STEMI vs NSTEMI: Clear Differences Between Acute Myocardial Infarction Types
Myocardial infarction remains a leading cause of morbidity and mortality worldwide, with different types of infarction presenting unique challenges for nursing assessment and patient management. Among these, ST-segment elevation myocardial infarction (STEMI) and non-ST-segment elevation myocardial infarction (NSTEMI) represent distinct clinical entities within the spectrum of acute myocardial infarction. While both conditions involve myocardial injury and compromised blood flow to the heart, their pathophysiology, electrocardiogram (ECG) presentation, risk factors, and treatment approaches differ significantly. Understanding these differences is essential for nurses, who are often the first to recognize early signs, monitor for complications, and implement evidence-based interventions that influence heart muscle damage and overall prognosis.
In clinical practice, timely identification of STEMI and NSTEMI can mean the difference between rapid reperfusion and preventable cardiac damage. Nurses must interpret subtle ECG changes, monitor cardiac biomarkers such as troponin, and recognize clinical presentations ranging from classic chest pain to atypical symptoms, particularly in patients with comorbidities or advanced age. Beyond acute care, nursing professionals also play a pivotal role in educating patients on secondary prevention strategies, helping mitigate cardiovascular risk and reduce the likelihood of recurrent heart attacks.
This article offers an in-depth exploration of STEMI vs NSTEMI, emphasizing pathophysiology, ECG patterns, diagnostic approaches, management strategies including percutaneous coronary intervention (PCI), and the role of nursing in optimizing patient outcomes. By integrating current clinical guidelines and evidence-based practices, this guide provides nursing students and practicing nurses with the knowledge needed to assess, manage, and support patients effectively across the continuum of acute coronary care. Through understanding these differences, nurses can contribute to improved short- and long-term outcomes, minimize heart muscle damage, and ensure safe, patient-centered care in the context of acute coronary syndrome
Understanding STEMI and NSTEMI
What Are STEMI and NSTEMI?
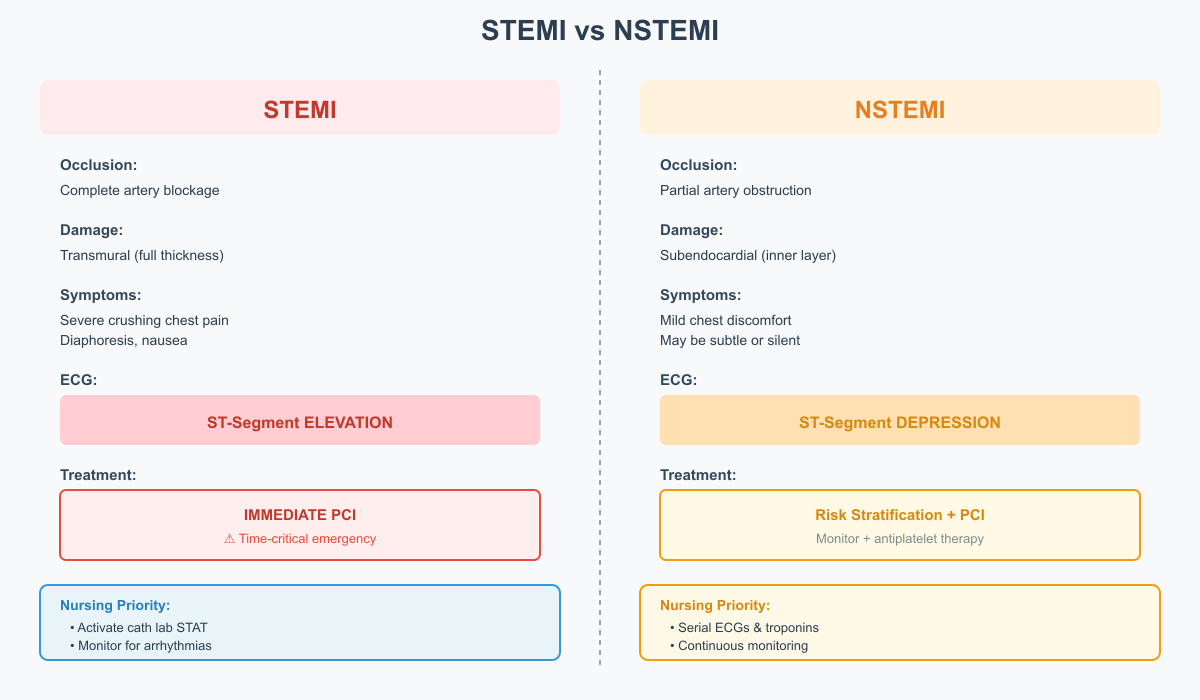
ST-segment elevation myocardial infarction (STEMI) and non-ST-segment elevation myocardial infarction (NSTEMI) are distinct forms of acute myocardial infarction, both resulting from a sudden reduction in blood flow to the heart muscle due to coronary artery disease. Both conditions fall under the broader category of acute coronary syndrome, but they differ in severity, clinical presentation, and treatment urgency.
