Nonselective Beta Blockers: A Nursing Student’s Guide to β-Adrenergic Receptor Blockade
Nonselective beta blockers are a foundational class of cardiovascular medications, widely used in the management of heart failure, hypertension, angina, and other cardiac conditions. At their core, these blocking agents work by inhibiting both β1 and β2 adrenergic receptors, reducing heart rate, cardiac contractility, and the workload on the heart. Unlike cardioselective beta blockers, which primarily target β1 receptors in the heart, nonselective β-blockers exert broader effects on the cardiovascular system, including influences on blood vessels and pulmonary function. Understanding their pharmacology, mechanism of action, and clinical applications is essential for nursing students who are learning to manage patients with complex cardiovascular disease.
The use of nonselective beta-blockers extends beyond simple heart rate control. These medications play a pivotal role in improving outcomes in patients with chronic heart failure, managing high blood pressure in adults, and preventing complications in angina or ischemic heart disease. Their administration requires careful consideration of contraindications, particularly in patients with asthma or chronic obstructive pulmonary disease, where β2 receptor blockade can precipitate bronchospasm. Nurses must also monitor for adverse effects such as hypotension, fatigue, and potential interactions with other agents, including calcium channel blockers and epinephrine, which can alter cardiovascular responses.
This guide provides a detailed exploration of nonselective beta-blocker therapy, emphasizing the integration of pharmacology, receptor blockade mechanisms, and practical nursing considerations. It examines the distinctions between selective versus nonselective beta blockers, highlights common examples such as propranolol, carvedilol, and metoprolol, and outlines clinical scenarios where their use is indicated. By understanding the effects of beta blockers on the heart, blood vessels, and adrenergic receptors, nursing students can develop the knowledge and critical thinking necessary to ensure safe and effective patient care in diverse cardiovascular settings.
Understanding Nonselective Beta Blockers and β-Adrenergic Receptor Blockade
Definition and Mechanism of Nonselective Beta-Blockers
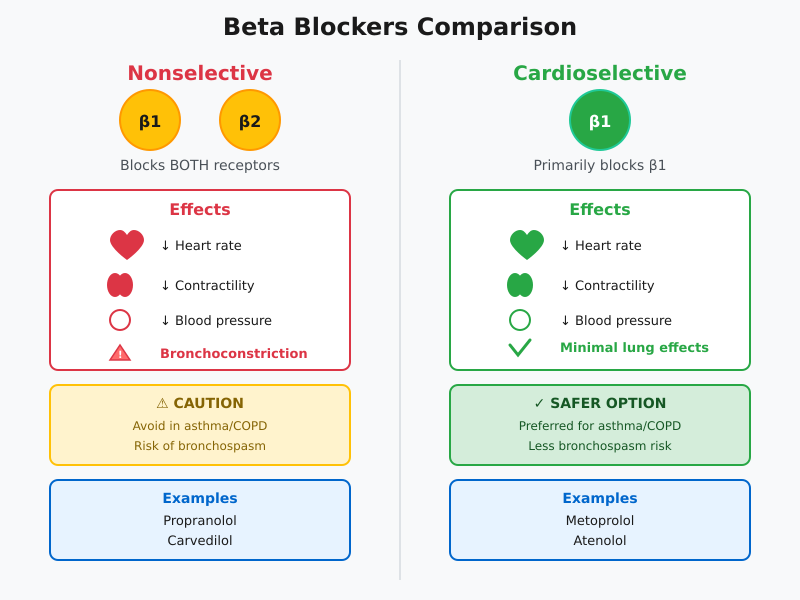
Nonselective beta blockers are a class of blocking agents that inhibit both β1 and β2 adrenergic receptors, producing systemic effects across the cardiovascular system. Unlike cardioselective beta blockers, which primarily target β1 receptors in the heart, nonselective β-blockers affect beta receptors located in both cardiac and extra-cardiac tissues, including the lungs and blood vessels. By blocking these receptors, nonselective beta blockers reduce the effects of adrenergic stimulation, such as increased heart rate, myocardial contractility, and vasodilation mediated by β2 receptors.
