
Charge Nurse: Roles, Responsibilities, Career Path, and How to Become a Charge Nurse
The role of the charge nurse is a pivotal element within the nursing profession, bridging the responsibilities of bedside care with leadership and administrative oversight. Charge nurses are registered nurses who assume accountability for the smooth functioning of a nursing unit or department, ensuring that patient care is coordinated, staff nurses are supported, and clinical operations proceed efficiently. Far from being solely a supervisory position, the charge nurse role integrates clinical expertise with leadership duties, requiring a balance between direct patient care and administrative responsibilities.
At its core, the charge nurse serves as a critical link between nursing staff and nurse managers, facilitating communication, guiding less experienced RNs, and supporting decision-making in high-pressure clinical environments. This leadership role involves not only overseeing the delivery of care but also mentoring staff, resolving conflicts, and coordinating admissions and discharges in ways that optimize patient outcomes. The responsibilities of a charge nurse often extend to ensuring compliance with institutional protocols, maintaining safety standards, and addressing emergent situations with clinical and managerial proficiency.
Understanding the charge nurse role is essential for registered nurses seeking career progression, as it provides foundational experience for advanced leadership positions such as nurse manager or nurse leader. Becoming a charge nurse requires a combination of education, clinical competence, and nurse leadership skills, including communication, delegation, and team management. Whether working in specialized areas like the emergency department or leading a general medical-surgical unit, charge nurses must navigate complex dynamics while maintaining high standards of patient care and fostering a collaborative environment for nursing staff.
This article provides a comprehensive exploration of the charge nurse position, detailing the duties and responsibilities, the differences between a charge nurse and a nurse manager, career pathways for RNs aspiring to this leadership role, and practical strategies for professional growth. By examining the clinical, administrative, and leadership dimensions of the charge nurse career, nursing students and practicing RNs can gain insight into the competencies and experiences required to excel in this integral nursing role.
Understanding the Role of a Charge Nurse
The charge nurse is a registered nurse who plays a critical leadership role within a nursing unit or department, acting as the link between bedside nursing staff and nurse managers. This role goes beyond traditional patient care, combining clinical expertise, leadership skills, and administrative responsibilities to ensure that the nursing unit operates smoothly and safely. Charge nurses oversee patient care, mentor staff, coordinate unit operations, and support nurse managers in implementing policies and maintaining standards of practice.
By balancing these responsibilities, charge nurses enhance the quality of patient care, promote teamwork among nursing staff, and contribute to the overall efficiency of the unit. This position demands not only strong clinical competence but also exceptional leadership skills, the ability to make rapid decisions under pressure, and the capacity to manage both human and material resources effectively.
Charge Nurse vs Nurse Manager
Although the charge nurse and nurse manager both occupy leadership roles, their responsibilities differ in scope and focus:
- Charge Nurse: Concentrates on day-to-day operations within the nursing unit. They supervise staff nurses, delegate nursing duties, oversee patient care, and coordinate admissions and discharges. Charge nurses are often the first point of contact for clinical questions or operational issues during a shift.
- Nurse Manager: Focuses on administrative and strategic responsibilities, such as staffing, budgeting, policy enforcement, performance evaluations, and long-term planning for the unit or department. Nurse managers may intervene in complex situations but rely on charge nurses for real-time unit management.
Collaboration Between Roles:
Charge nurses and nurse managers work together to maintain patient safety, improve workflow, and support nursing staff development. For example, a charge nurse may alert the nurse manager to an unexpected patient surge, prompting the manager to reassign resources or authorize additional staffing. This collaborative dynamic ensures that patient care and unit operations remain uninterrupted while allowing the nurse manager to focus on broader strategic objectives.
Key Responsibilities of a Charge Nurse on the Nursing Unit
The responsibilities of a charge nurse encompass both clinical oversight and leadership duties. Key aspects include:
- Overseeing Patient Care: Charge nurses ensure that patient care is delivered safely, efficiently, and in alignment with care plans. They monitor patient status, support staff in responding to clinical changes, and intervene when complex situations arise. For example, in a medical-surgical unit, a charge nurse may supervise care for postoperative patients, ensuring timely pain management and monitoring for complications such as infection or bleeding.
