Factor V Leiden and Thrombophilia Explained: Signs, Tests, and Preventing Abnormal Blood Clots
Blood coagulation is a normal physiological process that preserves circulatory integrity when a blood vessel is injured, forming a platelet‑fibrin plug to halt bleeding. However, when this delicate balance between clot formation and dissolution is disrupted, it can result in the formation of blood clots that impede normal blood flow and threaten organ function. One of the most studied genetic contributors to such disruption is factor v leiden, a variant in the gene encoding a critical element of the coagulation cascade. This inherited alteration is recognized as the most prevalent genetic cause of thrombophilia, a condition characterized by an increased tendency to develop clots in the venous system.
For nursing students, a solid understanding of Factor V Leiden and its clinical consequences is essential. Although many individuals carrying this genetic change remain asymptomatic throughout life, the presence of the variant can significantly influence a person’s risk of developing venous thrombotic events—particularly when additional risk factors are present. These events commonly manifest as clots in the deep veins of the legs or in the pulmonary circulation, requiring prompt clinical recognition and management.
This article explores the pathophysiology of Factor V Leiden and the mechanisms by which it contributes to abnormal clot formation, emphasizes how it alters the normal clotting response at the molecular level, and discusses how this predisposition intersects with other clinical variables. It also highlights the practical implications for nursing assessment, diagnosis, and prevention strategies, underscoring the importance of integrating genetic, biochemical, and clinical knowledge into patient care. By grounding the discussion in evidence‑based practice, nursing students will be better prepared to identify patients at risk, interpret diagnostic findings, and participate in multidisciplinary care aimed at reducing morbidity associated with inherited clotting disorders.
Understanding Factor V Leiden Thrombophilia and Its Impact on the Clotting Process
Proper blood coagulation is essential for preventing excessive bleeding when a blood vessel is injured. This process relies on a complex interaction of proteins known as coagulation factors, which work in a cascade to form a blood clot. Under normal conditions, this cascade is tightly regulated to ensure that clot formation stops once vascular integrity is restored. However, genetic variants like factor v leiden can disrupt this balance, increasing the risk of pathological clot formation, or thromboses. Understanding this pathophysiology is crucial for nursing students, as it informs both patient assessment and prevention strategies.
Proper blood coagulation is essential for preventing excessive bleeding when a blood vessel is injured. This process relies on a complex interaction of proteins known as coagulation factors, which work in a cascade to form a blood clot. Under normal conditions, this cascade is tightly regulated to ensure that clot formation stops once vascular integrity is restored. However, genetic variants like factor v leiden can disrupt this balance, increasing the risk of pathological clot formation, or thromboses. Understanding this pathophysiology is crucial for nursing students, as it informs both patient assessment and prevention strategies.
What is Factor V Leiden and How It Alters Normal Clotting
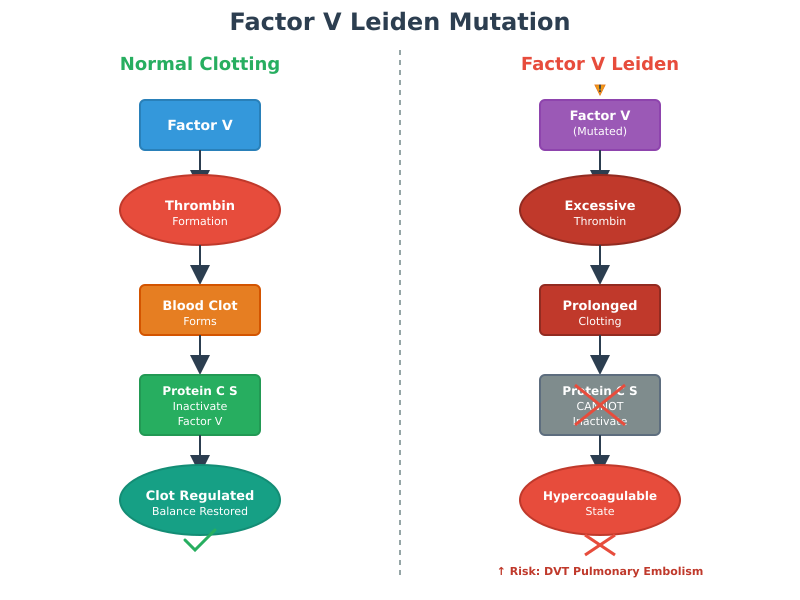
Normal Function of Factor V:
- Factor V protein is a cofactor in the coagulation cascade that enhances the conversion of prothrombin to thrombin, leading to fibrin formation and blood clotting.
- Once the clot has stabilized, regulatory proteins such as protein c and protein S inactivate normal factor v to prevent excessive clot growth.