For example, propranolol, one of the first nonselective beta-blockers introduced into clinical practice, exerts its blocking effects on both β1 and β2 receptors, making it effective for conditions such as angina, hypertension, and certain forms of arrhythmia. Similarly, carvedilol combines nonselective beta blockade with α1 receptor blockade, which allows for additional vasodilation and improved outcomes in heart failure with reduced ejection fraction. The mechanism of action involves competitive inhibition at the receptor site, preventing endogenous catecholamines—primarily epinephrine and norepinephrine—from activating the receptor.
β-Adrenergic Receptors in Cardiac and Vascular Physiology
Understanding β-adrenergic receptors is essential for grasping how nonselective beta blockers exert therapeutic effects. β1 receptors, predominantly located in the heart, mediate increases in heart rate, contractility, and cardiac output in response to sympathetic stimulation. In contrast, β2 receptors are found in the smooth muscle of blood vessels and the lungs, mediating vasodilation and bronchodilation. When nonselective beta-blockers inhibit β2 receptors, they reduce vascular relaxation and can potentially precipitate bronchoconstriction in patients with asthma or chronic obstructive pulmonary disease (COPD).
For instance, in a patient with hypertension and concurrent COPD, the use of a nonselective beta-blocker like propranolol requires careful monitoring due to the blocking effects on β2 receptors in the lungs. On the other hand, metoprolol, a cardioselective beta blocker, primarily targets β1 receptors, reducing heart rate and cardiac workload without significant pulmonary effects. These distinctions highlight the importance of understanding receptor physiology in clinical decision-making and patient safety.
Pharmacology of Nonselective Beta Blockers
The pharmacology of nonselective beta blockers centers on their ability to modulate β-adrenergic receptor activity, leading to measurable reductions in heart rate, cardiac output, and blood pressure. At the molecular level, these agents inhibit the adenylate cyclase pathway activated by β receptors, reducing intracellular cyclic AMP levels and downstream calcium influx into myocardial cells. This biochemical effect translates clinically into slower heart rhythm, decreased myocardial oxygen demand, and improved cardiac efficiency.
Systemically, nonselective beta-blockers reduce blood pressure by lowering cardiac output and, in some cases, by modulating renin release from the kidneys via β1 receptor blockade. This is particularly relevant in heart failure management, where drugs such as carvedilol have been shown to improve ventricular function while providing protective cardiovascular effects. Additionally, intrinsic sympathomimetic activity (ISA), present in some beta-blockers, can partially activate receptors while still providing blockade, which may reduce bradycardia risk in certain patient populations.
In clinical practice, these pharmacologic properties make nonselective beta blockers valuable for a wide spectrum of cardiovascular conditions, including angina, chronic heart failure, and high blood pressure management. Nurses play a crucial role in monitoring adverse effects, evaluating heart rate and blood pressure, and educating patients about taking a beta blocker safely, particularly regarding drug interactions with epinephrine or calcium channel blockers.
Types of Beta Blockers in Clinical Practice
Nonselective vs. Cardioselective Beta Blockers
Beta blockers are a diverse class of medications, broadly divided into nonselective beta blockers and cardioselective beta blockers. Understanding these distinctions is essential for nursing students, as it guides safe administration, monitoring, and patient education.
Nonselective beta blockers block both β1 and β2 adrenergic receptors, producing effects on the heart, lungs, and blood vessels. In contrast, cardioselective beta blockers primarily target β1 receptors, focusing on the heart and minimizing pulmonary effects. This difference has significant clinical implications:
- Cardiovascular Effects: Both nonselective and cardioselective beta blockers reduce heart rate, myocardial contractility, and blood pressure, but nonselective agents also affect β2 receptors, potentially causing bronchoconstriction.
- Pulmonary Considerations: Patients with asthma or chronic obstructive pulmonary disease (COPD) are at higher risk with nonselective β-blockers due to β2 receptor blockade, which can trigger bronchospasm. Cardioselective beta blockers such as metoprolol are preferred in these populations.