- Delegating Nursing Duties: Tasks are assigned based on staff skills, patient acuity, and unit workflow. Charge nurses ensure that workloads are balanced and that staff nurses can focus on tasks aligned with their expertise.
- Coordinating Admissions and Discharges: Charge nurses facilitate smooth patient flow by managing bed assignments, verifying patient documentation, and communicating discharge instructions. In high-volume settings, such as an emergency department, this function is critical to preventing bottlenecks and maintaining quality care.
- Supporting Nursing Staff: Charge nurses mentor new RNs, resolve conflicts, and provide guidance to bedside nurses. They often lead shift briefings to clarify patient care priorities, assign responsibilities, and ensure that all team members are aligned.
- Administrative Duties: Beyond patient care, charge nurses review documentation, ensure compliance with protocols, and manage incident reports. Their administrative oversight allows nurse managers to focus on strategic planning and policy implementation.
Leadership Skills and Nurse Skills Required
Effective charge nurses must combine clinical knowledge with strong leadership capabilities. Key competencies include:
- Communication Skills: Essential for delegating tasks, coordinating with multidisciplinary teams, and providing guidance to staff nurses.
- Team Management: The ability to organize, motivate, and support nursing staff to achieve unit goals.
- Conflict Resolution: Addressing interpersonal or professional disputes effectively while maintaining a collaborative environment.
- Clinical Competence and Decision-Making: Charge nurses must assess patient conditions, prioritize care, and intervene in emergent situations, especially in high-acuity environments like the emergency department.
- Adaptability: Balancing patient care, staff management, and administrative responsibilities requires flexibility and strong time management.
Example: In an emergency department, a charge nurse may triage several critical patients simultaneously, assign nursing staff according to experience and patient needs, and communicate urgent updates to the nurse manager — all while ensuring that patient care is delivered safely and efficiently.
Career Path and How to Become a Charge Nurse
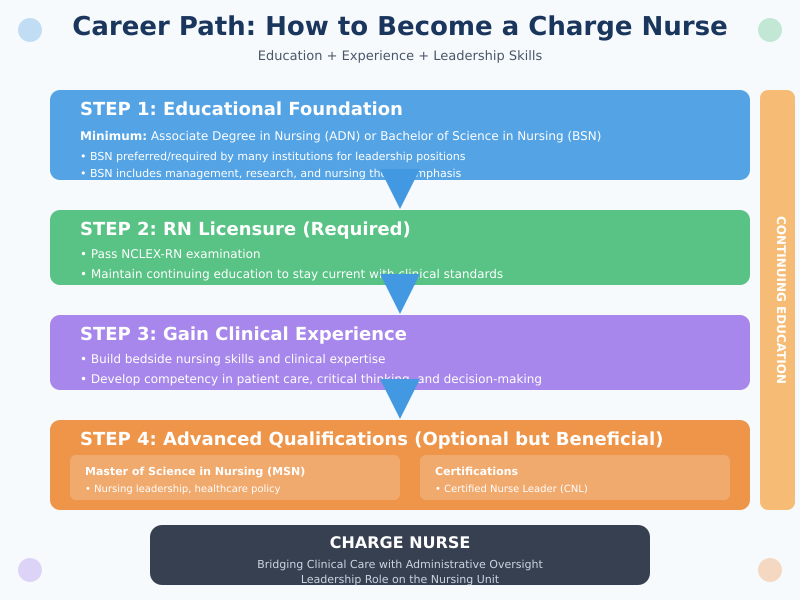
The path to becoming a charge nurse involves a combination of formal education, professional experience, and the development of leadership skills. Charge nurses are registered nurses who take on additional responsibilities, bridging clinical care with administrative oversight, and serving as leaders on the nursing unit. Understanding the educational requirements, necessary skills, and steps for career progression is essential for RNs aspiring to this leadership role.
Education and Qualifications
Becoming a charge nurse begins with a strong educational foundation and licensure as a registered nurse (RN). The minimum requirement is typically an associate degree in nursing (ADN) or a bachelor of science in nursing (BSN). While an ADN allows entry into clinical practice, many healthcare institutions prefer or require a BSN for leadership positions due to the emphasis on management, research, and nursing theory.