- This regulation ensures a balance between clot formation and breakdown, preserving normal blood flow.
Impact of the Factor V Leiden Mutation:
- The factor v leiden mutation alters the structure of coagulation factor v, creating a protein resistant to inactivation by activated protein c.
- Resistance to activated protein C results in a prolonged clotting response, even when clot formation is no longer necessary.
- Consequences include a hypercoagulable state that increases the risk of developing abnormal blood clots in veins, particularly the deep veins of the legs (deep vein thrombosis) and the lungs (pulmonary embolism).
- This mutation represents the most common form of inherited thrombophilia, emphasizing its clinical relevance.
Clinical Implications for Patients:
- Individuals carrying one factor v leiden gene (heterozygous factor v leiden) have a moderate increase in clotting risk.
- Individuals with two copies of the factor (homozygous factor v leiden) face a substantially higher risk of thromboses and more severe complications.
- Certain physiological or environmental triggers, such as surgery, immobility, pregnancy, or use of estrogen-containing medications, can increase the risk factor v leiden thrombophilia beyond baseline levels.
Activated Protein C Resistance and Increased Clotting Risk
Mechanism of APC Resistance:
- Activated protein c normally inactivates factor V to limit blood coagulation after a clot has formed.
- In people with factor v leiden, the mutation prevents effective cleavage of factor V, allowing continued thrombin generation.
- This resistance leads to a tendency to form abnormal blood clots, even in the absence of overt vascular injury.
Consequences of APC Resistance:
- Unchecked thrombin activity increases the likelihood of developing a blood clot in both superficial and deep veins.
- Patients may present with asymptomatic thromboses that only become clinically apparent when a clot obstructs blood flow or migrates to the lungs as a pulmonary embolism.
- APC resistance is a primary contributor to the risk of developing blood clots in carriers of the mutation.
Why Factor V Leiden is the Most Common Inherited Thrombophilia
Prevalence and Genetic Patterns:
- Leiden is the most common inherited cause of venous thromboses.
- It occurs in approximately 3–8% of individuals of European descent and is less common in other populations.
- Both heterozygous factor v leiden and homozygous factor v leiden carriers demonstrate elevated clotting risk, with homozygous individuals experiencing a markedly higher likelihood of developing abnormal blood clots.
Clinical Significance:
- The mutation impacts how clotting factors respond to physiological stress, surgical interventions, or hormonal changes, particularly in women with factor v leiden.
- Understanding the gene dosage effect is critical for nursing care planning, risk assessment, and preventive interventions.
- The presence of a factor v protein alteration informs the need for diagnosis and treatment, including patient education on avoiding situations that increase thrombosis risk.
Recognizing Symptoms of Factor V Leiden and Blood Clots
The clinical presentation of factor v leiden and related thrombophilia varies widely, ranging from asymptomatic carriers to patients presenting with life-threatening clotting events. Early recognition of signs and symptoms is critical, as timely intervention can prevent the development of severe complications such as pulmonary embolism or long-term vascular damage. Nursing students must understand both the subtle and overt manifestations of abnormal clot formation to provide proactive care.
Common Manifestations: Deep Vein Thrombosis and Pulmonary Embolism
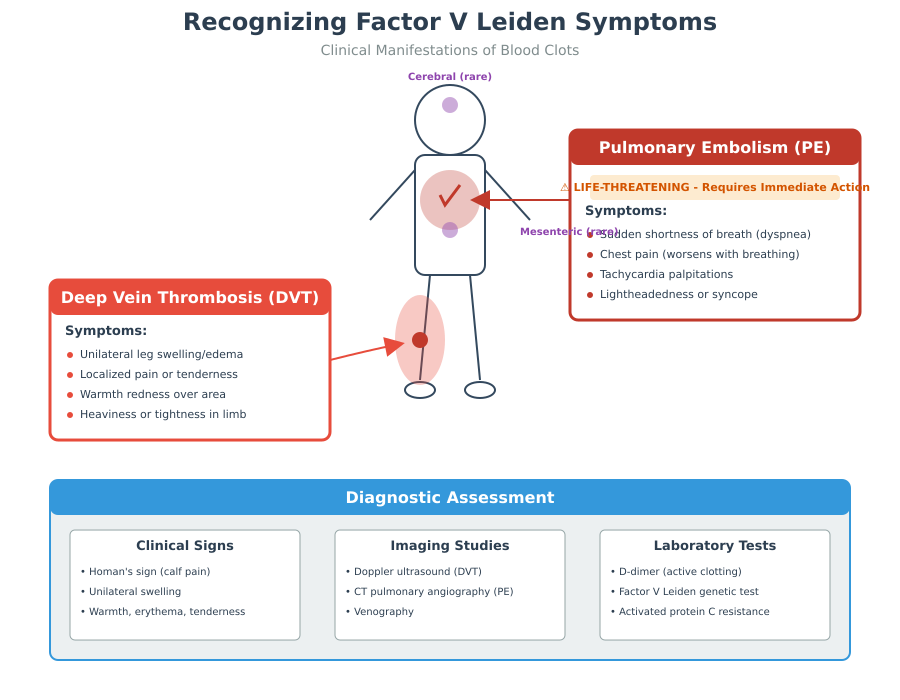
Deep Vein Thrombosis (DVT):
- DVT is the most frequent clinical manifestation of people with factor v leiden, occurring when a blood clot forms in the deep veins, typically of the legs.
