Culture of Excellence in Healthcare: A Guide for Nursing Students on Leading a Culture of Excellence to Foster Organizational Culture, Quality of Care, and Patient Experience
The culture of excellence in healthcare has become one of the most critical concepts shaping modern nursing practice. Excellence in healthcare refers to more than meeting minimum standards — it represents a sustained commitment to continuous improvement, professional growth, and the delivery of safe, compassionate, and high-quality care. For nursing students, understanding how to contribute to and lead a culture of excellence is not only essential for academic success but also for building the skills needed to thrive in professional practice.
In today’s complex healthcare system, patients, families, and communities expect more than just treatment; they seek holistic, patient-centered care that prioritizes safety, quality, and positive experiences. Nursing students, as future healthcare professionals, play a vital role in shaping this environment by learning how organizational culture, teamwork, and effective leadership strategies can transform care delivery. Developing awareness of the concept of a culture that prioritizes excellence empowers students to identify areas for improvement, engage in evidence-based practices, and contribute to better patient outcomes.
This article will guide you through the foundations of building and sustaining a culture of excellence. You will learn what defines excellence in healthcare, why it matters for nursing, and how it directly influences patient safety, satisfaction, and overall quality of care. It will also explore leadership qualities, communication strategies, and professional development practices that enable nurses to foster a culture of teamwork and accountability. Real-world examples and case studies will highlight successful models of organizational excellence, while practical tips will prepare you to apply these lessons in your clinical experiences.
Ultimately, as you progress through nursing education and transition into practice, your ability to create a culture of excellence will be central to improving patient outcomes, enhancing the patient experience, and advancing both your professional growth and the standards of care within the broader healthcare industry.
Understanding the Culture of Excellence
What is a Culture of Excellence in Healthcare?
A culture of excellence in healthcare is more than a slogan or mission statement—it is the organizational culture that guides how decisions are made, how patient care is delivered, and how staff interact with one another. At its core, it reflects a shared belief that every patient deserves the best care possible and that healthcare providers must continuously strive to achieve the highest standards.
This type of culture is built intentionally. Leaders set the tone by modeling behaviors that demonstrate a commitment to excellence and by creating structures that support accountability. It also relies on the healthcare team, where every member, from executives to nursing staff, contributes to a safe, respectful, and learning-oriented work environment.
Key characteristics include:
- Shared vision and values: Everyone understands and commits to the same goals—safety, compassion, and high-quality care.
- Focus on patient-centered care: Care delivery prioritizes respect, dignity, and individual needs.
- Continuous improvement: Staff are encouraged to identify areas for improvement and use evidence-based practices to strengthen systems.
- Professional development: Opportunities for training and development programs ensure staff grow alongside organizational goals.
- Open communication: Effective communication builds trust, reduces errors, and fosters teamwork across all disciplines.
Example: Consider a nursing unit where leadership implements structured bedside shift reports. By involving patients in the handoff process, the unit promotes transparency, teamwork, and better patient outcomes. This everyday practice reflects how an organization can create a culture of excellence that values both safety and patient engagement.
Why is a Culture of Excellence Important for Nursing?
For nursing students and future professionals, the culture within a healthcare organization profoundly shapes learning, growth, and practice. Entering a setting where excellence is prioritized provides several key benefits:
- Development of professional identity: Nursing students learn that excellence is not optional—it is the standard. By observing positive role models, they understand how professionalism, ethical practice, and evidence-based care fit into everyday work.
- Supportive work environment: A culture that values teamwork reduces stress, prevents burnout, and makes students feel part of the healthcare team, even during training. This kind of environment fosters resilience and prepares them for real-world challenges.
- Opportunities for leadership development: Students are encouraged to take part in projects that align with organizational goals, such as safety audits or quality improvement initiatives. These experiences give them a foundation for future nursing leadership roles.
- Alignment with standards of care: By practicing in organizations that prioritize excellence, nursing students become comfortable with policies, procedures, and best practices that meet or exceed standards of care.
Example: A student on clinical placement may be invited to participate in a hand hygiene compliance audit. Though simple, this activity introduces the student to quality improvement work, illustrates how small actions contribute to patient safety, and highlights their role in fostering an environment that prioritizes excellence.
How Does a Culture of Excellence Impact Patient Outcomes?
The link between culture and patient outcomes is direct and powerful. When a healthcare organization prioritizes excellence, the quality and safety of care improve, leading to better patient experiences and measurable health outcomes.
Impacts include:
- Improved patient safety: Open communication and nonpunitive reporting reduce risks, prevent repeated errors, and strengthen accountability.
- Enhanced quality of care: Evidence-based practices are consistently applied, reducing variation in care delivery.
- Positive patient experience: Patients feel respected, informed, and included in decisions, which improves trust in healthcare providers.
- Better patient outcomes: Fewer complications, lower rates of hospital-acquired conditions, and greater patient satisfaction are achieved when staff and leaders foster a culture of excellence.
Example: Imagine a surgical unit that adopts daily safety huddles where staff discuss risks, near misses, and patient priorities. Over time, this practice leads to fewer postoperative infections, greater confidence among nurses, and improved patient satisfaction scores. These measurable results show how organizational excellence directly translates into better patient outcomes.