- RN Licensure: All aspiring charge nurses must be licensed as a registered nurse. This requires passing the NCLEX-RN exam and maintaining continuing education to stay current with clinical standards.
- Advanced Degrees: Pursuing a master of science in nursing (MSN) can enhance opportunities for leadership roles, including nurse manager positions, specialized clinical roles, and administrative responsibilities. An MSN often emphasizes nursing leadership, healthcare policy, and advanced patient care management.
- Certifications: While not always mandatory, certifications such as Certified Nurse Leader (CNL) or specialty-specific credentials (e.g., critical care, emergency nursing) can strengthen a charge nurse’s qualifications, demonstrating expertise in both clinical and leadership domains.
- Continuing Education: Charge nurses must engage in ongoing professional development to refine clinical skills, stay informed about evidence-based practices, and develop leadership competencies.
Example: A registered nurse with a BSN who has completed additional training in leadership and emergency care may be better positioned for a charge nurse role in a high-acuity unit like the emergency department.
Developing Nurse Leadership Skills
Beyond formal education, the development of nurse leadership skills is critical for success as a charge nurse. Leadership in nursing involves not only supervising staff but also fostering collaboration, ensuring effective communication, and promoting a culture of accountability and patient safety.
Key nurse leadership skills for aspiring charge nurses include:
- Communication Skills: Clear, concise communication is essential for delegating tasks, coordinating patient care, and interacting with nursing staff and other healthcare professionals.
- Mentorship and Coaching: Charge nurses often mentor new RNs and staff nurses, guiding them through clinical challenges and helping them develop critical thinking skills.
- Conflict Resolution: Managing disagreements among staff or addressing patient-related concerns requires diplomacy, empathy, and problem-solving abilities.
- Decision-Making and Critical Thinking: Charge nurses must make rapid, evidence-based decisions that affect patient outcomes and unit operations.
- Time Management and Prioritization: Balancing administrative responsibilities, staff supervision, and patient care demands strong organizational skills.
Example: On a busy medical-surgical unit, a charge nurse may need to allocate staff according to patient acuity, resolve a scheduling conflict between RNs, and ensure that all patients receive timely interventions — demonstrating both leadership and clinical competence.
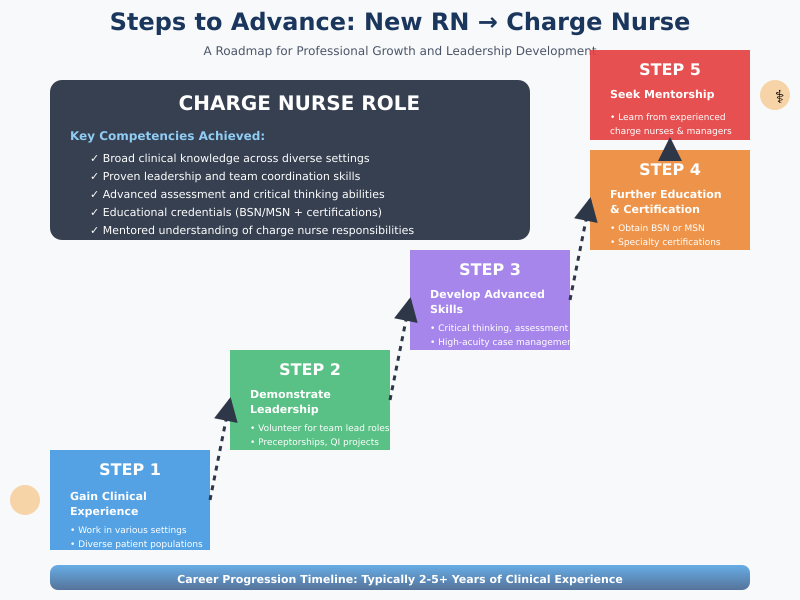
Steps for New RNs to Advance to Charge Nurse
For new nurses aspiring to a career as a charge nurse, several steps can facilitate professional growth and readiness for the role:
- Gain Clinical Experience:
- Work in various clinical settings to develop a broad base of nursing knowledge.
- Exposure to different patient populations helps build confidence in clinical decision-making.