- Symptoms of factor v leiden-related DVT include:
- Unilateral leg swelling or edema
- Localized pain or tenderness along the course of the vein
- Warmth, redness, or skin discoloration over the affected area
- A feeling of heaviness or tightness in the limb
Pulmonary Embolism (PE):
- PE occurs when part of a clot detaches and travels through the venous system to the lungs.
- Clinical signs may include:
- Sudden shortness of breath or dyspnea
- Chest pain that worsens with inspiration
- Tachycardia and palpitations
- Lightheadedness, syncope, or hypoxemia in severe cases
- Nursing assessment should prioritize early detection, as PE can rapidly become fatal if untreated.
Example: A 32-year-old woman with a history of carry the factor v leiden presents with unilateral calf swelling and mild pain. Recognizing these early DVT signs allowed prompt imaging and diagnosis and treatment, preventing a potential PE.
Identifying Abnormal Blood Clots in Blood Vessels
Locations and Presentation:
- Deep veins: Swelling, tenderness, erythema, and warmth
- Superficial veins: Palpable cord, localized redness, mild discomfort
- Pulmonary arteries: Dyspnea, tachypnea, pleuritic chest pain
- Mesenteric or cerebral vessels (rare): Abdominal pain, neurological deficits
Diagnostic cues:
- Positive Homan’s sign (pain in calf with dorsiflexion) – supportive but not definitive
- Imaging such as Doppler ultrasonography for DVT or CT pulmonary angiography for PE
- Laboratory tests, including D-dimer, may indicate active clot formation
Complications if untreated:
- Chronic venous insufficiency
- Pulmonary hypertension secondary to recurrent PE
- Risk of developing abnormal blood clots that can cause organ ischemia
Unique Considerations in Women: Pregnancy and Hormonal Risks
- Pregnancy: Increases clotting factors, reduces fibrinolytic activity, and physically compresses veins, elevating risk of blood clots in women with factor v leiden.
- Oral contraceptives or hormone replacement therapy: Estrogen increases the risk of developing abnormal blood by further reducing natural anticoagulant activity.
- Clinical approach: Nurses should assess hormonal status, obstetric history, and family history of inherited blood conditions to determine risk and implement preventive strategies.
Example: A pregnant woman with heterozygous factor v leiden may be prescribed low-dose blood thinners to prevent blood clots during high-risk periods such as the third trimester or postpartum.
Nursing Perspective: Bedside Assessment of Thromboses
Key Assessment Strategies:
- Conduct regular extremity checks for swelling, tenderness, and discoloration
- Monitor vital signs for tachycardia, hypoxia, or sudden hypotension that may indicate PE
- Assess for signs and symptoms of clot migration, including chest pain or sudden shortness of breath
- Evaluate patient history for history of blood clots, carry the factor v leiden, or other risk factors
Nursing Actions:
- Early recognition of DVT or PE allows timely initiation of blood thinners or other temporary treatment with an anticoagulant
- Educate patients on warning signs, such as calf pain, swelling, or unexplained shortness of breath
- Document and report changes promptly to the healthcare team for further intervention
Example: In a postoperative patient known to carry the factor v leiden, routine monitoring revealed calf swelling and tenderness. Early identification and initiation of prophylactic blood thinners prevented progression to PE.
Diagnosis and Testing for Factor V Leiden Thrombophilia
Accurate diagnosis of factor v leiden thrombophilia is critical for identifying individuals at heightened risk of developing blood clots, guiding diagnosis and treatment, and implementing preventive measures to avoid life-threatening complications like pulmonary embolism or recurrent deep vein thrombosis. Unlike many acquired clotting disorders, Factor V Leiden is an inherited clotting disorder, meaning that genetic factors directly influence the clotting process. Nursing students must understand the various diagnostic tools, their indications, and how genetic and functional results inform clinical decisions.