Key Components of a Culture of Excellence
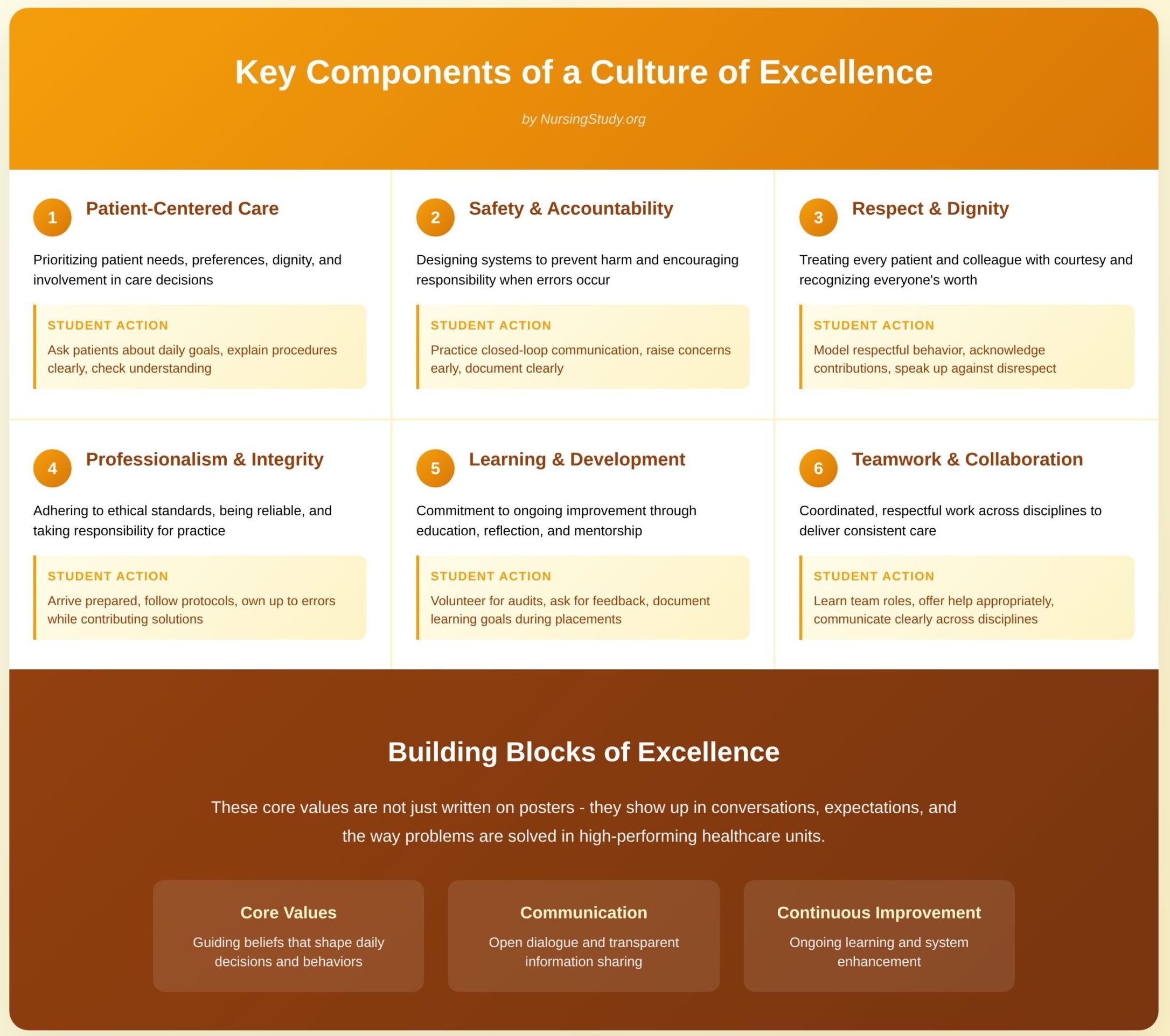
A culture of excellence is built from several interlocking components. Understanding these building blocks helps nursing students recognize strong practice environments and take concrete steps to contribute to them. The three foundational areas that follow — core values, communication, and continuous improvement — are where the culture is most visible and where students can have real impact.
What are the Core Values that Define Excellence in Healthcare?
Core values are the guiding beliefs and behaviors that shape day-to-day decisions. In units that consistently deliver high standards, these values are not just written on a poster — they show up in conversations, expectations, and the way problems are solved. Key values include:
- Patient-centered care
- Definition: Prioritizing the patient’s needs, preferences, dignity, and involvement in care decisions.
- How it shows up: Informed consent conversations, bedside handoffs that involve the patient, and personalized discharge teaching.
- Student action: Ask patients about their goals for the day, explain procedures in plain language, and check patient understanding before leaving the bedside.
- Safety and accountability
- Definition: Designing systems and behaviors that prevent harm and encourage staff to take responsibility when errors occur.
- How it shows up: Routine safety checks, open reporting of near misses, and leaders who investigate systems rather than blame individuals.
- Student action: Practice closed-loop communication (repeat-back), raise concerns early, and document observations clearly.
- Respect and dignity
- Definition: Treating every patient and colleague with courtesy and recognizing the worth of every team member.
- How it shows up: Inclusive language, protecting privacy, and valuing contributions from all staff levels.
- Student action: Model respectful behavior, acknowledge others’ contributions, and speak up if you observe disrespect.
- Professionalism and integrity
- Definition: Adhering to ethical standards, being reliable, and taking responsibility for one’s practice.
- How it shows up: Timely medication administration, thorough documentation, and transparent communication about mistakes.
- Student action: Arrive prepared, follow protocols, and own up to errors while contributing to solutions.
- Learning and development
- Definition: A commitment to ongoing improvement through education, reflection, and mentorship.
- How it shows up: Regular training, debriefs after critical events, and structured opportunities for career growth.
- Student action: Volunteer for audits, ask for feedback, and document learning goals during placements.
- Teamwork and collaboration
- Definition: Coordinated, respectful work across disciplines to deliver consistent care.
- How it shows up: Multidisciplinary rounds, shared care plans, and mutual support during busy shifts.
- Student action: Learn each team member’s role, offer help when appropriate, and communicate clearly across disciplines.
Concrete example: In a medical-surgical unit that values respect and learning, a student who notices a missed fall-risk reassessment is encouraged to report it; the team uses that information to redesign the reassessment trigger, reducing falls and reinforcing accountability without punishing the individual who missed it.
How Can Communication Foster a Culture of Excellence?
Communication is the glue that holds values and practice together. Clear, consistent, and respectful communication lowers risk, speeds up problem-solving, and builds trust among staff and patients.
Key communication practices and their impact
- Structured handoffs and reports
- Why they matter: Standardized formats reduce variability and prevent omissions during transitions of care.
- Student tip: Learn and use the unit’s handoff structure — practice concise, focused reporting and include patient priorities.
- Safety huddles and briefings
- Why they matter: Short, routine gatherings help teams identify risks for the shift and coordinate plans.
- Student tip: Attend huddles, listen for patterns, and volunteer to present one patient’s safety needs when appropriate.
- Closed-loop communication and read-backs
- Why they matter: Ensures instructions are heard, understood, and acted upon—critical for medication orders and urgent tasks.
- Student tip: Use read-backs for all verbal orders and show clear acceptance of responsibility.
- Nonpunitive feedback and debriefs
- Why they matter: When feedback is focused on system improvement rather than blame, staff are more willing to report errors and near misses.
- Student tip: When providing feedback, use “I noticed…”, describe the effect, and suggest a practical change.
- Patient and family communication
- Why it matters: Engaged patients often experience better outcomes and adhere more closely to care plans.