- Demonstrate Leadership Potential:
- Volunteer for team lead roles, preceptorships, or quality improvement projects.
- Take initiative in mentoring peers or organizing shift workflows.
- Develop Advanced Nurse Skills:
- Strengthen assessment, critical thinking, and patient management skills.
- Gain proficiency in coordinating care, documentation, and handling high-acuity cases.
- Pursue Further Education and Certification:
- Consider obtaining a BSN or MSN if not already completed.
- Explore specialty certifications relevant to the unit or department (e.g., emergency nursing, critical care).
- Seek Mentorship from Experienced Charge Nurses or Nurse Managers:
- Guidance from established leaders helps new RNs understand the nuances of the role, including managing nursing staff, coordinating admissions and discharges, and collaborating with nurse managers.
Example: A new RN working on a pediatric unit might begin by leading small projects, mentoring nursing students, and gradually taking on additional leadership responsibilities during shifts. Over time, this experience, combined with ongoing education and demonstrated leadership skills, positions the RN to become a charge nurse.
Charge Nurse Job Description and Daily Duties
The charge nurse job description encompasses a wide range of responsibilities that blend clinical oversight, leadership, and administrative duties. Charge nurses are registered nurses who act as the central point of accountability on a nursing unit or department, ensuring that patient care is delivered safely, efficiently, and according to professional standards. Their daily duties require balancing direct patient care with the coordination of staff nurses and collaboration with nurse managers.
Patient Care Oversight
One of the primary functions of a charge nurse is monitoring patient safety, coordinating nursing care, and ensuring quality standards. Charge nurses are responsible for overseeing the care delivered by RNs and other nursing staff, ensuring that each patient receives appropriate interventions, and identifying potential risks to patient safety.
- Monitoring Patient Safety: Charge nurses continuously evaluate the safety of the nursing unit, ensuring compliance with infection control protocols, medication administration procedures, and fall prevention strategies.
- Coordinating Nursing Care: They facilitate communication between staff nurses, physicians, and ancillary departments to ensure that care plans are implemented effectively. For example, a charge nurse in a medical-surgical unit may coordinate care for a patient requiring multiple specialty consults, ensuring that treatments, labs, and follow-ups occur in a timely manner.
- Ensuring Quality Standards: Charge nurses review patient outcomes, audit documentation, and monitor adherence to evidence-based practices. They play a key role in maintaining unit accreditation standards and promoting a culture of quality improvement.
Example: In a high-acuity unit, a charge nurse may detect early signs of sepsis in a patient, assign immediate interventions to staff nurses, and escalate the case to the attending physician — demonstrating both clinical competence and leadership oversight.
Nursing Duties on the Unit
Beyond patient care, charge nurses are responsible for a wide range of nursing duties that support the efficiency and effectiveness of the nursing unit. These duties involve supervision, delegation, documentation, and workflow management:
- Delegation: Charge nurses assign tasks to staff nurses based on their experience, skill level, and patient needs. For example, a charge nurse may assign a complex post-operative patient to an experienced RN while delegating routine medication administration to a newer staff nurse.
- Supervision of Staff Nurses: Charge nurses monitor nursing performance, provide guidance on complex patient scenarios, and mentor RNs to strengthen clinical decision-making and professional growth.
- Documentation Oversight: Accurate and complete documentation is critical for patient safety and compliance. Charge nurses review care notes, medication administration records, and incident reports to ensure that all legal and institutional requirements are met.
- Unit Workflow Management: Charge nurses coordinate admissions, discharges, and patient transfers to maintain efficiency and reduce bottlenecks. They may adjust staffing assignments in real-time to address unexpected patient surges or emergencies.
Example: During a busy shift in an emergency department, the charge nurse organizes triage assignments, supervises staff nurses managing multiple critical patients, and ensures that all patient records are updated promptly — balancing direct patient oversight with administrative responsibilities.
Managing High-Pressure Situations
The ability to perform effectively under pressure is a hallmark of the charge nurse role. Charge nurses often face emergencies, high-acuity patients, and situations that require rapid decision-making:
- Emergency Response: Charge nurses lead the unit during codes, trauma alerts, and other urgent situations. They coordinate staff, prioritize interventions, and communicate critical information to the healthcare team.
