Comprehensive Focused Soap Note for Schizophrenia Spectrum Other Psychotic and Medication-Induced Movement Disorders
Subjective
Chief Complaint (CC): “I was living with my mom, and she died. I was living and not bothering anyone, and those people– those people, they just will not leave me alone”.(Comprehensive Focused Soap Note for Schizophrenia Spectrum Other Psychotic and Medication-Induced Movement Disorders)
History of Presenting Illness: S.T. is a 53-year-old African-American male accompanied by his sister for a psychiatric evaluation. The patient reports that these people constantly watch him and will not leave him alone. During the visit, he reports that people outside are watching him; he hears them talking and sees shadows. He also sees a flying bird and hears heavy metal music that others do not hear. ST also reports that voices have become too loud for him to sleep, making him remain awake for extended durations. The patient believes the spies broke into the house to poison his food, but he managed to outsmart them by hiding everything in the fridge. He calls 911 to report the spies. The patient reports that he cannot go to the grocery but relies on his sister to avoid the spies. He suspects his sister has collaborated with the government to tap his phone. During the interview, ST enquired whether he was allowed to smoke and challenged his fatty liver diagnosis, claiming aliens must have summoned the doctors.(Comprehensive Focused Soap Note for Schizophrenia Spectrum Other Psychotic and Medication-Induced Movement Disorders)

Past Psychiatric History: ST has been hospitalized in the past due to Schizophrenia
Hospitalizations: He has been hospitalized three times in his 20s.
Medication trials: ST claimed Seroquel is benefiting him. Risperidone has gynecomastia side effects, while he does not like Haldol and Thorazine.(Comprehensive Focused Soap Note for Schizophrenia Spectrum Other Psychotic and Medication-Induced Movement Disorders)
Psychotherapy or Previous Psychiatric Diagnosis: The patient has received outpatient and inpatient psychiatric treatment before.
Substance Use History: ST smokes three packs of cigarettes and drinks beer daily. He was smoking marijuana three years ago before his mother passed away.(Comprehensive Focused Soap Note for Schizophrenia Spectrum Other Psychotic and Medication-Induced Movement Disorders)
Family Psychiatric/Substance Use History: The patient’s father has paranoid Schizophrenia, while his mother was diagnosed with anxiety.
Social History: ST is unemployed. His education level is 10th grade. His mother and sister raised him. He was living with his mother three years ago before she died, but now lives with his sister. ST reports that his father roughed him up as a child.(Comprehensive Focused Soap Note for Schizophrenia Spectrum Other Psychotic and Medication-Induced Movement Disorders)
Medical History: Fatty live disease and diabetes.
Current Medications: Metformin.
Allergies: No known food or drug allergies.
Reproductive: The patient has no children.
Review of Systems (ROS)
General: The patient denies any recent fevers, weight loss, fatigue, chills, cold or heat intolerance
HEENT: ST has not experienced any headaches, dizziness, head injuries, or visual issues such as double vision, eye discharge, yellowing of the sclera, ear discharge, or pain or hearing loss. The patient has also not experienced loss of smell, runny nose, sneezing, nasal congestion, voice hoarseness, sore throat, or difficulty swallowing.(Comprehensive Focused Soap Note for Schizophrenia Spectrum Other Psychotic and Medication-Induced Movement Disorders)
Skin: He does mention any rashes, itches, or skin tone changes.
Cardiovascular: ST does complain of palpitations, chest pain, swollen limbs, or shortness of breath.
Respiratory: He does not mention any cough, wheezing, sputum production, or difficulty in breathing.
Gastrointestinal: ST did not mention anorexia, vomiting, diarrhea, abdominal pain, or appetite loss.
Genitourinary: ST denies painful urination, incontinence, blood in urine, and decreased urine output.
Neurological: ST denies seizures, numbness, tingling sensations, syncope, limb paralysis
Musculoskeletal: ST also denies painful joints or muscles, muscle weakness, and joint swelling.
Hematologic: The patient denies anemia, bruising, and blood transfusions.
Lymphatics: ST has not had a splenectomy or swollen lymph nodes.
Endocrine: He also denies any intolerance to heat or cold, excessive thirst, sweating, or urination.