- Nursing Implications: Nurses must assess heart rate, blood pressure, and respiratory status before and during therapy. Education should emphasize reporting shortness of breath, wheezing, or unusual fatigue.
Intrinsic Sympathomimetic Activity and Clinical Relevance
Some beta blockers possess intrinsic sympathomimetic activity (ISA), meaning they partially stimulate β receptors while still providing blockade. This dual action can influence drug selection, particularly in patients prone to bradycardia or low cardiac output.
- Clinical Advantages of ISA:
- May reduce the risk of excessive bradycardia compared to standard nonselective beta blockers.
- Can help maintain heart rhythm in patients who are sensitive to full receptor blockade.
- Examples: Pindolol and acebutolol are known for ISA, though they are less commonly used than propranolol or carvedilol.
- Nursing Considerations: Nurses should understand that beta-blockers with ISA may have a milder effect on heart rate and blood pressure, requiring careful titration and monitoring, particularly in heart failure or high blood pressure management.
Common Examples and Indications
Beta blockers are selected based on receptor specificity, ISA, and the targeted cardiovascular condition. Some widely used examples include:
- Propranolol: A classic nonselective beta-blocker used in angina, hypertension, arrhythmias, migraine prophylaxis, and certain forms of anxiety. Its blocking effects on β1 and β2 receptors make it effective for multiple cardiovascular and systemic applications, but caution is needed in patients with asthma or COPD.
- Carvedilol: Combines nonselective beta blockade with α1-blocking properties, providing vasodilation alongside heart rate reduction. Commonly used in heart failure, particularly heart failure with reduced ejection fraction, and high blood pressure management.
- Metoprolol: A cardioselective beta-blocker that preferentially targets β1 receptors, making it safer for patients with pulmonary comorbidities. Used in hypertension, angina, post-myocardial infarction management, and chronic heart failure.
- Nadolol: A nonselective beta-blocker with a long half-life, often used for angina and hypertension. Nursing monitoring focuses on blood pressure, heart rate, and potential adverse effects such as fatigue or bradycardia.
Key Nursing Implications Across Types:
- Evaluate baseline heart rate, blood pressure, and respiratory status prior to administration.
- Monitor for adverse effects, including fatigue, bradycardia, or worsening heart failure.
- Educate patients on adherence, taking a beta blocker safely, and recognizing early signs of complications.
- Adjust drug selection based on comorbidities, such as asthma, COPD, or chronic heart failure, and clinical goals like lowering blood pressure or preventing angina attacks.
Clinical Indications for Nonselective Beta Blockers in Cardiovascular Care
Heart Failure and Congestive Heart Failure Management
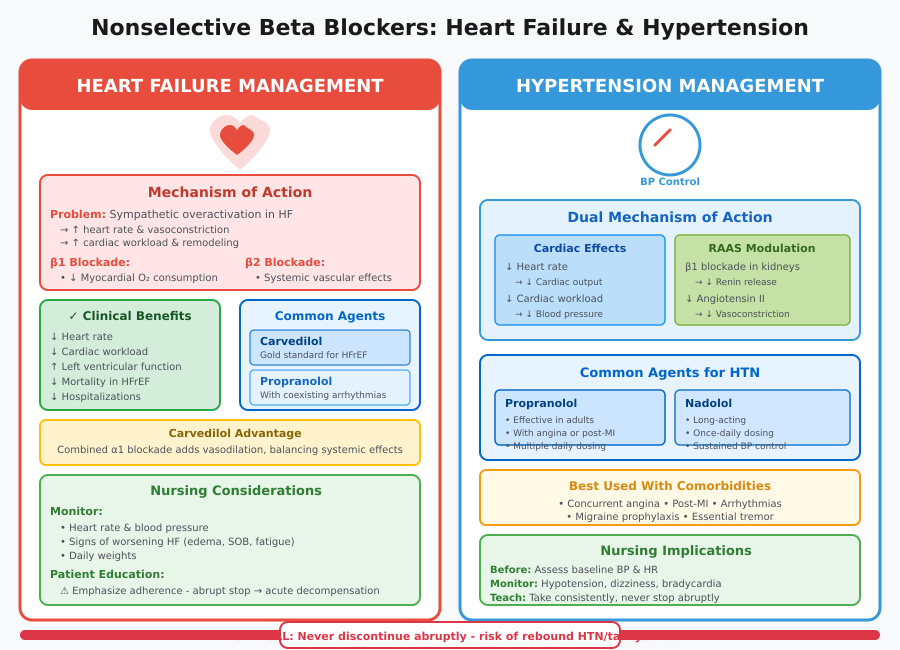
Nonselective beta blockers play a central role in the management of heart failure, particularly in patients with congestive heart failure or chronic heart failure. These blocking agents reduce sympathetic overactivation by inhibiting both β1 and β2 adrenergic receptors, which in turn decreases heart rate, myocardial contractility, and oxygen demand.