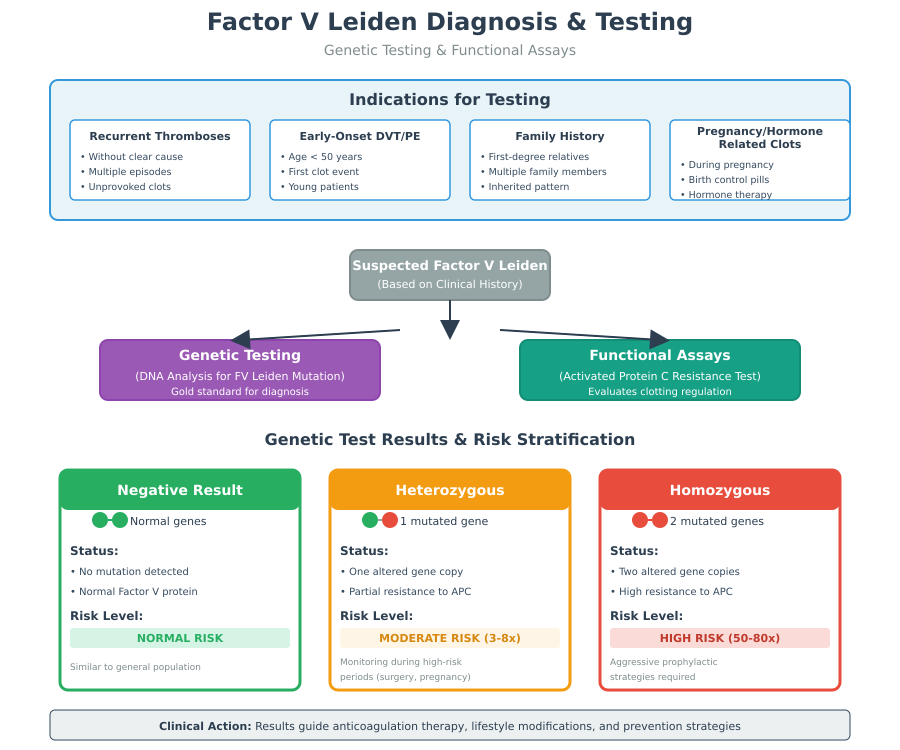
Diagnosis typically involves a combination of:
- Genetic testing, which identifies the specific factor v leiden mutation at the DNA level
- Functional assays, which evaluate the activity of activated protein c and overall clotting regulation
Together, these tests provide a complete picture of a patient’s risk and inform interventions such as anticoagulation therapy or lifestyle modifications.
Genetic Testing for the Factor V Gene
Purpose and Role in Diagnosis:
- Genetic test for the factor v gene detects the single-point substitution responsible for the Leiden mutation.
- This mutation alters factor v protein, making it resistant to inactivation by activated protein c, which leads to a hypercoagulable state.
- The test is particularly indicated in patients with:
- Recurrent thromboses without clear provoking factors
- Early-onset deep vein thrombosis or pulmonary embolism
- Strong history of blood clots in first-degree relatives
- Pregnancy or hormone therapy-related thrombotic events in women with factor v leiden
Interpretation of Results:
- Negative result: No mutation; clotting risk is similar to the general population unless other risk factors are present.
- Heterozygous factor v leiden: One altered copy of the factor v gene, moderate increase in risk of blood clots, may require monitoring during high-risk periods.
- Homozygous factor v leiden: Two copies of the factor v gene; significantly higher risk of developing abnormal blood clots. These patients often require more aggressive prophylactic strategies.
Clinical Example:
A 30-year-old patient with recurrent leg thromboses underwent testing for factor v leiden, confirming one altered gene. This diagnosis of factor v leiden prompted counseling on preventing blood clots during future surgeries or travel.
Functional Assays: Protein C and Activated Protein C Resistance Tests
Purpose of Functional Testing:
- While genetic testing identifies the presence of the mutation, functional assays assess how the patient’s blood responds to natural anticoagulant mechanisms.
- Activated protein c (APC) resistance test measures the ability of activated protein c to slow blood coagulation.
- A shortened clotting time in the presence of APC indicates resistance and suggests a pro-thrombotic state.
Key Assays:
- Activated Protein C Resistance Test:
- Patient plasma is exposed to APC.
- Normally, APC slows the clotting cascade by inactivating factor v.
- In people who have the factor v leiden, the abnormal factor v resists inactivation, allowing blood coagulation to proceed unchecked, increasing risk for developing blood clots.
- Protein C Activity Test:
- Measures plasma levels of functional protein c.
- Low activity may point to a coexisting deficiency or other clotting factor abnormalities.
- Provides context for interpreting APC resistance in complex cases.