Objective Assessment
Physical exam: Deferred
Diagnostic Results/ Tests: There were no diagnostic tests conducted for ST. However, laboratory tests need to be assessed to exclude medical conditions that mimic psychotic symptoms or disorders (LaHue & Douglas, 2022). The diagnostic tests include complete blood count, Vitamin B12 levels, thyroid function tests, drug screening, comprehensive metabolic panel or serology tests. Brain CT scans, or MRIs, are instrumental in ruling out structural problems leading to psychotic symptoms.(Comprehensive Focused Soap Note for Schizophrenia Spectrum Other Psychotic and Medication-Induced Movement Disorders)
Assessment
Mental Status Examination
ST is a 53-year-old male who appears well-developed and nourished for his age. The patient maintained eye and was calm, alert, and cooperative during the interview. His attire and grooming were appropriate and maintained. ST was oriented to place and person, although his orientation to time was impaired. He was audible and used normal tone and volume to communicate. The patient’s mood was stable, but he encountered paranoia and smiled appropriately. The patient has visual and auditory hallucinations and claims the government is after him. Clang associations and flight of ideas were also observed when the patient claimed his taxes were so high. The interview process was partially impaired as the patient had visual hallucinations of a flying bird. However, the patient denied suicidal or self-harm idealizations and had no motor movement abnormalities.(Comprehensive Focused Soap Note for Schizophrenia Spectrum Other Psychotic and Medication-Induced Movement Disorders)
Diagnoses
Schizophrenia 295.90 (F20.9) – Primary Diagnosis
Schizophrenia is a complex mental health disorder marked by altered reality interpretation. The primary presentations for the condition entail auditory hallucinations, persecutory delusions, neurocognitive defects, disorders of thinking or speech, abnormal motor activity, and depression (Wong et al., 2022). According to DSM-TR-5, the patient must present with two or more of the listed symptoms and social dysfunction for one month or less if treated successfully to be diagnosed with Schizophrenia (American Psychiatric Association, 2022). The patient’s symptoms are consistent with Schizophrenia as the patient presented with auditory and visual hallucinations, persecutory delusions in the belief of government spies for high taxes, and sleep disruptions. The patient also confirmed the symptoms have lasted weeks and weeks and longer, which is more than one month, confirming the diagnosis.(Comprehensive Focused Soap Note for Schizophrenia Spectrum Other Psychotic and Medication-Induced Movement Disorders)
Differential Diagnoses
Delusional Disorder (F22)
Delusional disorder is a distinct mental health disorder separate from classical Schizophrenia. The DSM-TR-5 criteria for delusional disorder claims that a patient must have false beliefs persisting for at least a month without any other psychosis symptoms (American Psychiatric Association, 2022). The patient’s symptoms should also not meet the criteria for Schizophrenia for delusional disorder diagnosis to be confirmed. The typical delusional disorder symptoms include hallucinations associated with delusions, impaired concentration, irrational suspicions or thoughts, irritability, social withdrawal, or problems. While ST meets the criteria for a delusional disorder diagnosis, his symptoms are more related to Schizophrenia, making it the primary diagnosis. (Comprehensive Focused Soap Note for Schizophrenia Spectrum Other Psychotic and Medication-Induced Movement Disorders)
Schizophreniform Disorder (F2081)
Schizophreniform disorder is a psychotic problem affecting peoples’ thoughts, behavior, and perception of reality. The primary presentation for the disorder entails hallucinations, delusions, strange behavior, poor hygiene, low energy, self-isolation, and lack of interest. According to DSM-TR-5, patients meet the Schizophreniform diagnosis when they experience at least one of the mentioned symptoms for not more than six months (Maj et al., 2021). Although ST meets the criteria for Schizophreniform diagnosis, he has experienced his symptoms for more than six months, making the diagnosis a differential diagnosis.(Comprehensive Focused Soap Note for Schizophrenia Spectrum Other Psychotic and Medication-Induced Movement Disorders)
