CNA vs PCT: Which Healthcare Career — Certified Nursing Assistant, Patient Care Technician, or Medical Assistant?
Understanding the distinctions between frontline caregiving roles is essential for students preparing to enter the healthcare environment. Although these roles often appear similar from a distance, they differ significantly in training expectations, clinical responsibilities, and the level of patient support they provide. These differences influence not only day-to-day tasks but also how individuals collaborate with nurses, physicians, and other members of the care team.
Across hospitals, rehabilitation centers, and long-term care environments, unlicensed assistive personnel play a crucial role in maintaining patient comfort, monitoring clinical changes, and supporting safe, effective care delivery. Their work forms a bridge between licensed nursing staff and the fundamental needs of patients—needs that range from mobility assistance and monitoring to essential daily care activities. Appreciating the nuances between these positions helps future clinicians understand how care teams function and how responsibilities are distributed within structured clinical hierarchies.
These roles also serve as common entry points into the broader healthcare field, making them especially relevant to students who envision long-term careers in nursing or allied health professions. Exploring the differences in training pathways, clinical skills, and work environments offers valuable insight into how each role contributes to the patient experience and how they can shape early professional development.
This guide provides a clear, comprehensive examination of how these positions compare. It outlines variations in training, clinical duties, workplace expectations, and growth opportunities, offering a grounded perspective for students evaluating their first steps into the healthcare workforce. By examining responsibilities across clinical settings and understanding how these support roles interface with licensed nurses, readers can develop a more informed view of patient care teams and the foundational skills required to thrive within them.
What is the difference between a CNA and a PCT (pct vs cna)?
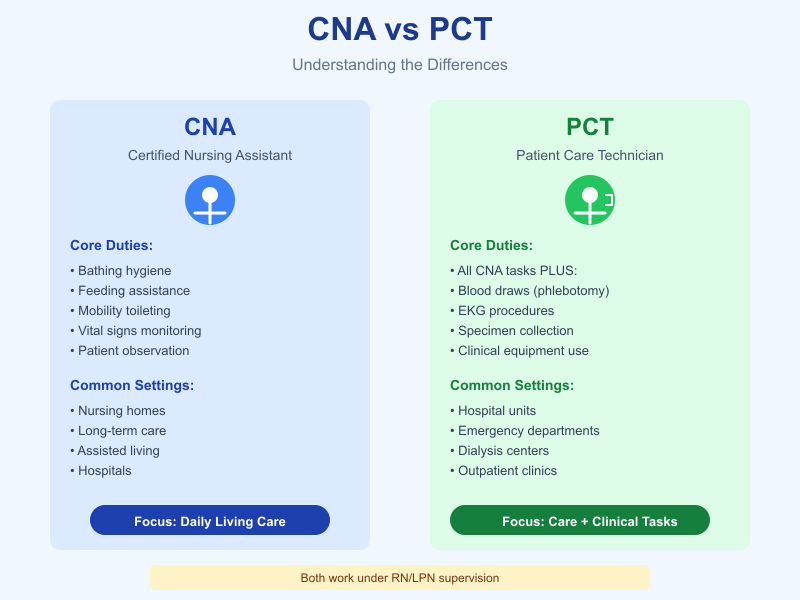
Certified nursing assistants and patient care technicians occupy overlapping but distinguishable roles on the bedside care team. At a basic level, a CNA (certified nursing assistant) is trained and certified to provide foundational nursing care such as hygiene, mobility assistance, feeding, toileting and basic monitoring. A PCT (patient care technician or patient care tech) usually performs all of those same core tasks but—depending on the employer and state rules—receives extra training to carry out limited clinical procedures (for example, drawing blood, running EKGs, or assisting with specimen collection). In short: CNAs focus tightly on direct patient care and daily living needs, while PCTs blend that hands-on care with additional technical skills.
How does a certified nursing assistant differ from a patient care technician in duties?
CNAs spend most of their shift performing activities of daily living (bathing, dressing, feeding, toileting), turning and repositioning patients, observing and reporting changes, and taking routine measures like vital signs. Their work is essential to patient comfort and safety and forms the bulk of bedside contact. PCTs perform those same ADLs but are more commonly trained to assist with basic clinical tasks that require some technical skill (phlebotomy, EKG tracing, some basic specimen handling, and sometimes use of specialized equipment). These additional duties mean PCTs are often scheduled in settings where those technical skills are needed on top of personal care.
Example: on a medical–surgical floor a CNA may be assigned to assist six patients with hygiene and ambulation and to report any changes to the charge nurse. A PCT on the same unit might have a smaller patient load because they also draw morning labs and perform EKGs, then help with turning and feeding.