STEMI occurs when a coronary artery is completely occluded, leading to transmural myocardial infarction, which affects the full thickness of the heart muscle. This type of infarction usually produces a characteristic ST-segment elevation on the ECG, and patients are at higher risk of heart muscle damage, heart failure, and cardiogenic shock if treatment is delayed. Immediate reperfusion through primary percutaneous coronary intervention (PCI) or thrombolytic therapy is essential to restore blood flow to the heart muscle and minimize short- and long-term damage.
NSTEMI, on the other hand, results from partial obstruction of a coronary artery, leading to subendocardial infarction, which affects only the inner layer of the myocardium. NSTEMI patients often present with less dramatic symptoms such as mild chest pain, fatigue, shortness of breath, or even silent myocardial ischemia, particularly in older adults and patients with diabetes. Although the immediate threat to heart muscle function is generally lower than in STEMI, NSTEMI carries a high risk of subsequent heart attacks and requires careful monitoring and management.
Clinical Example:
- A 58-year-old male presents with sudden, crushing chest pain radiating to the left arm and jaw, diaphoresis, and nausea. 12-lead ECG reveals ST-segment elevation in leads V2–V4, consistent with an anterior STEMI. Rapid activation of the cardiac catheterization team is initiated for primary PCI.
- A 70-year-old female with hypertension experiences mild chest discomfort and fatigue. Troponin is elevated, but the ECG shows ST-segment depression and T-wave inversion, indicating NSTEMI. She is managed with antiplatelet therapy, anticoagulation, and risk stratification before PCI.
Pathophysiology: How Myocardial Injury Differs Between STEMI and NSTEMI
The underlying myocardial injury in both STEMI and NSTEMI stems from coronary artery obstruction caused by plaque rupture or erosion, leading to thrombus formation and reduced blood flow to the heart.
- STEMI: Complete blockage of a coronary artery causes transmural myocardial infarction, damaging the entire thickness of the myocardium. This severe injury disrupts heart muscle contraction, increasing the likelihood of heart failure, cardiogenic shock, arrhythmias, and sudden cardiac death. Rapid reperfusion therapy is essential to limit damage to the heart muscle and improve prognosis.
- NSTEMI: Partial obstruction produces subendocardial infarction, affecting only the inner layers of the myocardium. Though the injury is less extensive, it can still compromise heart muscle function, produce elevated troponin levels, and predispose the patient to recurrent heart attacks and long-term cardiovascular complications.
Nursing Implications:
- STEMI patients require immediate monitoring for arrhythmias, hypotension, or acute heart failure, and urgent preparation for primary PCI.
- NSTEMI patients need risk assessment, continuous ECG monitoring, and serial troponin checks to guide timing of percutaneous coronary intervention and prevent further myocardial injury.
Example in Practice:
- A patient with complete occlusion of the left anterior descending artery develops significant anterior heart muscle damage, requiring rapid PCI.
- A patient with partial occlusion of a branch of the right coronary artery may show subtle ECG changes, yet still require intervention to prevent progression to full-thickness infarction.
HST-Segment Elevation and Non-ST-Segment Elevation: ECG Basics
The electrocardiogram (ECG) is a critical diagnostic tool for differentiating STEMI from NSTEMI.
- STEMI ECG Features:
- ST-segment elevation reflecting transmural myocardial injury.