Clinical Example:
A patient with mild calf swelling and no prior history of thromboses was found to have abnormal APC resistance, indicating the factor v leiden mutation increases clotting risk. The result guided prophylactic use of blood thinners during high-risk situations.
Interpreting Heterozygous vs. Homozygous Status
Heterozygous Factor V Leiden:
- Presence of one factor v leiden gene (heterozygous) confers a moderate risk of developing blood clots.
- These patients often remain asymptomatic until additional risk factors (immobility, surgery, pregnancy, oral contraceptives) trigger clot formation.
- Nursing implications:
- Patient education on signs and symptoms of developing a blood clot
- Guidance on lifestyle measures to prevent blood clots
- Consideration for temporary blood thinners during high-risk periods
Homozygous Factor V Leiden:
- Two copies of the factor (homozygous) create a high-risk state, with significantly elevated probability of developing abnormal blood clots.
- These patients may require long-term anticoagulation or intensive risk assessment for procedures.
- Nursing considerations:
- Close monitoring for early signs of deep vein thrombosis or pulmonary embolism
- Collaboration with healthcare providers to develop individualized prophylaxis plans
Clinical Example:
A 50-year-old male, homozygous for the factor v leiden mutation, was advised to undergo regular monitoring and temporary anticoagulation prior to elective orthopedic surgery to reduce risk of abnormal blood clots.
Nursing Implications
- Recognize when patients require testing for factor v leiden based on history or clinical presentation.
- Understand the difference between genetic tests (identify mutation) and functional assays (assess clotting behavior).
- Educate patients about the significance of heterozygous vs. homozygous status for risk of blood clots.
- Collaborate with multidisciplinary teams to implement preventive measures, including temporary treatment with an anticoagulant, blood thinners, and lifestyle modifications.
Risk Factors for Blood Clot Formation in Factor V Leiden
The risk of developing blood clots in patients with factor v leiden is influenced by both intrinsic and extrinsic factors. Intrinsic risk stems from the genetic alteration itself: the factor v gene mutation produces abnormal factor v that is resistant to activated protein c, impairing the body’s natural anticoagulation mechanisms. This predisposition forms the baseline susceptibility to thromboses, meaning even minor vascular injuries or temporary immobilization can trigger clot formation.
Extrinsic or acquired risk factors further elevate the risk. These include prolonged immobilization, obesity, smoking, trauma, and certain medications. For example, a sedentary adult carrier who undertakes long-haul travel without frequent movement is at higher risk for deep vein thrombosis, highlighting the importance of lifestyle considerations in nursing assessment and patient education.
How Factor V Leiden Increases Blood Clot Risk Compared to Other Disorders
Compared with other inherited or acquired clotting disorders, factor v leiden confers a significant but variable increase in thrombotic risk. Heterozygous carriers have a moderately elevated risk, estimated at 3–8 times that of the general population, while homozygous carriers face substantially higher risk. In contrast, rarer inherited deficiencies such as protein C, protein S, or antithrombin deficiency confer higher individual clotting risk but are far less common in the population.
Factor V Leiden is also unique because it combines high prevalence with measurable clinical impact, making it the most frequently encountered inherited blood clotting disorder. For instance, two patients may have different inherited thrombophilias: a patient with protein C deficiency might have a higher individual risk, but a patient with Factor V Leiden is more likely to be encountered in clinical practice, emphasizing the need for nurses to recognize early signs and symptoms.
Clinical Example:
A 35-year-old patient presenting with recurrent thromboses without identifiable triggers might be evaluated first for factor v leiden mutation, given its prevalence, before testing for rarer coagulation abnormalities.
Additional Risk Factors: Oral Contraceptives, Surgery, and Pregnancy
Certain modifiable and situational factors dramatically increase the likelihood of developing abnormal blood clots in people with factor v leiden.
- Oral contraceptives and hormone therapy: Estrogen-containing medications increase coagulation factor activity, amplifying clotting tendencies in carriers. Nursing staff must counsel women with Factor V Leiden on safer contraceptive options and monitor for symptoms of factor v leiden during use.
- Surgery and immobilization: Major procedures, particularly orthopedic and abdominal surgeries, elevate risk for developing blood clots due to temporary venous stasis and endothelial injury. Nurses play a key role in perioperative assessment, ensuring early ambulation and considering prophylactic blood thinners.
- Pregnancy and postpartum period: Physiologic hypercoagulability during pregnancy heightens clot risk. Women with Factor V Leiden may require closer surveillance and prophylactic anticoagulation. Nurses are essential in monitoring for early deep vein thrombosis or pulmonary embolism and educating patients on warning signs.
Clinical Example:
A 29-year-old woman with heterozygous Factor V Leiden planning pregnancy may need personalized counseling on risk of blood clots and preventive measures such as low-molecular-weight heparin during high-risk periods.