- Student tip: Use teach-back with patients after education and involve families in discharge planning.
Practical communication script (student-friendly):
- Situation: “Mrs. K is 72, post-op day 1 with rising pain scores and decreased urine output.”
- Background: “She had a laparotomy yesterday; IV fluids were decreased overnight.”
- Assessment: “Pain 8/10, urine output 15 mL/hr for last 2 hrs, tachycardic.”
- Recommendation: “I recommend we increase IV rate to X mL/hr, reassess in 30 minutes, and consider notifying the surgical team if no improvement.”
Using a concise structure like this helps the receiver understand the urgency and proposed next steps.
Why is Continuous Improvement Essential for Nursing Professionals?
Continuous improvement is the ongoing effort to make care safer, more efficient, and more patient-centered. It transforms isolated fixes into sustained gains and is essential at every career stage.
Why continuous improvement matters for nurses
- Makes care more reliable
- Small, tested changes reduce variation and create predictable, safer processes.
- Empowers frontline staff
- Nurses who participate in improvement work can change processes that directly affect their daily practice and patient outcomes.
- Supports professional growth
- Improvement projects develop skills in data interpretation, communication, project management, and leadership — all core to career advancement.
- Sustains measurable gains
- By measuring before and after interventions, teams can show real benefit and build momentum for broader change.
Simple improvement method (student-friendly version)
- Identify a problem — pick something you observe frequently (e.g., patient education at discharge is inconsistent).
- Measure baseline — collect a small sample for a week to see the current rate (e.g., % of patients with documented teach-back).
- Plan a small change — test one change (e.g., add a 5-minute teach-back checklist at discharge).
- Do the test — run the change for one week on one ward or during a single shift.
- Study results — compare the new data with baseline and gather staff feedback.
- Act — adopt, adapt, or abandon the change based on results; if successful, scale up and standardize.
Example micro-project: Reduce missed patient education at discharge
- Baseline: 40% documented teach-back.
- Intervention: Implement a two-item checklist on the nurse’s shift report and label discharge charts.
- Result: After two PDSA cycles, documented teach-back increases to 75%.
- Student role: Collect baseline data, run the checklist on your shift, and present results at the next unit meeting.
Building Your Leadership Skills
Developing leadership skills is not only for senior nurses — nursing students can and should begin cultivating leadership qualities early in their training. Leadership is central to sustaining a culture of excellence in healthcare, because leaders set expectations, model values, and influence how teams respond to challenges. Even without a formal title, students can demonstrate leadership by embodying qualities that inspire trust, promote teamwork, and enhance quality of care.
What Leadership Qualities Contribute to a Culture of Excellence?
Leadership qualities are the behaviors and attitudes that guide how individuals influence others. In healthcare settings, several qualities stand out as especially critical to building a culture of excellence:
- Vision and purpose
- Leaders articulate a clear direction that aligns with patient-centered goals.
- Example: A charge nurse sets the expectation that every patient will be updated about their care plan by midday, ensuring transparency and trust.
- Student application: Define small but clear goals during clinical rotations, such as ensuring every patient you care for understands one key element of their treatment before the end of your shift.
- Accountability
- Strong leaders own both successes and mistakes, modeling responsibility.
- Example: A nurse leader admits to missing a protocol step, discusses it openly, and introduces a strategy to prevent recurrence.
- Student application: If you make an error in documentation, acknowledge it immediately, correct it, and share what you learned.
- Integrity and ethical grounding
- Leaders act consistently with ethical standards, building credibility and trust.
- Example: Advocating for a patient’s pain management even when pressured to discharge quickly.
- Student application: Speak up when you notice care that could compromise safety or dignity, even if it feels uncomfortable.
- Adaptability
- Healthcare is unpredictable, and leaders must stay composed under pressure.
- Example: A team leader reorganizes assignments rapidly when several new admissions arrive simultaneously.
- Student application: Be flexible with new tasks, and show willingness to learn new skills quickly.
- Collaboration and inclusiveness
- Leaders value all perspectives and foster teamwork.
- Example: Including nursing assistants in safety planning meetings to capture their insights.
- Student application: Ask other team members for their observations before making decisions about patient priorities.
- Communication
- Effective leaders ensure information flows smoothly across disciplines and to patients.
- Example: Using structured briefings so all team members understand patient needs.
- Student application: Practice SBAR (Situation, Background, Assessment, Recommendation) during reports, even in student roles.
How Can Nursing Students Develop Effective Leadership Skills?
Leadership development is a continuous process that begins with self-awareness and small actions in everyday practice. Nursing students can start building leadership by focusing on the following strategies:
- Engage actively in clinical learning
- Take initiative by asking questions, volunteering for new experiences, and reflecting on patient outcomes.
- Example: If there’s a code simulation, volunteer to play a role, even if it feels challenging.
- Seek mentorship and role models
- Observing effective nurse leaders provides practical insights into decision-making and conflict resolution.
- Example: Ask your preceptor to explain how they prioritize tasks during a high-acuity shift.
- Practice self-reflection
- Journaling about clinical experiences helps identify strengths and areas for improvement.
- Example: After a shift, write down one moment where you showed leadership (e.g., organizing patient education) and one where you could improve.
- Develop clinical confidence
- Competence in skills builds credibility; others are more likely to follow your lead when you are reliable.
- Example: Master basic procedures like vital signs or IV monitoring, then gradually take responsibility for more complex tasks.
- Embrace small leadership opportunities
- Even as a student, you can lead by example.
- Example: Taking charge of ensuring all supplies are ready for wound care rounds, then briefing the team.
- Learn conflict management
- Disagreements are inevitable, and how they are handled affects the team climate.
- Example: If two team members disagree about task delegation, suggest focusing on patient needs as the common goal.
- Build interprofessional respect
- Leadership is not limited to nursing teams — it extends to collaboration with physicians, therapists, and families.
- Example: Thank a physical therapist for updates and incorporate them into your patient care plan, showing respect for shared expertise.
Student takeaway: Leadership is not about authority — it’s about influence. By consistently showing initiative, accountability, and respect, nursing students can already model the values of a culture of excellence.
What Role Does Emotional Intelligence Play in Nursing Leadership?
Emotional intelligence (EI) — the ability to recognize, understand, and manage one’s own emotions while responding effectively to others — is a cornerstone of leadership in nursing. In high-stress healthcare environments, EI determines whether leaders can maintain trust, foster collaboration, and ensure patient safety.