- The affected leads correlate with the involved coronary artery:
- Anterior STEMI → leads V1–V4 → left anterior descending artery.
- Inferior STEMI → leads II, III, aVF → right coronary artery.
- Other findings may include hyperacute T waves, reciprocal ST depression, and eventual Q-wave formation.
- NSTEMI ECG Features:
- ST-segment depression, T-wave inversion, or other subtle changes indicative of subendocardial ischemia.
- These changes may be transient or less pronounced, making serial ECGs necessary for accurate diagnosis.
- Diagnosis often relies on elevated troponin levels in conjunction with ECG findings.
Nursing Considerations:
- Recognizing ST-segment elevation on the ECG allows immediate activation of PCI protocols, minimizing heart muscle damage.
- NSTEMI patients require ongoing ECG monitoring, observation for dynamic changes, and integration of troponin results to guide treatment planning.
Clinical Example:
- A patient with chest pain and ST elevation in II, III, aVF undergoes emergent PCI.
- Another patient presents with ST depression in lateral leads and elevated troponin, prompting initiation of NSTEMI treatment including antiplatelet therapy and monitoring for ischemic progression.
Clinical Presentation of STEMI and NSTEMI
Common Symptoms and Early Warning Signs
Patients experiencing STEMI and NSTEMI may present with a variety of symptoms, ranging from classic chest pain to subtle signs of myocardial ischemia, depending on the type of infarction and individual patient factors. Recognizing these early warning signs is crucial for nurses, as rapid identification and intervention significantly affect heart muscle damage and prognosis.
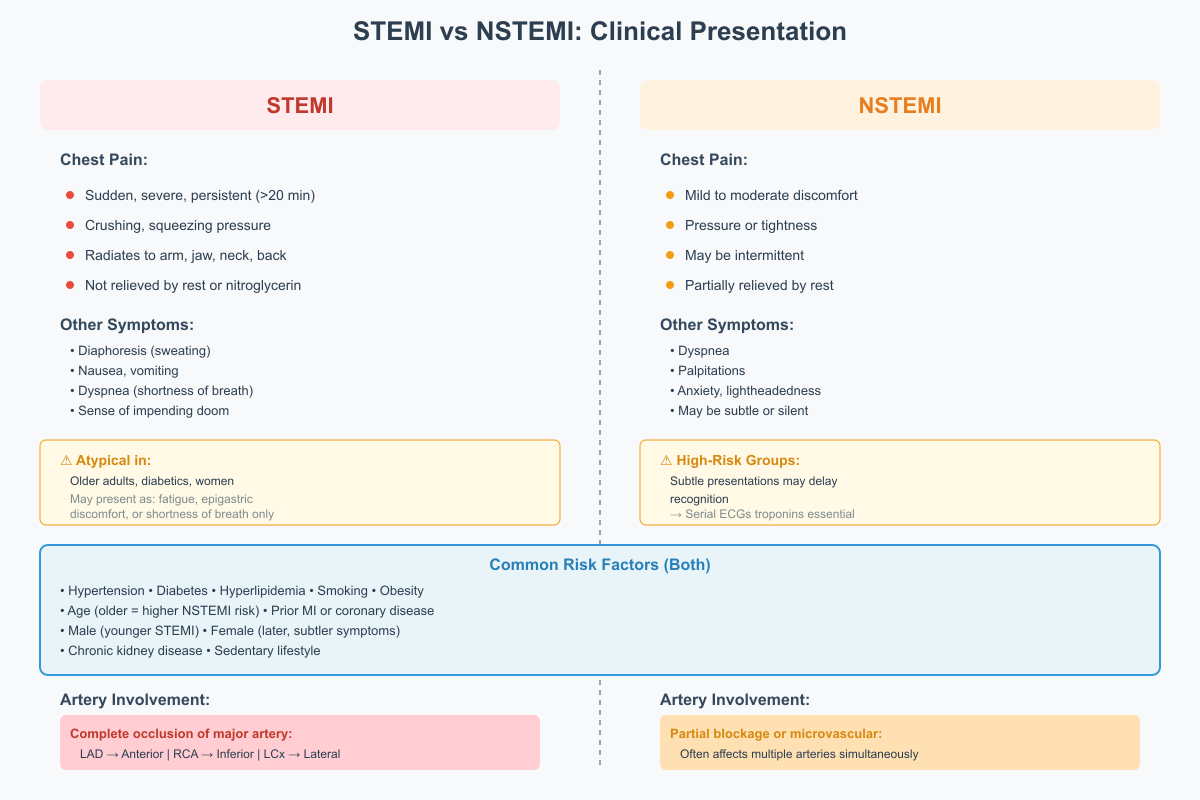
STEMI patients typically present with:
- Sudden, severe, and persistent chest pain lasting more than 20 minutes.