- High-Acuity Patient Care: Charge nurses often oversee patients with complex medical conditions or unstable vitals, guiding staff in assessment, intervention, and escalation when needed.
- Decision-Making Under Pressure: Charge nurses must make quick, evidence-based decisions that balance patient needs, staff capacity, and unit resources. They must remain calm and composed, modeling leadership for the nursing staff.
Example: In an intensive care unit, a charge nurse may simultaneously manage a patient experiencing respiratory distress, assign an RN to monitor vital signs, coordinate with the respiratory therapist, and notify the attending physician — all while ensuring that the remaining patients receive uninterrupted care.
Charge Nurse Career in Specialized Settings
The role of a charge nurse extends across multiple nursing units, but specialized settings such as the emergency department (ED) require a heightened level of expertise, leadership, and decision-making. Charge nurses in these high-acuity environments must not only supervise staff nurses and oversee patient care but also maintain their own clinical competence while ensuring the unit operates efficiently and safely.
Specialized settings present unique challenges that differentiate the charge nurse role from other clinical or administrative positions, emphasizing adaptability, rapid decision-making, and advanced leadership skills.
Emergency Department Charge Nurse Role
The emergency department is one of the most dynamic and high-pressure environments in healthcare. Charge nurses in the ED are responsible for coordinating patient flow, assigning nursing duties, and ensuring that critically ill patients receive timely interventions.
Specific Challenges of ED Nursing:
- High Patient Acuity: Patients in the ED present with unpredictable and often life-threatening conditions, requiring immediate assessment and intervention.
- Rapid Decision-Making: ED charge nurses must triage patients effectively, determine priorities, and allocate staff resources based on patient acuity.
- Staff Supervision: The ED often requires coordination among multiple RNs, nursing assistants, and support staff simultaneously. The charge nurse must oversee their activities while ensuring quality care.
- Emotional Stress: Managing patient families, distressed patients, and high-stakes clinical situations adds complexity to the leadership role.
Example: During a multi-trauma scenario, the charge nurse may assign RNs to lead airway management, monitor vital signs, and prepare medications while simultaneously coordinating with physicians, lab services, and radiology. This demonstrates the integration of nurse skills, leadership, and clinical decision-making under intense pressure.
Maintaining Clinical Competence While Leading
One of the most significant challenges for charge nurses in specialized settings is balancing leadership duties with hands-on patient care. While they are responsible for overseeing the unit, charge nurses must maintain clinical proficiency to model best practices and intervene when necessary.
Strategies to Maintain Competence:
- Hands-On Care Participation: Even while supervising, charge nurses may provide direct care for high-acuity patients, demonstrating advanced procedures, assessments, or interventions.
- Continuing Education: Engaging in ongoing education, certifications, and workshops ensures that charge nurses remain current with evidence-based practices, clinical guidelines, and technological advancements.
- Simulation Training: Participation in mock codes, trauma drills, and emergency response simulations helps charge nurses refine their clinical skills while improving team coordination.
Example: A charge nurse in a cardiac unit may perform direct assessments of a patient experiencing arrhythmias while simultaneously directing RNs to prepare for emergency interventions — ensuring both leadership and clinical competence are maintained.
Leadership Techniques for Effective Team Management
Effective charge nurses leverage specific leadership strategies to enhance team performance, mentor staff, and promote patient safety.
Key Leadership Techniques Include:
- Mentorship and Coaching:
- Charge nurses provide guidance and feedback to RNs, fostering professional development and confidence.
- Example: A charge nurse may pair a new RN with an experienced staff nurse for complex patient care tasks, gradually increasing responsibilities as competence grows.
- Delegation Based on Competency:
- Assigning tasks according to each RN’s experience and skill level ensures efficiency and patient safety.
- Example: In an ED, a charge nurse may assign triage to an RN with strong assessment skills while delegating medication administration to a junior RN.
- Promoting Team Collaboration:
- Encouraging open communication and regular briefings enhances teamwork and reduces errors.
- Example: A charge nurse may conduct a pre-shift huddle to review patient load, clarify priorities, and address anticipated challenges.
- Conflict Resolution:
- Managing interpersonal conflicts among staff or addressing patient concerns diplomatically maintains a positive work environment.