Where do CNAs and PCTs work — hospitals, nursing homes, long-term care facilities?
Both roles are found across the continuum of care—but the distribution differs by setting:
- Nursing homes and other long-term care facilities frequently employ large numbers of CNAs because residents need ongoing assistance with daily living and routine monitoring.
- Hospitals (medical–surgical units, telemetry, emergency departments, dialysis units) often employ PCTs because the workflow requires both bedside care and technical tasks like EKGs or specimen collection; CNAs are also present but may be more concentrated in units focused on ADLs.
- Rehabilitation centers, outpatient labs, and specialty clinics may employ PCTs when clinical support procedures are frequently needed. Both roles appear in assisted-living, home health, and other care facilities depending on local staffing models.
How do CNA and PCT roles relate to nursing staff like RNs and LPNs?
CNAs and PCTs work under the supervision and delegation of licensed nursing staff. A registered nurse (RN) typically oversees the plan of care, makes clinical assessments, and delegates specific tasks that CNAs and PCTs carry out. A licensed practical nurse (LPN) or vocational nurse often supervises daily tasks on smaller units and provides direct clinical care that is above the typical CNA/PCT scope (medication administration, some wound care). The licensed nurse remains accountable for patient assessment and for ensuring delegated tasks are appropriate and within state and facility policy. Good communication and accurate reporting from CNAs and PCTs to RNs/LPNs are essential for safe, coordinated care.
Practical illustration: an RN writes a care plan that requires hourly turning for a patient at high risk for pressure injury. A CNA implements the turning and documents the activity; a PCT might perform the turning and also record a post-turn EKG or draw a stat lab if the patient needs it—both actions are reported back to the RN, who integrates the information and updates the plan.
How do certification and training compare for CNAs and PCTs (certification, pct training, cna program)?
Certification and training requirements for Certified Nursing Assistants (CNAs) and Patient Care Technicians (PCTs) differ in length, scope, and complexity. While both roles involve direct patient care, the educational pathways reflect the different expectations of practice.
A cna program generally focuses on foundational patient care skills such as bathing, grooming, mobility assistance, feeding, and vital signs. The emphasis is on supporting patients with activities of daily living (ADLs) and ensuring comfort and safety in long-term care facilities, hospitals, and home-care settings.
On the other hand, pct training expands on CNA-level knowledge and includes more advanced clinical tasks. During a typical pct program, students learn skills such as ECG monitoring, phlebotomy, wound care assistance, specimen collection, and more advanced vital sign interpretation. Because PCTs work in more acute or specialized environments—such as emergency departments, ICUs, and outpatient clinics—the training equips them with technical competencies needed for fast-paced, high-acuity settings.
In summary:
| Aspect | CNA | PCT |
|---|---|---|
| Required Training | Shorter, foundational patient care | Longer, includes advanced clinical skills |
| Scope of Duties | Basic ADLs, mobility, vital signs | ECGs, phlebotomy, blood glucose testing, CNA-level tasks |
| Work Settings | Nursing homes, long-term care, home health | Hospitals, specialty units, outpatient centers |
| Credential Path | CNA certification | pct certification |
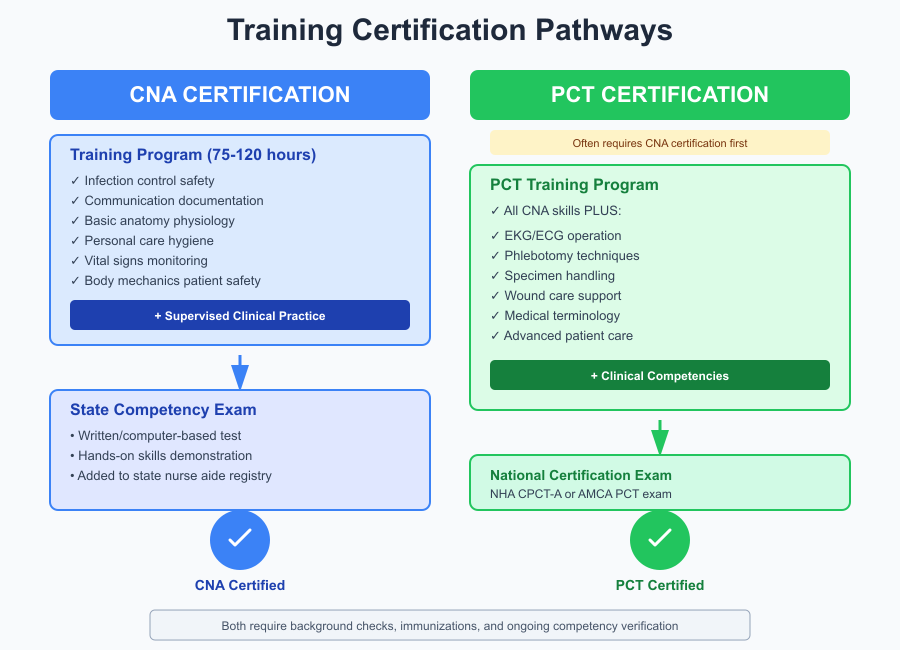
What does CNA certification and cna training involve?