Population and Demographic Prevalence
Factor V Leiden is the most common inherited thrombophilia in people of European descent, with heterozygosity present in 3–8% of this population. Its prevalence is lower among African, Asian, and indigenous populations. Certain regions, like southern Sweden and Greece, report frequencies as high as 15%.
Understanding these demographic patterns informs screening decisions and risk assessment in clinical practice. Nurses should consider family history, ethnic background, and prior history of blood clots when evaluating patients. For example, a nurse assessing a patient of European ancestry with a family history of DVT should consider the higher probability of carrying the factor v leiden when planning diagnostic testing and preventive strategies.
Clinical Implication:
Population prevalence data help prioritize genetic test screening for high-risk patients, enabling early identification and intervention to prevent blood clots.
Prevention and Treatment of Blood Clots in Factor V Leiden Thrombophilia
Managing the risk of thrombosis in individuals with factor v leiden thrombophilia requires a multifaceted approach that combines both pharmacologic and lifestyle strategies. Because this inherited condition predisposes patients to inappropriate formation of blood clots, it is critical that nursing students understand not only how to intervene when a clot forms, but also how to prevent clot development in the first place. This section explores evidence‑based preventative measures, the role of medications, long‑term management strategies, and lifestyle modifications that together form an effective care plan.
Role of Anticoagulants and Blood Thinners in Prevention and Management
Anticoagulant therapy — often referred to as blood thinners — is central to both preventing initial clot formation and treating existing venous thromboembolism, especially in high‑risk individuals with a known genetic predisposition. These medications work by interfering with components of the clotting cascade, slowing the rate at which fibrin and platelets accumulate to form a stable clot.
Mechanism and Indications:
- Vitamin K antagonists (e.g., warfarin) reduce the liver’s ability to produce certain clotting proteins.
- Direct oral anticoagulants (DOACs) (e.g., rivaroxaban, apixaban) target specific enzymes in the coagulation pathway, such as Factor Xa, to reduce thrombin generation.
- Low‑molecular‑weight heparin (LMWH) is often used temporarily in acute settings or perioperative periods because of its predictable effect and ease of dose adjustment.
Anticoagulation is generally indicated when a patient with Factor V Leiden presents with a documented thrombotic event (e.g., after imaging confirms a clot) or when they face a significant transient risk (such as major surgery or prolonged immobilization).
Example:
A 42‑year‑old patient admitted with leg pain and swelling undergoes ultrasound confirmation of a clot in a deep leg vein. Initiation of a DOAC leads to stabilization, symptom improvement over several days, and a plan for continued anticoagulation under specialist guidance.
Nursing Considerations:
- Monitor for signs of bleeding (e.g., bruising, hematuria).
- Educate patients on dosage timing and interactions (e.g., with foods high in vitamin K if on warfarin).
- Ensure scheduled laboratory monitoring where required (especially for warfarin) and follow up on INR values.
Long-Term Risk Management for Individuals with Factor V Leiden
After the initial management of thrombosis, many patients face decisions about how to prevent blood clots over the long term. The goal is to balance effective prevention with minimizing medication side effects, particularly bleeding. A lifelong prevention strategy is not required for every person with the mutation; instead, it is based on individualized risk profiles.
For patients with a single genetic variant (heterozygous factor v leiden) and no prior clotting events, long‑term anticoagulation is often not recommended unless additional risk factors are present. Regular clinical follow‑up includes:
- Periodic assessment of activity levels and mobility.
- Reassessment before high‑risk situations (e.g., surgery, long flights, pregnancy).
- Routine education on early signs and symptoms of thrombosis.
In contrast, individuals with a more intense genetic risk (e.g., two copies of the variant) or a history of recurrent clotting events may require indefinite anticoagulation. In these cases, collaborative management between primary care, hematology, and nursing staff ensures appropriate surveillance for complications and adjustments based on life changes.
Lifestyle Modification vs. Medical Prophylaxis
Effective thrombosis prevention extends beyond medications. Lifestyle interventions play a crucial role, particularly in patients who are not on chronic anticoagulants.
Mobility and Activity:
Frequent ambulation — especially during periods of prolonged sitting (such as long airplane flights) — improves venous return from the legs and reduces stasis, a key component of pathological clot formation.
Hydration and Diet:
Adequate fluid intake supports optimal blood viscosity. While there is no specific clot‑preventive diet, maintaining a healthy weight and balanced nutrition reduces a spectrum of risk factors (such as obesity and chronic inflammation) that compound genetic susceptibility.