Key dimensions of EI in nursing leadership:
- Self-awareness
- Understanding personal stress responses and triggers.
- Example: Recognizing that you become rushed when fatigued, and planning short breaks to stay calm during busy shifts.
- Self-regulation
- Controlling emotions to remain steady under pressure.
- Example: In a code situation, a leader speaks calmly, giving clear instructions despite chaos.
- Student practice: When overwhelmed, take a breath before responding and focus on facts rather than emotions.
- Motivation
- Staying focused on goals even during setbacks.
- Example: Encouraging a team to meet fall-prevention targets despite staffing shortages.
- Student practice: Set small daily goals for patient education or communication, and celebrate progress.
- Empathy
- Understanding the feelings of patients, families, and colleagues.
- Example: A nurse leader acknowledges a family’s anxiety about a procedure and ensures extra time for questions.
- Student practice: When a patient seems resistant, ask about their concerns before offering solutions.
- Social skills
- Building relationships, resolving conflicts, and fostering teamwork.
- Example: A leader notices tension between nurses and physicians and facilitates a shared problem-solving meeting.
- Student practice: Express gratitude to team members after collaborative efforts; small acknowledgments strengthen relationships.
Why EI matters in the culture of excellence
- It reduces conflict and improves team morale.
- It builds trust, which increases patient confidence in care delivery.
- It supports resilience by helping leaders cope with stress while modeling calm for their teams.
Concrete student example: During clinicals, a peer may be struggling with a skill. Instead of criticizing, a student with strong EI offers encouragement, helps break the task into steps, and validates the peer’s effort. This small act fosters collaboration and models leadership through empathy.
Strategies for Promoting a Culture of Excellence
Promoting a culture of excellence in healthcare requires intentional strategies that involve everyone, from executives to nursing students. While leadership sets the tone, individuals at every level play an important role in sustaining an organizational culture that values quality, safety, and patient-centered care. For nursing students, this means learning to advocate for high standards, encouraging teamwork, and using feedback constructively to identify opportunities for improvement.
How Can Nursing Students Advocate for Excellence in Their Clinical Settings?
Nursing students may feel limited in authority, but advocacy is not about titles — it’s about actions that demonstrate a commitment to excellence. Advocacy in clinical settings means standing up for patients, promoting evidence-based practices, and modeling professionalism.
Ways students can advocate include:
- Prioritizing patient-centered care
- Example: If a patient seems confused about medication, a student can respectfully remind the nurse preceptor to provide clear explanations. This small action helps ensure patients feel included in their care.
- Promoting patient safety
- Example: If a student notices a hand hygiene lapse, they can politely ask, “Would you like me to grab sanitizer for us before we start?” This approach advocates for patient safety without confrontation.
- Demonstrating accountability
- When errors or near misses occur, students should acknowledge them and learn from the process. Owning mistakes demonstrates integrity and fosters a culture that prioritizes safety and learning.
- Engaging in continuous learning
- Students can ask to participate in safety briefings, audits, or quality improvement projects during clinical rotations. This demonstrates initiative and highlights their interest in improving patient outcomes.
- Modeling respect and compassion
- Advocacy is not only about policies — it’s also about behaviors. By treating patients with dignity and maintaining professionalism with the healthcare team, students promote standards of excellence.
What Strategies Can Be Implemented to Encourage Team Collaboration?
A culture of excellence cannot exist without effective teamwork. Nursing students often join diverse healthcare teams, and how they interact influences the work environment and patient experience. Collaboration strategies benefit both staff and patients by reducing miscommunication and building trust.
Key strategies include:
- Structured communication
- Using frameworks like SBAR during handoffs ensures information is accurate and clear.
- Example: A student presenting a patient case to a nurse uses SBAR, which saves time and reduces errors.
- Interdisciplinary respect
- Recognizing the expertise of all healthcare providers fosters trust.
- Example: When a respiratory therapist provides recommendations, the student incorporates them into care notes, showing respect for shared knowledge.
- Shared decision-making
- Collaborative discussions ensure patient needs are prioritized over individual preferences.
- Example: During rounds, a student suggests including the patient’s expressed concerns in the plan, modeling inclusiveness.
- Active listening and support
- Team members feel valued when their perspectives are heard.
- Example: A student listens to a nursing assistant’s observation about a patient’s mobility before reporting it to the nurse.
- Celebrating small wins
- Acknowledging achievements reinforces positive behaviors.
- Example: Thanking peers after a successful procedure fosters morale and encourages repeat collaboration.
How Can Feedback Mechanisms Improve the Culture of Excellence?
Feedback is one of the most powerful tools for continuous improvement in healthcare. A strong feedback culture ensures that learning is ongoing, mistakes are addressed constructively, and patient outcomes continually improve.
For nursing students, feedback mechanisms serve three essential purposes:
- Improving clinical skills
- Constructive feedback from preceptors highlights areas where students can enhance their practice.
- Example: A preceptor points out that a student’s documentation lacked detail; the student adjusts immediately, strengthening the quality of patient care.
- Enhancing teamwork
- Feedback between peers fosters mutual respect and collective learning.
- Example: Two students working together reflect on each other’s communication style, improving collaboration for the next shift.
- Strengthening accountability
- Open feedback ensures staff and students remain aligned with organizational standards.
- Example: A student receives feedback on time management and uses it to better prioritize patient needs during clinical hours.
Best practices for feedback in a culture of excellence:
- Make it timely: Feedback should be given soon after the event to remain relevant.
- Keep it specific: Focus on observable behaviors, not personality traits.
- Ensure it’s balanced: Highlight strengths alongside areas for improvement.
- Encourage two-way dialogue: Students can also ask for feedback on how to improve patient interactions or teamwork.
Example: A student practicing IV insertion receives immediate feedback: “You maintained good aseptic technique, but next time ensure your explanation to the patient is clearer.” This balanced feedback builds confidence while encouraging growth.
Challenges to Building a Culture of Excellence
While the idea of a culture of excellence in healthcare sounds straightforward, creating and sustaining it is not without challenges. Many healthcare organizations face barriers that prevent consistent delivery of high-quality care, and these challenges can affect both staff and patients. For nursing students, understanding these barriers provides insight into the complexities of the healthcare system and equips them with strategies to contribute positively despite obstacles.