CNA certification is typically obtained after completing cna training through a state-approved program. A standard cna program includes both classroom instruction and supervised clinical practice. Topics usually covered include:
- Infection control and standard precautions
- Communication and documentation
- Basic anatomy and physiology
- Patient safety and body mechanics
- Personal care and hygiene
- Vital signs and basic patient monitoring
Clinical practice allows students to apply skills directly to patient care under instructor supervision. After training, students must complete a state competency exam consisting of a written or computer-based test and a hands-on skills demonstration. Once passed, the individual receives CNA certification and is added to the state nurse aide registry.
Example: A student in a nursing home–based cna program may complete 75–120 hours of training, then perform skills such as transferring a resident using a gait belt or measuring pulse rate during the certification exam.
What are common pct program and pct certification requirements?
Most pct program requirements are built upon CNA-level competencies. Many states and institutions require candidates to have an active CNA certification before enrolling in pct training, although some programs accept students without prior CNA experience.
Common components of a pct program include:
- Advanced patient care skills (bathing, feeding, repositioning, catheter care)
- Electrocardiogram (EKG/ECG) operation and basic rhythm interpretation
- Phlebotomy and specimen handling
- Wound and skin care support
- Medical terminology and patient communication
- Safety and emergency procedures
To earn pct certification, students typically complete a national examination such as:
- National Healthcareer Association (NHA) CPCT-A exam
- American Medical Certification Association (AMCA) PCT exam
Requirements may include:
- Proof of completing a pct program
- Background check and immunizations
- Hands-on skill competencies
- Passing a national pct certification exam
Example: During pct training, a student may learn how to draw blood using venipuncture techniques and how to perform a 12-lead ECG—skills not included in standard cna training.
How long are training programs and what is on the certification exam?
Training duration varies by state and institution:
CNA Training Length
- 4–12 weeks on average
- Includes 60–120 classroom hours plus 16–40 clinical hours
CNA certification exam content typically includes:
- Infection control
- Personal care procedures
- Mobility and safety
- Vital signs
- Interpersonal communication
- Documentation principles
The skills test may include tasks such as hand hygiene, blood pressure measurement, or ambulation assistance.
PCT Training Length
- 3–6 months depending on depth of clinical skills
- Some hospital-based programs may run longer due to extended clinical hours
PCT certification exam content usually includes:
- CNA-level foundational skills
- ECG and cardiac monitoring
- Phlebotomy and specimen collection
- Wound and catheter care
- Basic medical-surgical procedures
- Patient safety and emergency response
Example exam scenario: A PCT candidate may be tested on how to place ECG leads, identify normal vs abnormal rhythms, perform venipuncture, and demonstrate safe patient transfers.
What are the typical job duties and daily tasks for CNAs and PCTs (job duties, basic patient care)?
Both Certified Nursing Assistants (CNAs) and Patient Care Technicians (PCTs) are essential members of the bedside care team who provide high-volume, hands-on patient support. Their job duties overlap considerably, but the emphasis differs by role and setting.
Common day-to-day responsibilities shared by both roles include:
- Assisting with mobility and transfers (bed ↔ chair, ambulation with gait belts or assistive devices).
- Helping with personal hygiene and grooming tasks.
- Assisting with feeding and ensuring patients receive their nutrition safely.
- Observing patients and reporting changes in condition to licensed nursing staff.
- Maintaining accurate, timely documentation of care tasks and observations.
CNAs tend to spend a higher proportion of their shift on basic patient care — direct, continuous attention to comfort and daily needs — while PCTs combine that caregiving with additional clinical tasks when the unit requires it. Both roles are supervised by licensed nurses and are evaluated on accuracy, timeliness, and the quality of hands-on care.
Which activities of daily living and direct patient care do CNAs perform?