- Pain often described as crushing, squeezing, or pressure-like, radiating to the left arm, neck, jaw, or back.
- Associated symptoms such as diaphoresis, nausea, vomiting, dyspnea, or syncope.
- In some cases, particularly in older adults, diabetics, or women, the pain may be atypical, presenting as fatigue, epigastric discomfort, or shortness of breath.
NSTEMI patients, by contrast, often exhibit:
- Mild to moderate chest discomfort or pressure rather than the intense pain typical of STEMI.
- Symptoms may occur at rest or with minimal exertion and can be intermittent.
- Associated signs may include dyspnea, palpitations, anxiety, or lightheadedness.
- Subtle presentations in high-risk groups may delay recognition, emphasizing the importance of serial ECGs and troponin monitoring.
Example in Practice:
A 65-year-old man presents to the emergency department with intense chest pressure radiating to the jaw and diaphoresis. ECG shows ST-segment elevation in V3–V5, confirming STEMI. Rapid recognition allows activation of primary PCI, minimizing heart muscle damage.
Conversely, a 70-year-old female with diabetes experiences intermittent mild chest discomfort and fatigue. Troponin is elevated, and ECG shows T-wave inversion in lateral leads, indicating NSTEMI. Careful monitoring and risk assessment guide treatment and prevent progression.
Chest Pain Characteristics and Differentiation Between STEMI and NSTEMI
Chest pain is a key differentiating feature between STEMI and NSTEMI, although overlap exists. Understanding the nuances helps nurses prioritize acute interventions and assess myocardial injury risk.
- STEMI Chest Pain:
- Typically sudden, intense, and unrelieved by rest or nitroglycerin.
- May be described as crushing or heavy, sometimes accompanied by palpitations or a sense of impending doom.
- Often associated with ST-segment elevation on ECG and immediate myocardial injury.
- NSTEMI Chest Pain:
- Usually less severe, described as pressure, tightness, or mild discomfort.
- May be intermittent and partially relieved by rest or medications.
- Associated ECG findings include ST-segment depression or T-wave inversion, with subendocardial myocardial injury.
Nursing Consideration:
- Accurate assessment of chest pain characteristics is essential for differentiating STEMI from NSTEMI. Nurses should document onset, duration, location, radiation, intensity, and associated symptoms.
- Prompt recognition of STEMI symptoms triggers urgent reperfusion therapy, while recognition of NSTEMI patterns guides risk stratification and timely intervention.
Risk Factors and Coronary Artery Involvement
Understanding the risk factors and coronary artery involvement helps nurses anticipate which patients are more likely to experience STEMI or NSTEMI and informs preventive strategies.
Common Risk Factors Include:
- Traditional Cardiovascular Risk Factors
- Hypertension, diabetes mellitus, hyperlipidemia, smoking, obesity, and sedentary lifestyle.
- Age and Gender
- Older adults are at higher risk for NSTEMI and atypical presentations.
- Men are more frequently affected by STEMI at younger ages, whereas women may present later with subtler symptoms.
- History of Coronary Artery Disease
- Prior myocardial infarction, angina, or coronary stenting increases susceptibility.
- Other Contributing Factors
- Chronic kidney disease, inflammatory conditions, and certain medications may increase risk for NSTEMI and STEMI patients.
Coronary Artery Involvement:
- STEMI is usually associated with complete occlusion of a major coronary artery.
- Left anterior descending artery → anterior STEMI
- Right coronary artery → inferior STEMI
- Circumflex artery → lateral STEMI
- NSTEMI often involves partial blockage or microvascular ischemia, frequently affecting multiple coronary arteries simultaneously.