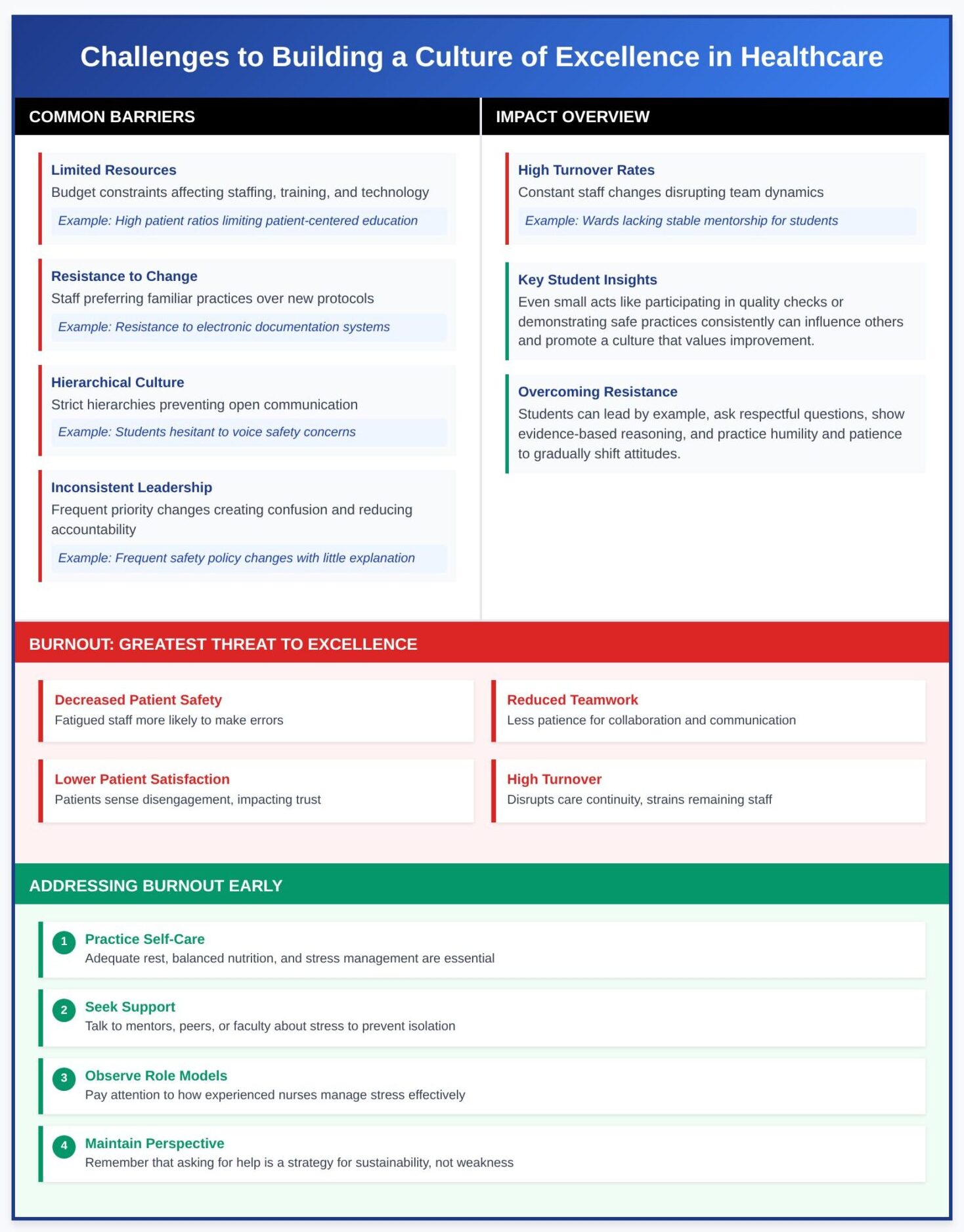
What Common Barriers Exist in Healthcare Settings?
- Limited resources
- Budget constraints often limit staffing, training, and technology. This can affect the quality of patient care and place pressure on nurses to manage more patients than is ideal.
- Example: A unit with high patient ratios may struggle to provide patient-centered education, impacting the patient experience.
- Resistance to change
- Staff may prefer familiar practices over adopting new best practices or evidence-based protocols.
- Example: A nurse may resist implementing electronic documentation systems, preferring paper charts, which creates inconsistencies in care delivery.
- Hierarchical culture within healthcare teams
- Strict hierarchies can prevent open communication, where students or junior staff feel unable to speak up about safety concerns.
- Example: A student notices a missed allergy notation but hesitates to speak up due to fear of challenging a senior nurse.
- Inconsistent leadership
- Without effective leadership strategies, priorities may shift frequently, creating confusion and reducing accountability.
- Example: Frequent changes in safety policies with little explanation can erode trust among the healthcare team.
- High turnover rates
- Constant staff changes disrupt team dynamics and impact the ability to foster a culture of excellence.
- Example: A ward experiencing high turnover may lack stable mentorship, leaving students without role models for nursing practice.
How Can Nursing Students Overcome Resistance to Change?
Even though nursing students may not have authority to enforce change, they can play a role in gradually shifting attitudes.
- Lead by example
- Students can demonstrate openness to new methods, such as adopting digital tools or applying updated protocols.
- Example: During clinical rotations, a student embraces electronic health record systems quickly, showing peers that adaptability improves efficiency.
- Ask questions respectfully
- Students can encourage reflection by asking preceptors or team members to explain why a process is done a certain way. This approach avoids confrontation while opening the door to considering opportunities for improvement.
- Show evidence-based reasoning
- If students are taught new evidence-based practices in class, they can share insights in a collaborative tone.
- Example: A student may say, “I learned in lecture that repositioning patients every two hours reduces pressure injuries—would it be okay if I help with this today?”
- Practice humility and patience
- Change takes time, and students should remain respectful, understanding that resistance often stems from fear of added workload or uncertainty.
Student insight: Even small acts — like asking to participate in quality checks or demonstrating safe practices consistently — can influence others and promote a culture that values improvement.
What Role Does Burnout Play in Diminishing a Culture of Excellence?
Burnout is one of the greatest threats to organizational excellence in healthcare. It occurs when healthcare professionals experience emotional exhaustion, depersonalization, and a reduced sense of accomplishment due to chronic stress.
How burnout undermines excellence:
- Decreased patient safety: Fatigued staff are more likely to make errors, compromising safety.
- Reduced teamwork: Overstretched staff may have less patience for collaboration or open communication.
- Lower patient satisfaction: Patients can sense when staff are disengaged, which impacts trust and care experiences.