Mechanism and Rationale:
- In heart failure, elevated sympathetic activity increases heart rate and peripheral vasoconstriction, which raises cardiac workload and exacerbates cardiac remodeling.
- By blocking β1 receptors, nonselective beta blockers reduce myocardial oxygen consumption and improve left ventricular function over time.
- β2 receptor blockade can contribute to systemic vascular effects, including mild vasoconstriction, but in agents like carvedilol, combined α1 blockade adds vasodilation, balancing systemic effects.
Examples in Clinical Practice:
- Carvedilol: Reduces mortality in heart failure with reduced ejection fraction by improving cardiac output and reducing hospitalization.
- Propranolol: Occasionally used in chronic congestive heart failure patients with coexisting arrhythmias, though less common than carvedilol due to β2 blockade.
- Nursing Considerations: Monitor heart rate, blood pressure, and signs of worsening heart failure such as edema, shortness of breath, or fatigue. Patient education should emphasize adherence, as abrupt discontinuation can precipitate acute decompensation.
Hypertension and High Blood Pressure Control
Nonselective beta-blockers are also prescribed to treat high blood pressure, especially when patients have additional cardiovascular comorbidities. Their efficacy stems from a combination of cardiac effects and modulation of the renin-angiotensin-aldosterone system (RAAS) via β1 receptor blockade in the kidneys.
Mechanisms:
- Reduction of heart rate lowers cardiac output, directly decreasing blood pressure and heart workload.
- Suppression of renin release decreases angiotensin II-mediated vasoconstriction, contributing to lower blood pressure.
Examples:
- Propranolol: Effective in hypertension management in adults, particularly in patients with concurrent angina or post-myocardial infarction.
- Nadolol: Long-acting nonselective beta-blocker used in chronic hypertension with sustained effect.
Nursing Implications:
- Assess baseline blood pressure and heart rate before initiating therapy.
- Monitor for hypotension, dizziness, or bradycardia as adverse effects.
- Educate patients on taking a beta blocker consistently, avoiding abrupt cessation, and reporting unusual fatigue or lightheadedness.
Angina and Other Cardiovascular Conditions
Nonselective beta-blockers are widely used in the management of angina, ischemic heart disease, and certain arrhythmias, providing both prophylactic and symptomatic relief.
Mechanism:
- β1 blockade decreases heart rate and contractility, reducing myocardial oxygen consumption during exertion.
- β2 blockade can reduce blood vessel dilation, which may influence vascular resistance, though combined α1 blockade in agents like carvedilol counteracts excessive vasoconstriction.
Clinical Applications:
- Propranolol: Commonly prescribed for stable angina and to prevent exercise-induced ischemia.
- Carvedilol: Used in patients with angina coexisting with heart failure for dual benefit.
- Arrhythmias: Nonselective beta blockers help stabilize heart rhythm in atrial fibrillation or supraventricular tachycardia.
Nursing Considerations:
- Monitor heart rate, blood pressure, and ECG when initiating therapy for arrhythmias.
- Educate patients about recognizing angina symptoms, reporting changes in chest pain, and avoiding sudden cessation of medication, which can precipitate rebound tachycardia or ischemia.