Case Formulation and Treatment
This case study involves a 53-year-old African-American male who complains of people who will not leave him alone. The patient thinks the people are spies from the government. During the interview, he hears heavy music and sees shadows and a flying bird. The patient is paranoid and accuses his sister of working with the government to bug his phone. ST’s symptoms of visual and auditory hallucinations, persecutory delusions, and social disturbances confirm Schizophrenia as the primary diagnosis based on the DSM-TR-5 criteria.(Comprehensive Focused Soap Note for Schizophrenia Spectrum Other Psychotic and Medication-Induced Movement Disorders)
The primary goal of treatment entails treating the symptoms and preventing psychotic symptoms. Therefore, psychotherapy and pharmacological treatment will effectively achieve the treatment goals. The patient has a history of non-compliance with oral medications owing to paranoia that the drugs are poisonous. Thus, injectable psychotropics should be provided for the patient. During the visit, the patient should receive an initial intramuscular injection of Paliperidone, 234mg (Edinoff et al., 2021). The dosage should be followed by the same medication, 156 mg on the eighth day, and subsequent doses of 117mg monthly. The patient had no problem with Seroquel. Thus, 25 mg at bedtime will be administered to aid sleep.(Comprehensive Focused Soap Note for Schizophrenia Spectrum Other Psychotic and Medication-Induced Movement Disorders)
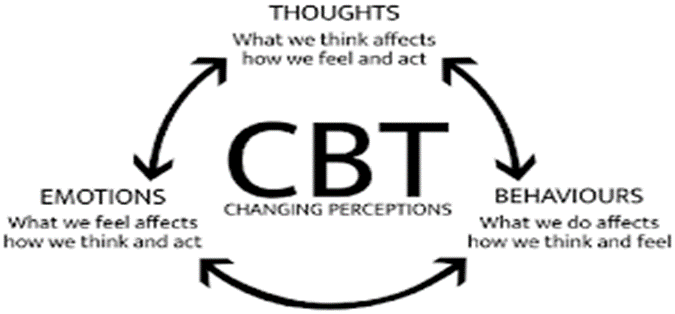
Subsequently, the psychotherapy approach-cognitive behavioral therapy will effectively manage the patient’s thoughts and behavioral symptoms. In a study to determine the efficacy of CBT in hallucination management in schizophrenic patients, CBT was reported to be effective in managing auditory hallucinations (Shukla et al., 2021). Notably, alternative therapies such as Yoga that incorporate mindfulness, meditation, and relaxation may improve the patient’s health.(Comprehensive Focused Soap Note for Schizophrenia Spectrum Other Psychotic and Medication-Induced Movement Disorders)
Moreover, the treatment strategy also aims to provide education to the patient. The patient will be educated on the significance of quitting cigarette and alcohol use. The patient will also be educated on the importance of complying with the treatment strategy by attending all sessions while reporting arising health concerns. The patient will also be educated on healthy living through regular exercise and taking a balanced diet to manage his diabetes condition (Mustapa et al., 2022). He will also be advised to join support groups to prevent social isolation and potential depressive symptoms. ST will also be referred to therapists. The patient will attend follow-up treatment after one week.(Comprehensive Focused Soap Note for Schizophrenia Spectrum Other Psychotic and Medication-Induced Movement Disorders)
Reflection
I would conduct the assessment differently if I had to re-do the case. I would order laboratory diagnostic tests such as drug screening, CBC, serology tests, Vitamin B12 levels, and complete metabolic panel to rule out health conditions that mimic psychiatric conditions and symptoms. I would also order a CT scan and MRI to rule out potential structural abnormalities. I would establish rapport and trust with the patient to foster a therapeutic alliance with the patient (Butt, 2021). In this case, I would affirm the patient’s experiences and gently challenge the hallucinations to make him understand how his symptoms are linked with Schizophrenia. I would offer psycho-education about the patient’s condition, causes, management options, and outcomes to improve his understanding.(Comprehensive Focused Soap Note for Schizophrenia Spectrum Other Psychotic and Medication-Induced Movement Disorders)