- Example: If two RNs disagree on patient assignment, the charge nurse mediates to ensure tasks are distributed fairly without compromising patient care.
- Monitoring Quality and Safety:
- Charge nurses oversee adherence to safety protocols, evidence-based practices, and institutional policies.
- Example: Auditing documentation, reviewing incident reports, and ensuring infection control standards are met.
By implementing these leadership techniques, charge nurses supervise nursing staff effectively, enhance team collaboration, and create a culture of patient safety, even in the most demanding environments.
Charge Nurse Salary, Job Outlook, and Career Growth
A career as a charge nurse offers not only professional fulfillment but also competitive compensation and opportunities for advancement within the nursing field. Understanding salary expectations, variations, and long-term career growth helps registered nurses plan their career trajectory and identify opportunities to develop leadership skills while contributing to high-quality patient care.
Salary Expectations and Variations
The salary of charge nurses varies depending on factors such as geographic location, healthcare setting, years of experience, education, and the specific responsibilities associated with the role. According to the Bureau of Labor Statistics (BLS, 2024), registered nurses earn a median annual salary of approximately $82,750, but charge nurses typically earn a higher salary due to their leadership responsibilities and supervisory duties.
Factors Influencing Charge Nurse Salary Include:
- Healthcare Setting: Charge nurses in specialty units such as the emergency department, intensive care units, or surgical units often earn higher salaries due to the high-acuity nature of their patients and the complexity of their duties.
- Experience and Tenure: Charge nurses with extensive clinical experience, advanced certifications, and proven leadership skills often qualify for higher salaries compared to entry-level or less experienced charge nurses.
- Education: Those with a bachelor of science in nursing (BSN) or master of science in nursing (MSN) may receive higher compensation, reflecting their additional training and preparedness for leadership roles.
- Unit Size and Responsibilities: Charge nurses overseeing larger nursing units or multiple staff nurses may receive additional pay reflecting the administrative responsibilities required.
Example: A charge nurse in a high-volume emergency department may earn a median annual salary significantly higher than an RN in a general medical-surgical unit due to the demands of patient acuity, staffing coordination, and emergency response leadership.
In general, charge nurses make more than bedside nurses while also gaining experience in leadership and administrative roles, which can serve as a foundation for advancement to nurse manager positions.
Career Opportunities and Advancement
A career as a charge nurse serves as a stepping stone for multiple leadership and specialty roles within nursing. By demonstrating competence in clinical oversight, staff management, and patient care coordination, charge nurses can pursue various career pathways:
- Promotion to Nurse Manager:
- Charge nurses with strong leadership skills, experience in supervising RNs, and proficiency in administrative duties are well-positioned for promotion to nurse manager roles.
- Nurse managers oversee the overall operations of a unit or department, including budgeting, staffing, policy enforcement, and strategic planning.
- Specialty Nursing Roles:
- Charge nurses may choose to specialize in high-acuity areas such as the emergency department, intensive care, perioperative nursing, or neonatal units.
- Advanced certifications or a master of science in nursing (MSN) can enhance opportunities in specialty units, leadership roles, and educator positions.
- Leadership Development Opportunities:
- Aspiring nurse leaders can leverage the charge nurse role to gain mentorship, administrative experience, and strategic planning skills.
- Charge nurses often participate in quality improvement projects, staff development programs, and policy implementation initiatives, all of which strengthen leadership competencies.
Example: A charge nurse in a cardiac care unit who demonstrates expertise in patient care oversight and staff mentorship may advance to a nurse manager role, eventually taking on responsibilities for multiple units or serving as a director of nursing.
Long-Term Charge Nurse Career Outlook
The demand for charge nurses is expected to grow in the coming years due to several factors:
- Aging Population: Increasing patient needs, particularly among older adults with complex medical conditions, drives demand for skilled nurses capable of supervising and coordinating care.
- Expansion of Healthcare Services: Growth in hospitals, specialty clinics, and outpatient care settings creates more opportunities for leadership roles such as charge nurses.
- Focus on Patient Safety and Quality Care: Hospitals and healthcare systems emphasize quality improvement, patient safety, and evidence-based practices, making the charge nurse role essential for effective unit operations.