Activities of daily living (ADLs) are the backbone of CNA practice and make up most of the CNA’s direct contact time with patients. Typical ADLs and direct patient care tasks performed by CNAs include:
- Personal hygiene: bed baths, shower assistance, oral care, hair care, shaving and grooming.
- Dressing and toileting: assisting with clothing choices, incontinence care, catheter care per facility policy.
- Feeding and nutrition support: helping with meals, following swallowing/diet precautions, documenting intake.
- Mobility: safe transfers (using lift teams or mechanical lifts when indicated), ambulation assistance, turning/repositioning to prevent pressure injury.
- Elimination: assisting with toileting schedules, measuring and recording urinary output when required.
- Observation & basic monitoring: routine checks and the initial identification and reporting of changes in skin integrity, behavior, or level of consciousness.
Example: In a long-term care unit a CNA may be assigned to six residents and will spend the morning shift assisting with hygiene, dressing, breakfast, and toileting; throughout the day they provide repositioning and social support, documenting completed ADLs for the care team. These tasks directly affect patient comfort, dignity, and outcomes.
What basic medical procedures and vital signs monitoring do PCTs handle?
PCTs frequently perform standard bedside clinical procedures that require technical competence beyond ADLs. Typical PCT responsibilities include:
- Vital signs monitoring and interpretation: frequent measurement and trend-reporting (blood pressure, pulse, temperature, respiratory rate, pulse oximetry) and escalation of abnormal findings.
- Phlebotomy and specimen collection: venipuncture, capillary blood draws, proper labeling and transport of specimens to the lab.
- Electrocardiograms (ECGs): lead placement, running 12-lead tracings, and recognizing gross abnormalities to alert the nurse or physician.
- Assisting with basic wound care or dressing changes under nurse direction (scope depends on facility).
- Use of basic medical equipment: oxygen delivery devices, glucose monitors, bladder scanners, and cardiac telemetry hookup.
Example: On a medical–surgical unit a PCT may be assigned to draw morning labs for several patients, perform scheduled ECGs, chart vital signs every four hours, and then assist with patient hygiene—mixing technical skill work and bedside care. These tasks require accurate technical performance and clear communication with RNs.
How do responsibilities vary between care facilities and hospital settings?
Care facilities (nursing homes, long-term care, assisted living)
- Workload emphasizes sustained ADL assistance, chronic condition monitoring, and building long-term rapport with residents.
- CNAs are the primary workforce for day-to-day resident support; their continuity of care aids in noticing gradual changes over time.
- Technical procedures (phlebotomy, ECGs) are less frequent on-site and often handled by visiting or dedicated clinical staff unless the facility employs PCTs.
Hospitals and acute-care units
- The environment is faster-paced; care priorities include frequent monitoring, rapid recognition of acute changes, and coordination with multidisciplinary teams.
- PCTs are more common in acute settings where technical procedures are routine (e.g., morning blood draws, telemetry setup, urgent ECGs). CNAs also work in hospitals but may be assigned more patients for ADLs and bedside support while PCTs balance ADLs with technical tasks.
- Hospitals require strict adherence to protocols for infection control, specimen handling, and documentation because diagnostic turnaround and treatment decisions are time-sensitive.
Clinical implications for nursing students: knowing the difference helps you anticipate workflow and priorities on different units. A student preparing for clinical rotations on a medical–surgical floor should expect frequent interactions with PCTs who can demonstrate phlebotomy and ECG setup; in long-term care, emphasis will be on ADL-focused care and relationship-based communication skills with CNAs
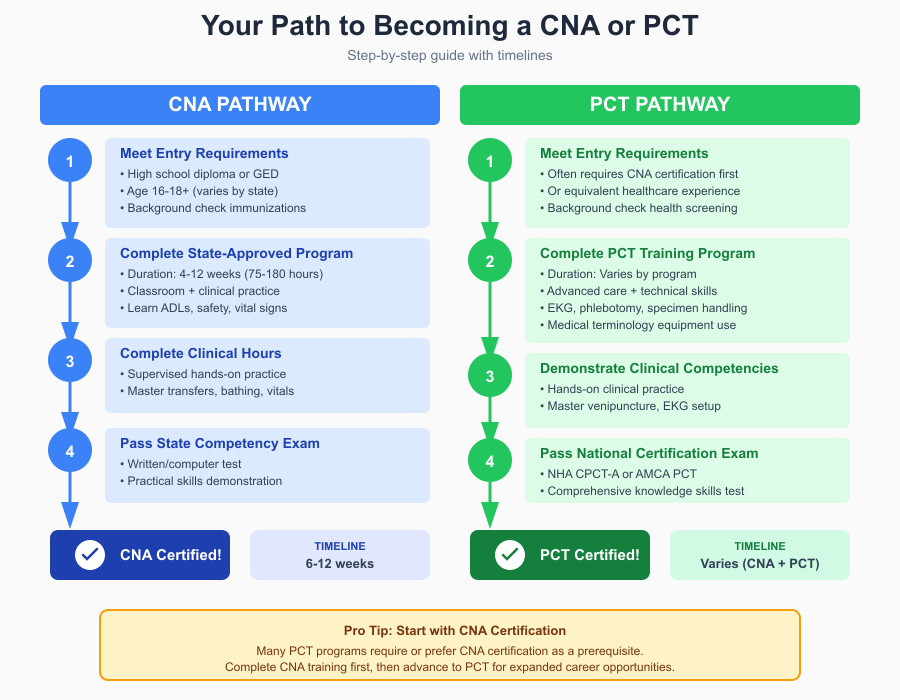
How do I become a CNA or a PCT — educational requirements and steps (becoming a certified nursing assistant, become a pct)?