Example in Practice:
A patient with a history of hypertension and hyperlipidemia presents with ST-segment elevation in V1–V4, indicating anterior STEMI due to left anterior descending artery occlusion. Another patient with diabetes and chronic kidney disease has elevated troponin and ST depression in lateral leads, consistent with NSTEMI involving partial obstruction of multiple coronary arteries.
Nursing Implications:
- Assessment of risk factors enables early identification of patients at risk for STEMI and NSTEMI.
- Knowledge of coronary artery involvement helps anticipate complications such as heart failure, arrhythmias, or cardiogenic shock, and guides monitoring and treatment priorities.
Diagnostic Approach
Role of ECG in STEMI and NSTEMI
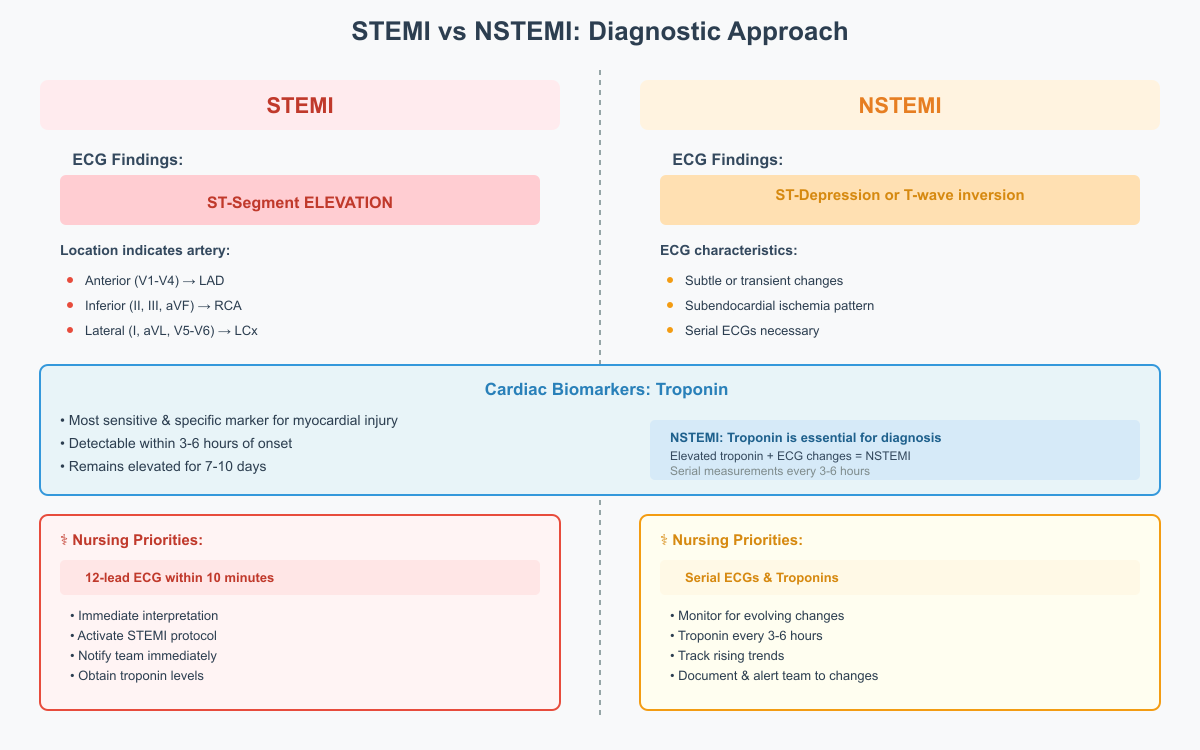
The electrocardiogram (ECG) is the cornerstone in the diagnostic approach for both STEMI and NSTEMI. Rapid and accurate interpretation of the ECG allows early identification of myocardial injury, guiding urgent interventions and influencing prognosis.
