliver comprehensive rehabilitation services, and actively engage family caregivers. Caregiver preparation and support are essential, as they reinforce therapy adherence, monitor for complications, and maintain continuity of care after discharge. By integrating transitional care management principles, healthcare providers can reduce hospital readmissions, improve rehabilitation outcomes, and enhance quality of transitional care across care settings.
Moreover, the alignment of Medicare reimbursement with structured transitional care services and the use of data-driven quality metrics ensure that these programs are sustainable, measurable, and patient-centered. Implementing a One-Care Model exemplifies how coordinated, seamless transitions can optimize patient outcomes, enhance caregiver engagement, and improve overall health outcomes for vulnerable populations.
For nursing students, understanding transitional care in nursing is not only an academic exercise but a practical imperative. It underscores the importance of comprehensive discharge planning, interprofessional collaboration, and evidence-based strategies that extend care beyond the hospital walls. By mastering the principles of transitional care, future nurses can contribute to safer care transitions, support patients and family caregivers, and promote a culture of high-quality, coordinated care throughout the healthcare system.
In essence, transitional care in nursing is about more than bridging settings—it is about creating a continuum where patients receive consistent, personalized, and effective care, enabling recovery, independence, and improved quality of life.
Frequently Asked Questions
What is the meaning of transitional care?
Transitional care refers to a set of coordinated healthcare services that support patients as they move between different care settings, such as from a hospital or acute care unit to home health, a skilled nursing facility, or a rehabilitation facility. Its goal is to ensure continuity of care, prevent complications, and reduce hospital readmission by addressing medical, functional, and psychosocial needs during these critical transitions.
What are examples of transitions of care?
Transitions of care occur whenever a patient moves between care settings or care levels. Examples include:
- Hospital to home: A patient discharged after surgery receives home health care and follow-up with their primary care provider.
- Acute care to a transitional care unit (TCU): A patient recovering from cardiac surgery is monitored in a TCU before returning home.
- Hospital to skilled nursing facility (SNF): An older adult with a hip fracture moves to a SNF for rehabilitation services and occupational/physical therapy.
- ICU to general ward: A critically ill patient transitions to a medical-surgical unit for continued recovery and care coordination.
Is transitional care the same as hospice?
No, transitional care and hospice care are not the same. Transitional care focuses on supporting recovery, rehabilitation, and safe care transitions after hospitalization or acute illness. It aims to restore independence and prevent readmissions. Hospice care, on the other hand, is for patients with terminal illness and prioritizes comfort and quality of life rather than rehabilitation or recovery.
What is transitional care in the ICU?
In the ICU, transitional care refers to the structured support provided as patients move from critical care to a lower-acuity unit, such as a step-down or general medical-surgical ward. This involves:
- Stabilizing acute illness symptoms and monitoring for complications.
- Ensuring continuity of care by communicating care plans, medications, and rehabilitation services to the receiving team.
- Engaging family caregivers to prepare them for ongoing care needs after ICU discharge.
Example: A patient recovering from severe sepsis is transferred from the ICU to a step-down unit with a detailed plan for medication management, nutrition, and physical therapy, maintaining a seamless care transition.