Becoming a frontline caregiver starts with clear, sequential steps: meet entry requirements, complete an approved training track, pass competency testing, and gain supervised clinical experience. The paths to entry for a certified nursing assistant and a patient care technician overlap but differ in depth, time, and the technical skills emphasized. Below is a student-ready, step-by-step guide for each pathway plus realistic timelines and examples.
What are the entry requirements to become a CNA and enroll in a cna program?
1. Verify basic eligibility (entry requirements to become a CNA).
Most programs expect a high school diploma or GED (some local programs accept mature-age applicants without a diploma). Applicants typically must be at least 16–18 years old, provide proof of immunizations (MMR, Hep B, TB screening), and complete a background check and drug screen if required by the training site or future employer. Some regions add language or health-clearance requirements.
2. Enroll in a state-approved CNA program.
A state-approved CNA program combines classroom instruction with supervised clinical hours. Typical duration: 4–12 weeks (roughly 75–180 total hours, including hands-on clinical practice). Coursework covers infection control, basic anatomy, safe patient handling, ADLs, communication, and vital signs. Many community colleges, vocational schools, hospitals, and community organizations run these courses.
3. Complete required clinical hours and skills practice.
Clinical labs and practicum experiences are essential. Under instructor supervision you’ll practice transfers, bathing, feeding, and measuring vital signs until competent.
4. Pass the competency evaluation (state certification exam).
The exam usually includes a written (or oral/computer) knowledge test and a practical skills demonstration (e.g., hand hygiene, ambulation, measuring pulse or blood pressure). Passing the exam results in placement on the state nurse aide registry and the right to work as a CNA.
Example timeline: If you start a full-time CNA class in January, you may be eligible to test and begin work by March—roughly 6–12 weeks depending on program length and testing schedules.
How do you become a PCT and what pct program options exist?
1. Decide your entry route (direct PCT program vs. CNA first).
Some PCT programs require an active CNA credential before enrollment; others bundle CNA training into a longer PCT curriculum. Employer hiring practices vary—many hospitals prefer hires who already hold CNA certification plus phlebotomy or EKG training.
2. Enroll in a PCT program or stacked certificate pathway.
A common structure is modular: CNA fundamentals + phlebotomy + EKG/telemetry + basic lab/specimen handling. Program lengths differ widely: short tracks (6–8 weeks) exist for accelerated entry (often aimed at students with prior healthcare experience), while comprehensive PCT certificates typically run 2–4 months or longer if paced part-time. Many community colleges, technical schools, and hospital training centers offer PCT certificates that prepare students for national exams (e.g., NHA CPCT/A or AMCA PCT credentials).
3. Demonstrate competencies in technical skills.
Expect practical testing in venipuncture, capillary blood sampling, ECG lead placement and tracing, and safe patient transfers. Clinical externships or practicum hours show you can perform under real unit conditions.
4. Obtain employer-recognized certifications (optional but valuable).
National credentials such as Certified Patient Care Technician/Assistant (CPCT/A) or phlebotomy/EKG certifications improve hireability in hospitals and specialty units. Because there is no single nationwide PCT license, local norms determine which certificates matter most.
Example timeline: A stacked PCT certificate that includes CNA, phlebotomy, and EKG can often be completed in 8–16 weeks full-time; hospital-run programs sometimes combine training with guaranteed placement or externships.
Can CNAs advance into LPN, RN, or other nursing programs and career in healthcare?