Avoiding Modifiable Risks:
Smoking cessation, regular cardiovascular exercise, and avoiding prolonged immobilization are simple but powerful strategies. For patients preparing for surgery or with temporary mobility restrictions, nurses often recommend graduated compression stockings or prophylactic anticoagulation under physician guidance.
Example:
A 55‑year‑old patient with a family history of thrombosis plans a long vacation involving several days of travel. Nursing guidance includes advice on leg exercises during travel, frequent hydration, and wearing compression stockings to support circulation — nonpharmacologic measures that complement clinical vigilance.
Synthesizing Prevention and Treatment
For individuals with inherited clotting predispositions, prevention and treatment of blood clots must be tailored. Pharmacologic strategies — especially anticoagulants — are foundational but must be balanced with bleeding risk and lifestyle needs. Comprehensive care includes:
- Early recognition of clotting events
- Appropriate use of anticoagulant therapy
- Longitudinal risk assessment and patient education
- Empowering patients with practical lifestyle adjustments
Nursing Considerations in Factor V Leiden and Thrombophilia Care
Caring for patients with factor v leiden thrombophilia requires a multifaceted nursing approach that integrates assessment, monitoring, patient education, and clinical intervention. Because carriers have an increased risk of developing abnormal blood clots, nurses play a central role in early detection, prevention, and long-term management. Understanding the interplay of genetic predisposition, situational risk factors, and patient lifestyle is essential for safe and effective care.
Monitoring and Assessment of Patients at Risk
Early recognition of thromboses is critical in preventing complications such as pulmonary embolism or extensive deep vein thrombosis. Nurses should employ a combination of bedside assessment techniques, vital sign monitoring, and patient history evaluation to detect early warning signs of abnormal blood clot formation.
Key monitoring strategies include:
- Physical Assessment: Inspect for swelling, redness, warmth, and tenderness in extremities, which may indicate deep vein thrombosis. Assess for signs and symptoms such as sudden chest pain, shortness of breath, or hemoptysis, which could suggest pulmonary embolism.
- Vital Signs Monitoring: Observe for tachycardia, hypotension, or low oxygen saturation, as these may be early indicators of significant clotting events.
- Patient History and Risk Evaluation: Regularly evaluate risk factors, including prior history of blood clots, recent surgery, immobility, or hormone therapy, to anticipate high-risk periods.
Example:
A patient recovering from hip surgery who carries a heterozygous factor v leiden mutation is assessed daily for leg swelling, calf tenderness, and pulse discrepancies. Early identification allows prompt intervention with blood thinners, reducing the risk of developing blood clots.
Critical Nursing Actions During Thromboses or Vascular Injury
Immediate intervention is required when a patient presents with a suspected thrombotic event. Nurses must act quickly to reduce morbidity and prevent progression of thromboses or abnormal blood clot formation.
Priority actions include:
- Rapid Assessment and Escalation: Evaluate symptoms, vital signs, and oxygenation. Notify the medical team immediately if there is evidence of pulmonary embolism or extensive clotting.
- Initiation of Protocols: Ensure timely administration of blood thinners or anticoagulants as ordered. In acute care settings, mechanical interventions such as compression devices or limb elevation may be employed.
- Monitoring for Complications: Watch for bleeding or hemodynamic instability, particularly when anticoagulation therapy has been started.
Example:
A patient with factor v leiden suddenly develops unilateral leg swelling and calf pain. The nurse quickly performs a bedside assessment, elevates the leg, applies compression stockings as per protocol, and notifies the physician. Early intervention enables temporary treatment with an anticoagulant, preventing clot propagation and potential pulmonary embolism.
Patient Education and Counseling
Education is a cornerstone of thrombophilia care, empowering patients to participate actively in preventing blood clots and managing factor v leiden thrombophilia. Nurses translate complex genetic and pharmacologic information into practical guidance tailored to the patient’s daily life.
Key counseling points include:
- Understanding Genetic Results: Explain the difference between heterozygous and homozygous factor v leiden gene status, implications for risk of developing abnormal blood clots, and the importance of family screening.
- Lifestyle and Risk Reduction: Advise on mobility strategies, hydration, maintaining a healthy weight, and avoiding smoking. Counsel women on hormonal risk factors, including oral contraceptives, and strategies to reduce clotting risk during pregnancy.
- Medication Adherence: Educate patients on proper administration of blood thinners, including timing, potential interactions, and signs of bleeding. Stress the importance of consistent follow-up and laboratory monitoring when required.
- Recognizing Early Symptoms: Teach patients how to identify early signs and symptoms of DVT or pulmonary embolism, such as swelling, redness, shortness of breath, and chest pain, and to seek immediate medical attention.