Contraindications and Precautions in Nonselective Beta-Blocker Therapy
Pulmonary Considerations
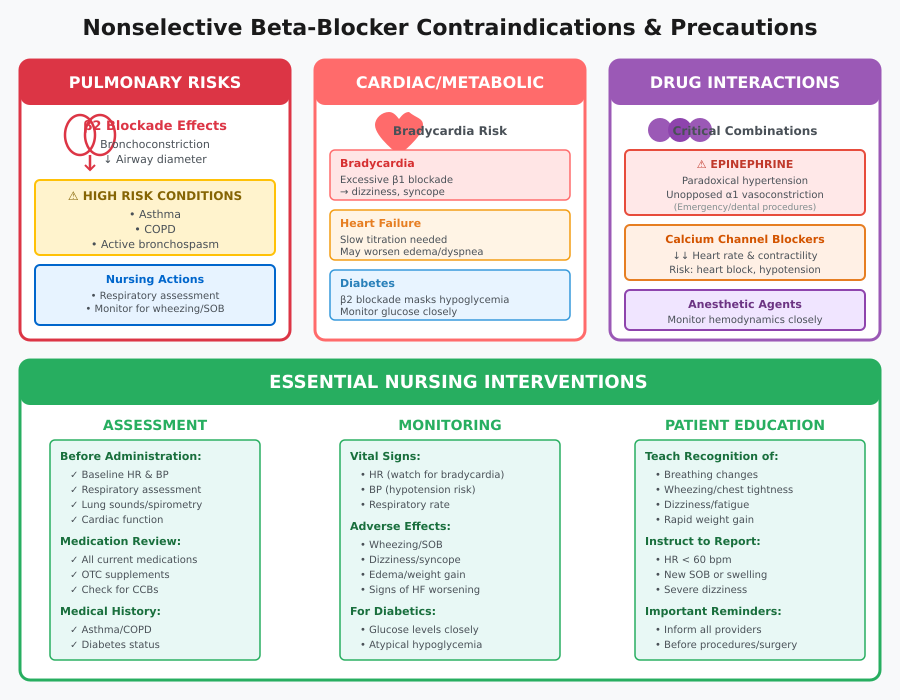
Nonselective beta blockers, by blocking both β1 and β2 adrenergic receptors, have significant implications for patients with asthma or chronic obstructive pulmonary disease (COPD). The β2 receptor blockade in bronchial smooth muscle can precipitate bronchospasm, reduce airway diameter, and worsen respiratory function.
Clinical Examples and Implications:
- Propranolol, a classic nonselective beta-blocker, can trigger severe bronchoconstriction in a patient with asthma if prescribed without caution.
- Carvedilol, while effective for heart failure and high blood pressure, also carries a β2 blockade risk, requiring careful titration or avoidance in patients with COPD.
Nursing Considerations:
- Conduct a thorough respiratory assessment prior to administration, including spirometry or symptom history.
- Educate patients to recognize early signs of wheezing, shortness of breath, or increased sputum production.
- Collaborate with prescribers to consider cardioselective beta blockers like metoprolol in patients with significant pulmonary disease.
Cardiac and Metabolic Precautions
While nonselective beta blockers are essential in managing cardiovascular disease, certain cardiac and metabolic conditions warrant caution.
Key Considerations:
- Bradycardia: Excessive β1 receptor blockade may slow heart rate, potentially leading to symptomatic bradycardia, dizziness, or syncope.
- Heart failure: In patients with decompensated congestive heart failure, initiating nonselective beta blockers too rapidly can worsen cardiac output and exacerbate symptoms such as edema and dyspnea.
- Diabetes: β2 receptor blockade may mask signs of hypoglycemia, such as tachycardia, making glucose monitoring essential.
Clinical Example:
- A patient with chronic heart failure started on carvedilol requires slow titration, careful monitoring of blood pressure, heart rate, and weight, with education on reporting early signs of worsening heart failure.
Nursing Implications:
- Obtain baseline heart rate and blood pressure before initiating therapy.
- Monitor for adverse effects, including hypotension, bradycardia, and signs of worsening heart failure.
- Educate patients with diabetes about self-monitoring of blood glucose and recognizing atypical hypoglycemia symptoms.