In STEMI patients, the hallmark ECG finding is ST-segment elevation, reflecting transmural myocardial infarction due to complete coronary artery occlusion. The location of the ST elevation often indicates which coronary artery is involved:
- Anterior STEMI → leads V1–V4 → left anterior descending artery
- Inferior STEMI → leads II, III, aVF → right coronary artery
- Lateral STEMI → leads I, aVL, V5–V6 → circumflex artery
Additional ECG findings may include hyperacute T waves, reciprocal ST depression in opposite leads, and eventual development of pathologic Q waves, signaling permanent heart muscle damage if reperfusion is delayed.
In NSTEMI patients, persistent ST-segment elevation is absent. Instead, the ECG may show:
- ST-segment depression
- T-wave inversion
- Non-specific changes indicating subendocardial myocardial injury
Because these changes can be subtle or transient, serial ECGs are recommended to detect evolving myocardial ischemia. Nurses play a critical role in obtaining a 12-lead ECG within 10 minutes of patient presentation, accurately documenting findings, and promptly notifying the healthcare team to initiate STEMI or NSTEMI protocols.
Example in Practice:
A 60-year-old man with acute chest pain has ST-segment elevation in V2–V5. Rapid ECG interpretation triggers immediate primary PCI, restoring blood flow to the heart muscle. A 70-year-old woman with intermittent chest discomfort shows T-wave inversion in lateral leads on serial ECGs, prompting NSTEMI management with antiplatelets, anticoagulation, and risk assessment.
Cardiac Biomarkers: Troponin and Other Laboratory Tests
Cardiac biomarkers are essential for confirming myocardial injury, particularly in NSTEMI, where ECG changes may be subtle. Troponin is the preferred biomarker due to its high sensitivity and specificity for myocardial cell injury.
- Troponin I and T:
- Detect myocardial injury within 3–6 hours of onset and may remain elevated for 7–10 days.
- Elevated troponin in NSTEMI confirms non-ST-segment elevation myocardial infarction, even in the absence of ST-segment elevation.
- In STEMI, troponin is also elevated but is supplemented by ECG findings to guide urgent reperfusion.
- Other Laboratory Tests:
- CK-MB (Creatine Kinase–Myocardial Band): Historically used but less sensitive than troponin.
- Myoglobin: Rises early but is non-specific.
- BNP or NT-proBNP: May be elevated in patients with concurrent acute heart failure, particularly after STEMI.
Nursing Implications:
- Serial measurement of troponin every 3–6 hours is critical for NSTEMI diagnosis and risk stratification.
- Nurses must ensure timely blood collection, document results, and alert the healthcare team to rising trends, as this can influence decisions regarding PCI or medical management.
Example in Practice:
A patient presents with mild chest pain and non-specific ECG changes. Initial troponin is normal but rises over six hours. Diagnosis of NSTEMI is confirmed, guiding initiation of antiplatelet therapy, anticoagulation, and close hemodynamic monitoring.
Universal Definition of Myocardial Infarction and Clinical Guidelines
The universal definition of myocardial infarction provides a standardized framework for diagnosing STEMI and NSTEMI, emphasizing clinical, ECG, and biomarker criteria. According to the Fourth Universal Definition of Myocardial Infarction:
- Diagnosis requires:
- A rise and/or fall of cardiac troponin with at least one value above the 99th percentile, and
- At least one of the following:
- Symptoms of ischemia (e.g., chest pain, dyspnea)
- New ST-segment or T-wave changes or new left bundle branch block on ECG
- Imaging evidence of new loss of viable myocardium or regional wall motion abnormality
- Identification of a coronary thrombus by angiography
- STEMI vs NSTEMI Classification:
- STEMI: Presence of persistent ST-segment elevation or new left bundle branch block.
- NSTEMI: Absence of ST elevation but with troponin elevation indicating subendocardial myocardial infarction.
Clinical Guidelines for Nurses:
- Nurses should integrate ECG findings, patient symptoms, and troponin levels when initiating the STEMI or NSTEMI care pathway.
- Guidelines from the American Heart Association (AHA) and European Society of Cardiology (ESC) recommend ECG within 10 minutes of hospital arrival, immediate reperfusion for STEMI, and risk-guided invasive or medical management for NSTEMI.
- Early recognition and adherence to these guidelines by nursing staff directly influence heart muscle salvage, prevention of complications, and short- and long-term outcomes.