Yes — working as a CNA or PCT is a common, practical entry point into higher nursing education and allied health careers. The hands-on experience gives applicants an advantage for competitive nursing programs.
Typical advancement routes:
- CNA → LPN (Licensed Practical Nurse): LPN programs usually take 12–18 months, include classroom and clinical coursework, and conclude with the NCLEX-PN licensure exam. Many LPN programs accept CNA experience as a strength in applications and occasionally offer bridge options or credit for prior learning.
- CNA → RN (ADN/BSN): There are no universal “CNA-to-RN” shortcuts, but CNAs commonly enter associate degree (ADN, ~2 years) or bachelor’s (BSN, ~4 years) tracks. CNA experience helps with clinical confidence and sometimes meets prerequisite clinical hour expectations. Some nursing schools offer accelerated or flexible entry paths for working CNAs.
- Lateral allied health growth: PCTs with phlebotomy/EKG skills may transition into roles such as medical assistant, phlebotomy tech, or clinical lab assistant; further education can lead to roles like respiratory therapist, radiologic tech, or paramedic.
Practical advice: Keep transcripts, clinical competency logs, and employer references. Work experience as a CNA/PCT strengthens applications and provides practical context for nursing coursework. Many employers support tuition assistance for staff pursuing LPN/RN training—ask about employer education benefits and flexible scheduling for classes/clinical rotations.
What is the salary and job outlook for CNAs versus PCTs (salary, job outlook)?
Companion bedside roles such as Certified Nursing Assistants (CNAs) and Patient Care Technicians (PCTs) are in steady demand, and their compensation reflects factors like setting, geographic region, shift worked, and any extra clinical credentials held. Below I compare typical pay ranges, review labor-market projections, and explain how additional skills and workplace choices influence both immediate salary and longer-term advancement opportunities.
What are typical salary ranges for CNAs and pcts in different healthcare settings?
Authoritative national data for nursing assistants (the BLS occupational category that includes CNAs) shows a median annual wage of $39,530 (May 2024). The distribution is wide: the lowest 10% earned under about $31,390 and the highest 10% earned more than $50,140. These figures reflect large state-by-state and setting-based variation.
PCT pay estimates vary because PCTs are not always listed separately in federal data. Employer-reported and crowdsourced sources place typical PCT pay slightly above or similar to CNA pay in many markets. For example, Glassdoor and other salary aggregators report average PCT salaries in the low-to-mid $40,000s annually (roughly $18–$22/hour), with hospital-based PCTs and those with phlebotomy or EKG skills toward the higher end. ZipRecruiter and Indeed show regional differences and a range that commonly spans roughly $32,000–$50,000 depending on experience and duties.
Setting matters:
- Nursing homes / long-term care: CNAs here often make toward the lower end of the national distribution, though unionized facilities or high-cost states may pay more.
- Hospitals (medical–surgical, telemetry, ED): PCTs working in hospitals—especially units requiring phlebotomy/ECG support—typically command higher pay and more frequent shift differentials (nights/weekends), which raises total compensation.
- Specialty clinics / dialysis / cardiac units: Technically skilled PCTs (dialysis, telemetry) often earn premiums due to specialized duties and training.
Example: A CNA in a rural nursing home might earn near $31,000–$35,000/year, while a hospital PCT with phlebotomy and telemetry experience in an urban area could reasonably earn $45,000+/year including shift differentials.
What is the job outlook and demand for cnas and pcts in the healthcare industry?
Demand for bedside support roles remains resilient. The U.S. Bureau of Labor Statistics projects continued employment needs for nursing assistants due to an aging population and staffing patterns that rely on direct-care personnel; median projections and short-term estimates indicate steady (moderate) growth. Other industry analyses and training programs also report ongoing, localized shortages that make hiring for CNAs and PCTs frequent across facilities. Because PCTs bring technical skills, they may find broader hiring opportunities in acute care settings compared with CNAs who are most heavily employed in long-term care.
Practical implication for students: Entry-level job availability is usually strong, but the type of opening differs by sector—expect more CNA openings in long-term care and more PCT openings in hospitals and specialty units.
Do certification and additional skills affect pay and advancement opportunities?
Yes—additional clinical credentials and skills (phlebotomy, ECG/telemetry, dialysis tech, medication aide training) commonly translate to higher starting pay, more desirable shifts, and better promotion prospects. Multiple sources and employer job postings show that CNAs or PCTs who hold recognized certificates (or who can demonstrate competency in blood draws, EKG lead placement, or specialized equipment) frequently earn wage premiums and are preferred for hospital roles that require those functions. Cross-training (for example, adding phlebotomy to a CNA background) is one of the fastest ways to increase marketability and hourly pay.