- High turnover: Burnout leads to resignations, disrupting continuity of care and straining remaining staff.
Example: A nurse working consistent overtime may struggle to maintain compassion in interactions, resulting in rushed explanations and a negative patient experience. This demonstrates how burnout directly impacts the quality of care provided.
How students can address burnout early:
- Practice self-care: Adequate rest, balanced nutrition, and stress management are essential.
- Seek support: Talking to mentors, peers, or faculty about stress helps prevent isolation.
- Observe role models: Pay attention to how experienced nurses manage stress and workload effectively.
- Maintain perspective: Remind yourself that asking for help is not a weakness but a strategy for sustainability.
Student takeaway: By recognizing burnout in themselves and others, nursing students can learn to prioritize well-being, advocate for manageable workloads, and contribute to a work environment where staff resilience supports consistent excellence.
Real-World Examples and Case Studies
Learning about the culture of excellence in healthcare becomes most meaningful when examined through real-world models and case studies. These examples show how healthcare organizations apply leadership strategies, teamwork, and continuous improvement to transform care delivery and enhance the patient experience. For nursing students, analyzing such cases provides concrete lessons on how to apply the principles of excellence in both training and future practice.
What Are Some Successful Models of a Culture of Excellence in Healthcare?
A culture of excellence in healthcare is not theoretical—it is demonstrated through established models that reshape the organization’s culture, improve safety, and enhance the patient experience. These models provide tangible pathways for nursing students to understand how leadership, teamwork, and evidence-based strategies drive meaningful change.
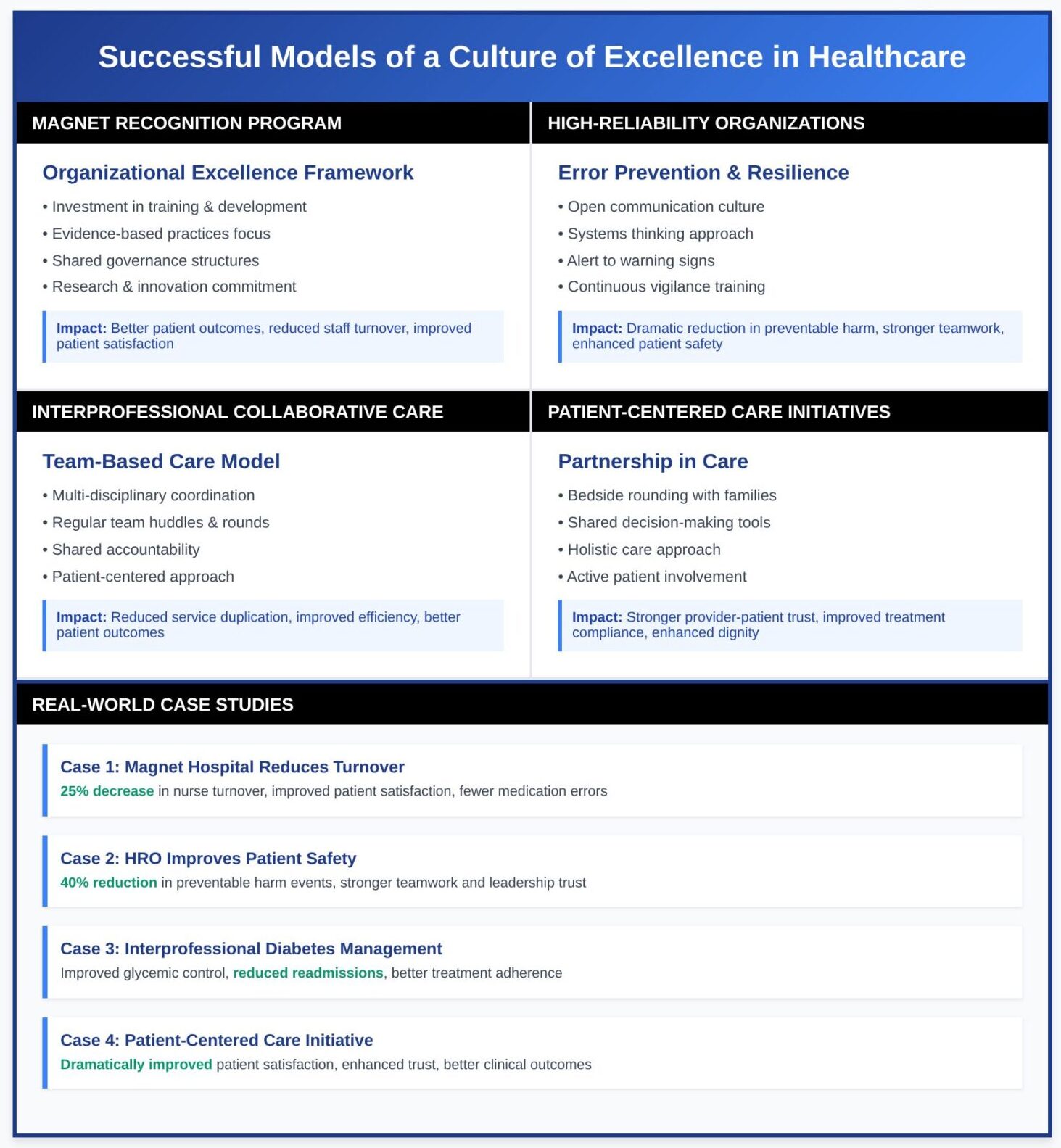
Magnet Recognition Program
The Magnet Recognition Program is one of the most widely respected frameworks for demonstrating organizational excellence in nursing. Achieving Magnet status requires hospitals to meet rigorous standards related to professional development, standards of care, and quality improvement.
- Core Features:
- Investment in training and development to empower nurses at all levels.
- Strong focus on evidence-based practices to ensure the best care is delivered consistently.
- Shared governance structures where nurses participate in decision-making, ensuring their voices shape the organization’s goals.
- Commitment to research and innovation in nursing practice.
- Impact on Healthcare Delivery:
- Magnet-recognized facilities consistently report better patient outcomes, such as lower rates of hospital-acquired infections and readmissions.
- Staff turnover decreases as nurses feel valued and engaged, reducing burnout.
- Patients experience higher trust in their providers, contributing to improved patient satisfaction.
- Student Takeaway: For nursing students, Magnet hospitals demonstrate how a structured approach to leadership development, continuous learning, and teamwork directly translates to excellence in patient care. Observing these models in practice highlights how leaders set the tone for quality and safety across an organization.