I will also respect ethical and legal concerns by respecting the patient’s autonomy while creating the treatment. I will only use involuntary treatment when protecting the patient from adverse events such as self-harm idealizations. I will balance autonomy with the need to address the patient’s symptoms while respecting set guidelines within my practice. I will also offer health promotion to assist the patient with a smoking problem that could lead to complications due to his diabetes diagnosis. Providing psychological and emotional support during counseling will effectively promote healthy behaviors. I will also use my cultural sensitivity knowledge to deliver culturally competent care to ensure that I create treatment plans that respect patient’s values and beliefs to promote compliance (Liu et al., 2022). I will also assess the patient’s socioeconomic variables, such as access and affordability to healthcare. I will determine whether the patient can afford transport for follow-up treatment. I can educate and help him obtain Medicare transport to promote compliance.(Comprehensive Focused Soap Note for Schizophrenia Spectrum Other Psychotic and Medication-Induced Movement Disorders)

References
American Psychiatric Association. (2022). Diagnostic and statistical manual of mental disorders, text revision DSM-5-TR. American Psychiatric Association.(Comprehensive Focused Soap Note for Schizophrenia Spectrum Other Psychotic and Medication-Induced Movement Disorders)
Butt M. F. (2021). Approaches to building rapport with patients. Clinical medicine (London, England), 21(6), e662–e663. https://doi.org/10.7861/clinmed.2021-0264
Edinoff, A. N., Doppalapudi, P. K., Orellana, C., Ochoa, C., Patti, S., Ghaffar, Y., Cornett, E. M., Kaye, A. J., Viswanath, O., Urits, I., Kaye, A. M., & Kaye, A. D. (2021). Paliperidone 3-Month Injection for Treatment of Schizophrenia: A Narrative Review. Frontiers in psychiatry, 12, 699748. (Comprehensive Focused Soap Note for Schizophrenia Spectrum Other Psychotic and Medication-Induced Movement Disorders)https://doi.org/10.3389/fpsyt.2021.699748
LaHue, S. C., & Douglas, V. C. (2022). Approach to Altered Mental Status and Inpatient Delirium. Neurologic clinics, 40(1), 45–57. https://doi.org/10.1016/j.ncl.2021.08.004
Liu, T. T., Chen, M. Y., Chang, Y. M., & Lin, M. H. (2022). A Preliminary Study on the Cultural Competence of Nurse Practitioners and Its Affecting Factors. Healthcare (Basel, Switzerland), 10(4), 678. (Comprehensive Focused Soap Note for Schizophrenia Spectrum Other Psychotic and Medication-Induced Movement Disorders)https://doi.org/10.3390/healthcare10040678
Maj, M., van Os, J., De Hert, M., Gaebel, W., Galderisi, S., Green, M. F., Guloksuz, S., Harvey, P. D., Jones, P. B., Malaspina, D., McGorry, P., Miettunen, J., Murray, R. M., Nuechterlein, K. H., Peralta, V., Thornicroft, G., van Winkel, R., & Ventura, J. (2021). The clinical characterization of the patient with primary psychosis is aimed at personalization of management. World psychiatry: official journal of the World Psychiatric Association (WPA), 20(1), 4–33(Comprehensive Focused Soap Note for Schizophrenia Spectrum Other Psychotic and Medication-Induced Movement Disorders). https://doi.org/10.1002/wps.20809
Mustapa, A., Justine, M., & Manaf, H. (2022). Effects of patient education on the quality of life of patients with type 2 diabetes mellitus: A scoping review. Malaysian Family Physician: The official journal of the Academy of Family Physicians of Malaysia, 17(3), 22–32(Comprehensive Focused Soap Note for Schizophrenia Spectrum Other Psychotic and Medication-Induced Movement Disorders). https://doi.org/10.51866/rv.208
Shukla, P., Padhi, D., Sengar, K. S., Singh, A., & Chaudhury, S. (2021). Efficacy and durability of cognitive behavior therapy in managing hallucination in patients with Schizophrenia. Industrial Psychiatry Journal, 30(2), 255–264(Comprehensive Focused Soap Note for Schizophrenia Spectrum Other Psychotic and Medication-Induced Movement Disorders). https://doi.org/10.4103/ipj.ipj_94_20
Wong, V., Chin, K., & Leontieva, L. (2022). Multifactorial Causes of Paranoid Schizophrenia With Auditory-Visual Hallucinations in a 31-Year-Old Male With History of Traumatic Brain Injury and Substance Abuse. Cureus, 14(5), e25488(Comprehensive Focused Soap Note for Schizophrenia Spectrum Other Psychotic and Medication-Induced Movement Disorders) https://doi.org/10.7759/cureus.25488

 Add Instructions
Add Instructions Online | Privacy policy
Online | Privacy policy