Other factors that raise pay or advancement potential:
- Shift differentials: nights, weekends, and holidays pay more.
- Region/state cost of living: urban and high-cost states pay higher nominal wages.
- Union contracts or employer pay scales: some long-term care employers offer step increases for tenure or credentials.
- Experience and demonstrated reliability: supervisors value clinical judgment and documentation accuracy—traits that support promotion into charge roles or technical positions.
Example: A CNA who completes a PCT program with phlebotomy competency and an ECG certificate can often move from a nursing-home CNA role into an entry-level hospital PCT position with a $3,000–$8,000 annual pay increase (varies by market and employer).
Bottom line for nursing students
- If immediate entry and rapid employment are priorities, CNA roles provide reliable hiring and a valuable clinical foundation.
- If you want higher starting pay and broader hospital opportunities, plan to add technical certificates (phlebotomy, EKG) or enroll in a PCT track.
- Track local labor-market data (hospital job postings, regional pay surveys) because precise wage levels and demand are highly location-dependent.
Which career path should I choose: CNA, PCT, or medical assistant (career path, pct or cna, medical assistant)?
Choosing a healthcare career is a multifaceted decision for nursing students or aspiring healthcare workers. The decision to pursue a CNA, PCT, or medical assistant role depends on your career goals, desired work environment, willingness to pursue additional education, and long-term trajectory in the healthcare industry. Each role provides a unique mix of job duties, patient contact, technical skill development, and career advancement opportunities. Below is a detailed comparison to guide informed decision-making.
How do career paths compare for a certified nursing assistant, patient care technician, and medical assistant?
Certified Nursing Assistant (CNA)
- Primary focus: Hands-on patient care and activities of daily living (ADLs) in long-term care, nursing homes, and some hospitals.
- Training duration: 4–12 weeks on average.
- Career trajectory: CNAs gain essential patient care experience and may leverage their position to advance into LPN, RN, or specialized care programs.
- Pros: Fast entry into the workforce, stable demand, exposure to bedside care, foundational for nursing programs.
- Cons: Limited technical skill development and lower starting salary compared to PCTs or medical assistants in hospitals.
- Example: A CNA in a nursing home may develop strong observational and communication skills, making them competitive applicants for LPN bridge programs.
Patient Care Technician (PCT)
- Primary focus: CNA-level duties plus basic clinical procedures such as ECGs, phlebotomy, and lab specimen handling.
- Training duration: 2–4 months, often requiring prior CNA experience or concurrent training.
- Career trajectory: PCT experience positions candidates for hospital-based roles, technical certifications, or transitions to allied health programs.
- Pros: Higher salary potential, exposure to acute care settings, broader technical skill set.
- Cons: Longer training requirements and more responsibility; duties are faster-paced and may be stressful in acute care units.
- Example: A PCT in a hospital telemetry unit performs vital signs, blood draws, and ECG monitoring, building competencies that can support later nursing or technical certifications.
Medical Assistant (MA)
- Primary focus: Clinical and administrative support in outpatient clinics, physician offices, and specialty practices. Duties include vitals, injections, medication administration (where allowed), scheduling, billing, and patient communication.
- Training duration: 9–12 months (certificate or diploma programs); associate degree options extend to 2 years.
- Career trajectory: MAs can advance into nursing, medical office management, or specialized clinical roles.
- Pros: Exposure to both patient care and administrative workflows, potential for broader career paths in outpatient healthcare.
- Cons: Less hands-on inpatient experience; hospital bedside skills may be limited.
- Example: A medical assistant in a primary care clinic draws blood, administers vaccines, schedules appointments, and maintains EMR documentation.
Which role is best for long-term care, hospital work, or entry into nursing programs?
- Long-term care / nursing homes: CNAs are the backbone of care. Their primary responsibilities are ADLs, mobility support, and patient observation. This environment provides stable work hours and a slower pace ideal for building foundational patient care skills.
- Hospital / acute care settings: PCTs are more commonly employed in hospitals due to their technical skills. Units such as medical–surgical, telemetry, and emergency departments benefit from PCTs who can perform phlebotomy, ECGs, and assist with multiple clinical procedures.
- Entry into nursing programs: CNAs and PCTs both provide strong preparation, but CNAs may be preferable for those seeking gradual exposure to patient care before committing to technical procedures. PCT experience adds technical competencies that can make students more competitive for hospital-based nursing programs or advanced technical certifications. Medical assistants provide a different perspective, with administrative experience that may be less relevant for inpatient nursing programs but advantageous for outpatient or clinic-focused nursing careers.