- High-Reliability Organizations (HROs) Borrowed from industries like aviation and nuclear power, high-reliability organizations emphasize error prevention and resilience in complex, high-risk environments. Applying these principles in the healthcare industry is vital given the complexity of modern care delivery.
- Core Features:
- A strong culture of open communication, where all staff feel safe to report errors without fear of punishment.
- Relentless attention to detail and systems thinking to anticipate and prevent risks.
- Leaders and staff are trained to remain alert to small warning signs, reducing the likelihood of catastrophic failures.
- Impact on Patient Safety:
- Hospitals implementing HRO principles have seen dramatic reductions in wrong-site surgeries, medication errors, and other preventable harm.
- Interdisciplinary accountability improves collaboration and strengthens the healthcare team.
- Patient safety becomes the foundation of every clinical decision.
- Student Takeaway: Nursing students in HRO-focused hospitals learn how every action, from medication checks to hand hygiene, ties into larger systems of accountability. This approach teaches them that quality and safety are not abstract values but daily practices that safeguard patients and improve trust in the healthcare system.
- Core Features:
Interprofessional Collaborative Care Models
Modern healthcare services require multiple disciplines to work together to address the diverse needs of patients. Interprofessional models of care exemplify how collaboration creates better outcomes and a more efficient system.
- Core Features:
- Physicians, nurses, pharmacists, therapists, and social workers coordinate care around the patient rather than working in silos.
- Regular team huddles and rounds ensure alignment on treatment goals and progress.
- Shared accountability ensures each professional is responsible for the quality of patient care provided.
- Impact on Care Delivery:
- Reduces duplication of services and prevents conflicting treatment plans.
- Improves efficiency while maintaining high-quality care standards.
- Example: In managing complex diabetes, coordinated care between nurses, dietitians, and pharmacists results in improved blood sugar control, fewer hospital visits, and better patient outcomes.
- Student Takeaway: For nursing students, these models demonstrate the importance of mutual respect and communication across disciplines. Observing team-based care helps students learn how to foster a culture of excellence by valuing diverse perspectives and prioritizing patient-centered goals.
Patient-Centered Care Initiatives
At the heart of a commitment to excellence is patient-centeredness—the belief that patients should be active partners in their care. Hospitals adopting patient-centered initiatives demonstrate how involving patients transforms the patient experience.
- Core Features:
- Bedside rounding, where patients and families are included in daily discussions about treatment.
- Shared decision-making tools to ensure care aligns with patient values and preferences.
- Emphasis on treating patients holistically, addressing not only physical health but also emotional and social needs.
- Impact on Quality and Satisfaction:
- Builds stronger trust between healthcare providers and patients.
- Enhances compliance with treatment plans, as patients feel respected and involved.
- Reduces anxiety, improves dignity, and fosters long-term relationships with the healthcare system.
- Student Takeaway: Nursing students witness how patient-centered care drives both compassion and measurable results. By observing these initiatives, they learn that true excellence is not only about clinical outcomes but also about the patient’s perception of care and their overall well-being.
How Can Nursing Students Learn from Real-World Case Studies?
Real-world case studies provide nursing students with concrete examples of how a culture of excellence in healthcare is implemented, the challenges faced, and the measurable results achieved. By analyzing these situations, students can bridge the gap between theory and practice, preparing themselves to contribute meaningfully to a healthcare organization’s success.
Case Study 1: Magnet-Recognized Hospital Reduces Nurse Turnover
A large urban hospital that achieved Magnet Recognition noticed persistently high nurse turnover rates, leading to staffing shortages and decreased morale. Leadership responded by investing in professional development programs, creating shared governance councils, and promoting a culture that prioritizes open communication.
- Outcome: Within two years, nurse turnover decreased by 25%, and patient satisfaction scores improved significantly. The hospital also reported measurable improvements in the quality of patient care, including fewer medication errors and higher compliance with evidence-based practices.
- Student Learning: Nursing students observing this case see the direct link between leadership strategies, professional support, and better patient outcomes. They learn that effective nursing leadership not only improves staff well-being but also enhances the care provided to patients.
Case Study 2: High-Reliability Organization Improves Patient Safety
A regional healthcare system adopted the principles of high-reliability organizations (HROs) after experiencing a rise in preventable adverse events. Leaders implemented nonpunitive reporting systems, emphasized continuous learning, and trained staff to identify areas for improvement through daily safety huddles.
- Outcome: Over three years, the hospital saw a 40% reduction in preventable harm events, such as wrong-site surgeries and central line infections. Staff reported stronger teamwork and trust in leadership, and patients consistently rated safety as a strength in satisfaction surveys.
- Student Learning: Nursing students exposed to this environment understand how a strong commitment to excellence and a leadership style that empowers staff directly improves patient safety. They learn that promoting transparency and vigilance in their future practice will help them foster a culture of excellence.
Case Study 3: Interprofessional Team Improves Diabetes Management
In a mid-sized community hospital, a patient population with uncontrolled diabetes was experiencing frequent emergency room visits and poor health outcomes. The hospital formed an interprofessional collaborative care model that included nurses, dietitians, physicians, and pharmacists.
- Outcome: Within one year, patients showed improved glycemic control, reduced hospital readmissions, and better adherence to treatment plans. The hospital also reported increased patient satisfaction, as individuals felt more supported by a coordinated healthcare team.
- Student Learning: For nursing students, this case demonstrates the value of teamwork and the importance of respecting contributions from multiple professionals. It highlights how effective leadership and interprofessional collaboration not only improve patient outcomes but also create a supportive work environment.
Case Study 4: Patient-Centered Care Initiative Improves Patient Experience
A teaching hospital launched a patient-centered care initiative by implementing bedside shift reporting and involving patients in daily rounds. Nurses and healthcare providers were trained to practice active listening and engage patients in setting care goals.
- Outcome: Patient satisfaction scores rose dramatically, with patients reporting greater trust and reduced anxiety. Clinical outcomes also improved, as patients adhered more consistently to treatment plans due to shared decision-making.
- Student Learning: Nursing students in this setting see firsthand how patient-centered care is not just a philosophy but a practical tool for enhancing patient outcomes. They learn that involving patients directly in care decisions fosters dignity, strengthens trust, and improves both safety and quality of care.
What Lessons Can Be Applied to Your Future Practice?