Example:
A nurse meets with a patient recently diagnosed with factor v leiden thrombophilia. Using visual aids, the nurse explains how a mutation in factor v increases the likelihood of developing a blood clot, demonstrates leg exercises to improve circulation, and provides a medication calendar for anticoagulant therapy. The patient gains a clear understanding of preventive steps and warning signs, improving adherence and outcomes.
Conclusion
Factor V Leiden thrombophilia represents the most common inherited clotting disorder, with a well-established predisposition to develop blood clots due to a factor v leiden mutation. At the core of this condition is a disruption in the clotting process, where the protein called factor v becomes resistant to activated protein c, impairing the natural anticoagulation mechanisms and increasing the risk of developing abnormal blood clots. Understanding the pathophysiology is essential for nursing students, as it informs assessment, monitoring, and interventions in both acute and long-term care settings.
Clinical recognition is crucial because early signs and symptoms of thromboses—including deep vein thrombosis and pulmonary embolism—can be subtle yet potentially life-threatening. Nurses play a pivotal role in bedside evaluation, including assessment for limb swelling, tenderness, discoloration, and systemic indicators such as tachycardia or hypoxia. Prompt identification of these symptoms of factor v leiden allows rapid intervention, often involving blood thinners or temporary anticoagulant therapy, preventing progression to severe thrombotic events.
Accurate diagnosis and treatment rely on a combination of genetic testing for the factor v gene, functional assays assessing protein c activity, and evaluation of activated protein c resistance. Differentiating between heterozygous factor v leiden and homozygous factor v leiden carriers guides individualized care planning, influencing decisions regarding prophylactic anticoagulation, long-term monitoring, and lifestyle interventions. Nursing students must understand the implications of these test results to educate patients, support shared decision-making, and anticipate potential complications.
Prevention strategies extend beyond pharmacologic management. Lifestyle modification—including regular mobility, adequate hydration, weight management, and avoidance of smoking—works synergistically with clinical interventions to reduce risk of blood clots. In high-risk situations such as surgery, pregnancy, or prolonged immobility, nurses implement appropriate prophylactic measures, including blood thinners or mechanical compression devices, while ensuring patient adherence and understanding.
Patient-centered care remains the foundation of thrombophilia management. Effective nursing practice integrates assessment, education, and advocacy. Nurses educate patients about their inherited blood clotting disorder, explain the role of the factor v protein and abnormal factor v leiden, guide them on identifying early signs and symptoms, and provide practical instructions for preventing blood clots. This empowerment enhances adherence, reduces anxiety, and improves overall outcomes.
In conclusion, caring for individuals with factor v leiden thrombophilia requires a combination of scientific knowledge, clinical vigilance, and compassionate patient engagement. Nurses are uniquely positioned to bridge the gap between complex pathophysiology and daily self-care practices, ensuring early detection of thromboses, effective implementation of preventive strategies, and sustained patient education. By integrating these approaches, nursing professionals can reduce the incidence of abnormal blood clots, support long-term wellness, and promote safety in both acute and community care settings.
Frequently Asked Questions
What is thrombophilia and factor V Leiden?
Thrombophilia is a condition in which a person has an increased tendency to develop abnormal blood clots due to inherited or acquired defects in the clotting process. Factor V Leiden is the most common inherited thrombophilia, caused by a mutation in the factor v gene. This mutation produces an abnormal factor v protein that disrupts normal anticoagulation, predisposing individuals to blood clots such as deep vein thrombosis (DVT) or pulmonary embolism (PE).
How does factor V Leiden stop the clot?
Actually, factor V Leiden does not stop clots effectively. Normally, factor v helps in the clotting process, and activated protein c regulates clot formation by inactivating factor v to prevent excessive clotting. In factor V Leiden, the factor v protein becomes resistant to activated protein c, which means the clotting cascade continues unchecked, increasing the risk of developing abnormal blood clots.
How does factor V Leiden disorder increase the risk of an affected individual developing a DVT or PE?
Because activated protein c resistance prevents proper inactivation of factor v, the blood of affected individuals has a tendency to form abnormal blood clots more easily. These clots often form in deep veins, leading to deep vein thrombosis, and can dislodge and travel to the lungs, causing a pulmonary embolism. The risk is higher in homozygous factor v leiden carriers, during periods of immobility, surgery, pregnancy, or hormonal therapy.
What are the three most significant risk factors for clot formation?
The three key risk factors that significantly increase clot formation in patients with factor v leiden thrombophilia are:
- Genetic predisposition – carrying one or two copies of the factor v leiden gene.
- Hormonal influences – use of oral contraceptives, hormone replacement therapy, or pregnancy.
- Prolonged immobilization or surgery – situations that slow blood flow in blood vessels and enhance thromboses risk.