Example: A student planning to pursue an RN program may start as a CNA in a long-term care facility to develop strong patient communication and observation skills, then transition to a hospital-based PCT role to acquire technical experience in preparation for clinical rotations.
What factors — certification, training time, salary, and job duties — should influence my decision?
- Certification and credentials: CNA and PCT certification can open doors to hospital employment, specialized units, or further education. Additional certifications (e.g., phlebotomy, ECG) increase job market competitiveness.
- Training time and cost: CNA programs are the shortest (4–12 weeks), PCT programs are intermediate (2–4 months), and medical assistant programs are longer (9–12 months or more). Students must weigh immediate employment needs versus long-term goals.
- Salary considerations: CNAs generally earn less than PCTs and some MAs, but geographic region and facility type affect pay. Hospital-based PCTs with technical skills often command higher wages than nursing home CNAs.
- Job duties and patient interaction: Evaluate the desired work environment—long-term relationship-building with residents (CNA), technical and acute care tasks (PCT), or outpatient administrative-clinical balance (MA).
- Career trajectory: CNAs and PCTs often progress into LPN, RN, or other allied health roles. MAs can transition to nursing programs or administrative healthcare positions. Choosing a role aligned with long-term goals maximizes return on initial education and training investment.
Decision-making example: A student with limited time and immediate financial needs may start as a CNA, gaining patient care experience and certification quickly. Another student targeting hospital work with higher pay and exposure to technical clinical procedures may choose a PCT program. If the student prefers outpatient clinics, administrative tasks, and broader scope for medical office career progression, the medical assistant path may be optimal.
Conclusion
Choosing between a CNA, PCT, or medical assistant role is a critical decision for nursing students and aspiring healthcare professionals. Each career path offers distinct opportunities for skill development, patient interaction, and long-term advancement. CNAs provide foundational exposure to direct patient care, focusing on activities of daily living and bedside support in long-term care facilities and nursing homes. PCTs expand upon this foundation, integrating technical competencies such as phlebotomy, ECG monitoring, and basic medical procedures, making them highly valuable in hospital and acute-care settings. Medical assistants combine clinical and administrative responsibilities, often in outpatient clinics, preparing students for both patient care and healthcare operations roles.
The decision between these roles should consider several key factors: training requirements, certification pathways, salary expectations, job duties, and your personal career trajectory. Students seeking rapid entry into patient-facing roles may prioritize CNA programs, while those aiming for technical experience, hospital exposure, or higher compensation may find PCT programs more suitable. Similarly, those interested in outpatient or administrative healthcare work might consider medical assistant training for a broader scope of responsibilities.
Ultimately, starting as a CNA or PCT not only provides hands-on clinical experience but also establishes a strong foundation for advancing into LPN, RN, or other allied health programs. By understanding the differences in responsibilities, training, and career growth potential, nursing students can make informed decisions that align with both immediate employment goals and long-term aspirations in the healthcare industry. Regardless of the path chosen, each role contributes meaningfully to patient care, healthcare team effectiveness, and the overall well-being of patients across care settings.
Frequently Asked Questions
What is the difference between a patient care assistant and a patient care technician?
A Patient Care Assistant (PCA) typically performs basic patient care tasks such as bathing, feeding, and assisting with activities of daily living, mostly in nursing homes or long-term care settings. A Patient Care Technician (PCT) performs similar duties but also handles technical clinical tasks like phlebotomy, EKG monitoring, and basic lab specimen collection, usually in hospital or acute-care settings. PCTs have additional training and certification for these clinical procedures.
Which one is better, CNA or PCT?
“Better” depends on career goals. CNAs provide foundational patient care and are ideal for long-term care or early exposure to healthcare. PCTs have higher earning potential and more technical skills, making them preferable for hospital work and advancement into specialized nursing or allied health roles.
Is a licensed nursing assistant the same as a certified nursing assistant?
Not exactly. A Certified Nursing Assistant (CNA) has completed a state-approved training program and passed a certification exam. Some states may use the term Licensed Nursing Assistant (LNA) interchangeably, but in practice, CNA is the standard recognized credential nationwide. Always check your state’s registry to confirm the credential type.
What is the difference between a health care assistant and a certified nursing assistant?
A Health Care Assistant (HCA) is a broad term used internationally or in some U.S. facilities to describe staff who assist with patient care, which may or may not require formal certification. A CNA is a formally trained and certified professional with a state-recognized credential and is authorized to provide specific nursing-related tasks under supervision.