The real test of studying a culture of excellence in healthcare is not only understanding its principles but also applying them in daily nursing practice. For nursing students preparing to transition into professional roles, the lessons from successful models and case studies provide a roadmap for how to contribute meaningfully to organizational excellence and improved patient outcomes.
1. Prioritize Patient-Centered Care
One of the strongest lessons is the importance of keeping the patient at the center of all decisions. By practicing patient-centered care, nurses ensure that treatments, communication, and planning reflect the patient’s needs, values, and preferences. In future practice, this means actively involving patients in decision-making, listening carefully to their concerns, and recognizing that respect and empathy are as essential as technical skills.
- Practical Application: A new nurse can incorporate bedside rounding by explaining treatment plans directly to patients and their families, encouraging questions, and ensuring they feel included. This fosters dignity and strengthens trust between patients and healthcare providers.
2. Commit to Continuous Improvement
Excellence requires more than maintaining standards—it involves continuous improvement and regularly identifying opportunities for growth. Nursing students entering the workforce must embrace the mindset of ongoing learning, whether through evidence-based practices, quality initiatives, or participating in improvement projects within their units.
- Practical Application: A future nurse may join a unit-based council focused on reducing falls or medication errors, helping to improve quality and enhance patient safety. By engaging in such projects, nurses actively contribute to better patient outcomes and a stronger organization’s culture.
3. Develop Strong Leadership Qualities
Even as new graduates, nurses play a leadership role in shaping the culture within their workplace. Lessons from case studies show that effective leadership is not limited to formal titles—it involves setting the tone through accountability, teamwork, and professionalism. A leadership style that values collaboration and respect for colleagues promotes both quality care and a healthy work environment.
- Practical Application: A nurse who models open communication, advocates for safe staffing, or mentors peers demonstrates a commitment to excellence and inspires others to do the same.
4. Embrace Teamwork and Interprofessional Collaboration
Successful healthcare delivery depends on a cohesive healthcare team where each professional’s expertise is valued. Lessons from collaborative care models show that teamwork reduces errors, improves coordination, and leads to enhancing patient outcomes.
- Practical Application: Future nurses can participate actively in interdisciplinary rounds, ensuring that the nurse’s perspective is represented in planning care. By doing so, they foster a culture of excellence where shared responsibility improves both safety and efficiency.
5. Guard Against Burnout and Promote Well-Being
Case studies highlight that burnout undermines excellence by reducing motivation, increasing turnover, and weakening the organization’s performance. Future nurses must learn to balance their workload, seek support when needed, and participate in wellness and development programs that strengthen resilience.
- Practical Application: New nurses can practice self-care, advocate for fair workloads, and support peers experiencing stress. By maintaining their well-being, they ensure they can consistently deliver high-quality care to patients.
6. Use Feedback as a Tool for Growth
Feedback, when approached constructively, drives continuous learning and personal development. Lessons from real-world models show that hospitals using structured feedback mechanisms experience stronger engagement and measurable improvements in care.
- Practical Application: A future nurse can invite feedback from preceptors or colleagues during clinical practice, using it to refine skills, strengthen communication, and enhance the quality of patient care delivered.
7. Demonstrate a Commitment to Excellence Daily
Finally, the most enduring lesson is that excellence requires consistent action. Whether through small decisions—such as double-checking a medication—or larger initiatives, like leading a quality improvement project, each act reflects a nurse’s dedication to maintaining high standards of care delivery.
- Practical Application: Nursing students transitioning into their careers can set personal goals to practice evidence-based care, communicate openly with their teams, and uphold the highest standards of care, thereby demonstrating a genuine commitment to excellence.
Conclusion
A culture of excellence in healthcare does not emerge by chance. It is built intentionally through leadership, collaboration, and a shared commitment to excellence across every level of a healthcare organization. For nursing students, the journey toward becoming professionals is not just about acquiring clinical knowledge—it is also about understanding how to create a culture of excellence that transforms both the work environment and the care provided to patients.
Throughout this article, we have seen that the concept of a culture in healthcare is rooted in values such as accountability, respect, and continuous learning. By studying real-world models like Magnet hospitals, high-reliability organizations, interprofessional care, and patient-centered initiatives, nursing students learn that excellence requires more than skill—it requires leadership, resilience, and the ability to engage others in a shared vision of quality and safety.
As you prepare to enter the healthcare industry, remember that nursing practice is more than a set of tasks; it is about consistently delivering high-quality and patient-centered care while contributing to your organization’s culture. Whether you are advocating for safer staffing, engaging in quality improvement projects, or simply listening carefully to a patient’s concerns, you are shaping the standards of care that define the future of healthcare delivery.
You will also face challenges—such as burnout, resistance to change, and competing demands—but these are opportunities to demonstrate resilience and to lead by example. By applying the lessons of effective leadership, teamwork, and continuous improvement, you can help identify areas for improvement, inspire colleagues, and foster a culture of excellence that prioritizes the well-being of patients and staff alike.
Ultimately, your role as a future nurse is not just to adapt to the organization’s expectations but to set the tone for excellence within your environment. By demonstrating a commitment to professional growth, embracing evidence-based practices, and promoting open communication, you will strengthen the quality of patient care and help achieve better patient outcomes.
Excellence in healthcare refers to more than standards—it is about cultivating a mindset that seeks to improve, to learn, and to serve with integrity. As you step into your career, remember that leaders set the tone, but every nurse contributes to sustaining excellence. Your actions, both big and small, can transform a team, enhance the patient experience, and leave a lasting impact on the healthcare system.
Frequently Asked Questions
What is the culture of excellence?
The culture of excellence is an organizational mindset and environment where high standards, continuous improvement, and a strong commitment to quality are prioritized in every action. It emphasizes accountability, teamwork, and delivering the best outcomes consistently.
What are the characteristics of the culture of excellence in healthcare?
Key characteristics include patient-centered care, teamwork, evidence-based practices, open communication, strong leadership, commitment to patient safety, continuous learning, and a focus on improving both patient outcomes and staff well-being.
What is an example of excellence in healthcare?
An example is a Magnet-recognized hospital that invests in nursing leadership, professional development, and quality improvement initiatives. Such hospitals often report lower nurse turnover, higher patient satisfaction, and measurable improvements in patient safety.
What is the culture of excellence theory?
The culture of excellence theory explains how values, behaviors, and leadership strategies within an organization shape its ability to consistently achieve high standards. It highlights how organizational culture, continuous improvement, and commitment from leaders and staff foster sustainable excellence.