Drug Interactions and Perioperative Use
Nonselective beta blockers interact with several drugs and require special precautions during perioperative care.
Epinephrine and Anesthetic Considerations:
- Epinephrine, commonly used in emergencies or dental procedures, may cause paradoxical hypertension when administered to patients on nonselective beta blockers due to unopposed α1-mediated vasoconstriction.
- During surgery, anesthetic agents combined with beta blockade can potentiate bradycardia or hypotension, requiring close hemodynamic monitoring.
Calcium Channel Blocker Interactions:
- Concurrent use with calcium channel blockers (e.g., verapamil or diltiazem) may excessively depress heart rate and cardiac contractility, increasing the risk of heart block or symptomatic hypotension.
Nursing Recommendations:
- Verify all medications, including over-the-counter agents, prior to administering a nonselective beta-blocker.
- Collaborate with the anesthesia team for perioperative management, ensuring vital signs are closely monitored during induction and recovery.
- Educate patients to inform all healthcare providers about their beta-blocker therapy, especially before procedures or emergency care.
Adverse Effects and Nursing Monitoring
Cardiovascular Adverse Effects
Nonselective beta blockers, while essential for managing heart failure, high blood pressure, and other cardiovascular conditions, can produce significant cardiovascular adverse effects due to β1 receptor blockade in the heart.
Common Effects Include:
- Bradycardia: Excessive slowing of the heart rate can lead to dizziness, syncope, or fatigue.
- Hypotension: Reduced cardiac output and vasodilation may cause low blood pressure, lightheadedness, or fainting.
- Worsening Heart Failure: In patients with chronic heart failure, abrupt initiation or rapid titration of nonselective beta-blockers can transiently reduce cardiac output, exacerbating edema, shortness of breath, or exercise intolerance.
Assessment and Intervention:
- Baseline Measurements: Record heart rate, blood pressure, and weight before starting therapy.
- Ongoing Monitoring: Assess heart rhythm regularly and watch for signs of decompensation in patients with heart failure, including increasing shortness of breath, edema, or fatigue.
- Interventions: For bradycardia or hypotension, notify the prescriber; dose adjustments or temporary discontinuation may be required. Gradual titration is critical to minimize adverse effects.
Example:
A 65-year-old patient with heart failure with reduced ejection fraction started on carvedilol should be monitored daily for blood pressure, heart rate, and weight changes. Nurses should educate the patient to report sudden fatigue, dizziness, or worsening dyspnea.
Respiratory and Systemic Effects
Nonselective β-blockers also impact β2 receptors, leading to respiratory and systemic adverse effects:
Respiratory Effects:
- Bronchospasm: Particularly in patients with asthma or chronic obstructive pulmonary disease (COPD), β2 receptor blockade can precipitate wheezing, shortness of breath, and hypoxia.
Systemic Effects:
- Fatigue: Reduced cardiac output can lead to persistent tiredness, impacting daily activity.
- Sexual Dysfunction: Some patients experience erectile dysfunction or decreased libido due to systemic sympathetic blockade.
- Rebound Hypertension: Abrupt discontinuation may lead to sudden increases in blood pressure and heart rate, especially in patients with hypertension or angina.
Nursing Implications:
- Conduct baseline respiratory assessment and monitor for bronchospasm in at-risk patients.
- Educate patients on reporting unusual fatigue, sexual dysfunction, or chest discomfort.
- Emphasize gradual tapering when discontinuing therapy to prevent rebound effects.
Example:
A patient with high blood pressure and mild COPD prescribed propranolol must be closely monitored for wheezing, shortness of breath, and oxygen saturation, with patient teaching on early recognition of bronchospasm.
Patient Assessment and Early Warning Signs
Effective nursing monitoring ensures the safe use of nonselective beta-blockers and early detection of adverse effects.
Monitoring Strategies Include:
- Vital Signs: Regular assessment of heart rate, blood pressure, and respiratory rate.
- Fluid Status: Monitor for edema or sudden weight gain in patients with heart failure.