According to the Bureau of Labor Statistics, registered nursing positions are projected to grow 7% from 2022 to 2032, with higher demand in specialized units where charge nurses are integral to patient care oversight and staff supervision.
Long-Term Prospects for Charge Nurses Include:
- Advancement to nurse manager or nurse director positions, often accompanied by higher salary and broader leadership responsibilities.
- Opportunities to serve as clinical educators, preceptors, or mentors for nursing staff.
- Participation in hospital committees, quality improvement initiatives, and healthcare policy development, which can influence nursing practice and patient outcomes.
Example: A charge nurse with a decade of experience may progress to nurse manager in a high-acuity unit, later assuming leadership of multiple units or contributing to hospital-wide nursing leadership initiatives, highlighting the career growth potential within the profession.
Conclusion
The role of a charge nurse is pivotal within the nursing profession, blending clinical expertise, leadership skills, and administrative responsibilities to ensure that patient care is delivered safely, efficiently, and to the highest standard. Charge nurses serve as the backbone of the nursing unit, bridging the gap between bedside nursing staff and nurse managers, coordinating admissions and discharges, overseeing high-acuity patient care, and mentoring registered nurses.
Becoming a charge nurse requires more than technical competence; it demands strong nurse leadership skills, the ability to make critical decisions under pressure, and a commitment to fostering teamwork among nursing staff. Whether in high-intensity settings like the emergency department or specialized units, charge nurses must maintain their clinical competence while guiding and supporting their team, balancing administrative duties with hands-on patient care.
Career progression to a charge nurse position is rooted in a solid educational foundation, typically a bachelor of science in nursing (BSN) or master of science in nursing (MSN), RN licensure, and a demonstrated ability to lead and mentor others. Aspiring charge nurses, including new RNs, can advance through deliberate skill development, gaining experience, and actively seeking leadership opportunities on the nursing unit.
The charge nurse career also offers competitive compensation and a strong job outlook, with opportunities for advancement to nurse manager roles or specialized leadership positions. With healthcare systems increasingly prioritizing patient safety, quality outcomes, and staff development, charge nurses are essential to meeting these goals.
Ultimately, the charge nurse role is both challenging and rewarding. It empowers registered nurses to develop professionally, influence patient care outcomes, and contribute meaningfully to the growth and effectiveness of their nursing unit. By combining clinical expertise, leadership acumen, and administrative skill, charge nurses exemplify the integral link between high-quality patient care and effective nursing leadership.
Frequently Asked Questions
How does someone become a charge nurse?
To become a charge nurse, an individual must first be a licensed registered nurse (RN). Typically, this involves completing an associate degree in nursing (ADN) or a bachelor of science in nursing (BSN) and passing the NCLEX-RN exam. Many aspiring charge nurses pursue further education such as a master of science in nursing (MSN) or specialty certifications. Gaining clinical experience, demonstrating leadership skills, and actively participating in staff mentorship or unit management responsibilities are essential steps for advancing to this leadership role.
What are the duties of a charge nurse?
A charge nurse is responsible for overseeing patient care, supervising nursing staff, delegating nursing duties, and coordinating admissions and discharges on the unit. They ensure that care standards are met, monitor patient safety, provide mentorship to staff nurses, manage workflow, and serve as the primary point of contact for the nurse manager when escalations or critical decisions are needed. In specialized units, they may also handle emergency situations and high-acuity patient care.
What skills are needed as a charge nurse?
Charge nurses require a combination of clinical competence and leadership skills, including:
- Strong communication and team management skills to guide staff nurses and coordinate care.
- Critical thinking and decision-making under pressure, especially in high-acuity settings like the emergency department.
- Conflict resolution, mentorship, and the ability to oversee unit operations efficiently.
- Organizational skills for scheduling, delegating tasks, and managing nursing staff and administrative responsibilities.
Do charge nurses take patients?
Yes, charge nurses often take patients, especially in high-acuity or specialized units where they may need to intervene directly for complex cases. While their primary focus is supervising the nursing unit and staff, they maintain clinical competence by providing hands-on care when necessary, demonstrating procedures, or handling critical patient situations. The balance between leadership and bedside nursing ensures both patient safety and effective team management.