- Laboratory Values: In some cases, monitor blood glucose, especially in diabetic patients, since β2 blockade may mask hypoglycemia symptoms.
- Patient Education: Teach patients to recognize early warning signs such as dizziness, fatigue, dyspnea, or chest pain and to report these promptly.
Clinical Example:
In a patient taking carvedilol for chronic heart failure, nurses should maintain a monitoring log of daily blood pressure, heart rate, and weight, educating the patient to contact the clinic if heart rate drops below 50 bpm or weight increases by more than 2 kg in a week, which may indicate fluid retention.
Key Takeaway:
Through vigilant assessment, timely intervention, and patient education, nurses ensure nonselective beta blockers provide maximum therapeutic benefit while minimizing cardiovascular, respiratory, and systemic adverse effects.
Administration and Patient Education for Safe Beta-Blocker Use
Dosing and Switching Between Agents
Safe administration of nonselective beta blockers requires individualized dosing, careful titration, and attention to the specific beta-blocker therapy prescribed. Nurses must understand the pharmacologic differences among propranolol, carvedilol, and metoprolol to optimize therapeutic outcomes.
Dosing Considerations:
- Propranolol: Often administered orally in divided doses; for hypertension or angina, initial low doses (e.g., 40 mg twice daily) are titrated based on heart rate and blood pressure response.
- Carvedilol: Typically started at a low dose (e.g., 3.125 mg twice daily) in heart failure to minimize the risk of bradycardia or hypotension, with gradual titration every 1–2 weeks.
- Metoprolol: As a cardioselective beta blocker, dosing for hypertension or heart failure begins low (12.5–25 mg twice daily), with slow adjustments to achieve target heart rate and blood pressure.
Switching Between Agents:
- Switching may be indicated due to adverse effects, comorbidities, or suboptimal therapeutic response.
- Transitioning from a nonselective beta-blocker to a cardioselective agent (e.g., metoprolol) can reduce β2 blockade-related pulmonary complications, particularly in patients with asthma or chronic obstructive pulmonary disease (COPD).
- When switching, a gradual tapering of the first beta blocker is essential to prevent rebound hypertension, tachycardia, or angina exacerbation.
Nursing Monitoring During Titration:
- Regularly monitor heart rate, blood pressure, weight, and symptoms of heart failure.
- Assess for fatigue, dizziness, or worsening angina during titration.
- Document adverse effects and communicate with prescribers regarding dose adjustments.
Teaching Patients About Nonselective Beta-Blockers
Patient education is central to safe beta-blocker therapy. Nurses should ensure patients understand how to take a beta blocker correctly, recognize adverse effects, and implement lifestyle modifications to enhance efficacy.
Key Education Points:
- Adherence: Emphasize the importance of taking medication consistently, at the same time each day, and never abruptly stopping therapy to prevent rebound hypertension or heart rhythm complications.
- Recognizing Adverse Effects: Patients should be aware of symptoms such as fatigue, dizziness, bradycardia, shortness of breath, or worsening heart failure. Early reporting of these signs allows prompt intervention.
- Lifestyle Considerations: Encourage regular physical activity, low-sodium diet for heart failure, and avoidance of over-the-counter medications that may interact with beta blockers (e.g., decongestants containing epinephrine).
- Self-Monitoring: Patients may benefit from home blood pressure and heart rate monitoring to detect early signs of over- or under-treatment.
Example:
A patient with chronic heart failure prescribed carvedilol should be educated to check blood pressure twice daily, report sudden weight gain (>2 kg in a week), and note any worsening shortness of breath or fatigue. This proactive monitoring improves clinical outcomes and reduces hospitalizations.
Drug Interactions and Safety Warnings
Nonselective beta blockers interact with several medications, and nurses must provide guidance to ensure patient safety:
- Epinephrine Caution: During emergencies or dental procedures, patients on nonselective beta blockers are at risk for unopposed α1-mediated vasoconstriction, potentially causing severe hypertension. Nurses should educate patients to inform all healthcare providers about their beta-blocker therapy.
- Calcium Channel Blockers: Co-administration with agents like verapamil or diltiazem may excessively lower heart rate or depress cardiac contractility, increasing the risk of bradycardia or heart block. Nurses must monitor heart rate and blood pressure closely.
- Other Considerations: Advise caution with insulin or oral hypoglycemic agents, as β2 blockade may mask hypoglycemia symptoms, and with drugs that may potentiate hypotension.
Nursing Recommendations:
- Verify all medications before administration and maintain clear communication with prescribers.
- Educate patients on reporting new medications or supplements.
- Reinforce the importance of carrying a list of current medications, especially during emergencies or medical procedures.
Conclusion
Nonselective beta blockers remain a cornerstone of cardiovascular disease management, offering substantial benefits in heart failure, hypertension, angina, and certain arrhythmias. By blocking both β1 and β2 adrenergic receptors, these β-blockers exert powerful effects on heart rate, cardiac output, and blood vessel tone, ultimately reducing cardiac workload and improving patient outcomes. Understanding the pharmacology, mechanisms of blockade, and clinical nuances of nonselective beta-blocker therapy is essential for nurses, who play a pivotal role in monitoring, administering, and educating patients.
Nursing practice demands vigilance in recognizing contraindications—particularly in patients with asthma or chronic obstructive pulmonary disease—and monitoring for cardiovascular and systemic adverse effects such as bradycardia, hypotension, or rebound hypertension. Proper dosing, titration, and careful switching between agents like propranolol, carvedilol, and metoprolol can enhance safety while optimizing therapeutic benefit. Additionally, nurses must provide thorough patient education, emphasizing adherence, early recognition of side effects, lifestyle modifications, and awareness of drug interactions, including epinephrine and calcium channel blockers.
Ultimately, the role of nonselective beta blockers extends beyond pharmacology—they serve as a framework for holistic patient care, requiring integration of clinical knowledge, patient assessment, and education strategies. By understanding the mechanisms, indications, and precautions, nursing professionals can enhance patient safety, improve treatment adherence, and contribute meaningfully to the management of cardiovascular disease. This comprehensive approach ensures that nonselective beta-blockers are used effectively, safely, and in alignment with evidence-based practice, reinforcing the nurse’s role as both a clinician and patient educator.
Frequently Asked Questions
How to remember nonselective beta blockers?
A simple way to remember nonselective beta blockers is to focus on the ones that block both β1 and β2 receptors. Common examples include propranolol, carvedilol, and nadolol. A mnemonic: “PNC” – Propranolol, Nadolol, Carvedilol – Nonselective Coverage. These agents affect both the heart (β1) and lungs/blood vessels (β2).
How do nonselective beta blockers work?
Nonselective beta blockers inhibit both β1 and β2 adrenergic receptors, which leads to:
- β1 blockade: Reduces heart rate, contractility, and myocardial oxygen demand.
- β2 blockade: Can cause bronchoconstriction and mild vasoconstriction in blood vessels.
Overall, this decreases cardiac workload, lowers blood pressure, and helps control arrhythmias and angina.
What is the difference between selective and nonselective beta agonists?
- Selective beta agonists target one receptor subtype:
- β1 agonists: Primarily affect the heart (increase heart rate and contractility).
- β2 agonists: Primarily affect the lungs and blood vessels (cause bronchodilation and vasodilation).
- Nonselective beta agonists stimulate both β1 and β2 receptors, affecting heart rate and bronchial/lung function simultaneously.
Note: This is the opposite concept of blockers—agonists activate receptors, while beta blockers inhibit them.
Are selective or non-selective beta blockers better for anxiety?
- Nonselective beta blockers (like propranolol) are generally preferred for performance anxiety because they reduce physical symptoms such as tremors, palpitations, and rapid heart rate by blocking both β1 and β2 receptors.
- Cardioselective beta blockers (like metoprolol) primarily target β1, which may help anxiety-related palpitations but are less effective for tremors or peripheral adrenergic symptoms.
For nursing students: Propranolol is the classic choice for anxiety-related autonomic symptoms, but patient comorbidities (e.g., asthma) must be considered.