Example in Practice:
A patient arrives with chest pain. ECG shows ST elevation in inferior leads, and troponin is elevated. Following the universal definition, STEMI is confirmed, and nurses initiate rapid primary PCI, administer aspirin and antiplatelet therapy, and monitor for arrhythmias or cardiogenic shock.
Management and Treatment Strategies
Immediate STEMI Treatment: Reperfusion and Medications
The management of STEMI patients is time-sensitive, with the primary goal being rapid reperfusion of the occluded coronary artery to restore blood flow to the heart muscle and minimize heart muscle damage. Immediate treatment typically involves a combination of reperfusion therapy and pharmacologic interventions.
Reperfusion Strategies:
- Primary Percutaneous Coronary Intervention (PCI):
- Considered the gold standard for STEMI management.
- PCI involves mechanically opening the occluded coronary artery using balloon angioplasty and stent placement.
- Recommended to be performed within 90 minutes of first medical contact (“door-to-balloon time”) to optimize heart muscle salvage.
- Thrombolytic Therapy:
- Used when PCI is not immediately available (e.g., rural hospitals without a cath lab).
- Medications such as tissue plasminogen activator (tPA) or reteplase dissolve the thrombus, restoring blood flow to the heart.
- Most effective when administered within 12 hours of symptom onset.
Adjunct Medications:
- Antiplatelets (Aspirin, P2Y12 inhibitors) to prevent further thrombus formation.
- Anticoagulants (heparin or low-molecular-weight heparin) to reduce propagation of the clot.
- Nitroglycerin for symptomatic relief of chest pain and reduction of myocardial oxygen demand.
- Beta-blockers and ACE inhibitors as indicated to reduce heart muscle workload and prevent heart failure.
Example in Practice:
A 58-year-old male presents with chest pain and ST-segment elevation in V2–V4. He is immediately prepared for primary PCI while receiving aspirin, heparin, and nitroglycerin. Rapid reperfusion restores blood flow to the heart muscle, minimizing infarct size and reducing the risk of acute heart failure.
NSTEMI Treatment: Medical and Invasive Approaches
NSTEMI patients typically experience partial coronary obstruction and subendocardial myocardial injury, making early risk assessment critical in guiding treatment. Management focuses on preventing progression, minimizing heart muscle damage, and reducing the risk of future heart attacks.
Medical Management:
- Antiplatelets (aspirin, clopidogrel, ticagrelor) to prevent thrombus growth.
- Anticoagulation (heparin or enoxaparin) to inhibit further clot formation.
- Beta-blockers to decrease myocardial oxygen demand and protect against arrhythmias.
- Statins for lipid lowering and plaque stabilization.
- Nitroglycerin for symptom relief, particularly in patients with ongoing angina.
Invasive Strategies:
- Early PCI is considered in high-risk NSTEMI patients, particularly those with elevated troponin levels, dynamic ECG changes, or significant coronary artery disease.
- Timing of intervention is often stratified:
- Immediate (<2 hours): Reserved for unstable patients or those with refractory chest pain.
- Early (within 24 hours): Standard for patients with moderate-to-high risk NSTEMI.
Example in Practice:
A 70-year-old female with diabetes and intermittent chest discomfort shows elevated troponin and ST depression on ECG. She is initiated on dual antiplatelet therapy, anticoagulation, and beta-blockers, followed by early PCI within 24 hours, preventing progression to transmural infarction.
Role of PCI, Thrombolytics, and Timing of Intervention
Percutaneous coronary intervention (PCI) and thrombolytic therapy are the primary interventions to restore blood flow to the heart muscle, with timing being critical to short- and long-term outcomes.
- PCI: Preferred for STEMI due to higher success rates in reperfusing the myocardium and lower risk of hemorrhagic complications. Also used in high-risk NSTEMI patients to improve prognosis and reduce recurrent events.
- Thrombolytics: Life-saving when PCI is not immediately available. Their effectiveness decreases significantly after 12 hours of symptom onset.
- Timing:
- Early intervention is directly linked to smaller infarct size, preservation of heart muscle function, and lower incidence of cardiogenic shock.
- For NSTEMI, timely invasive strategy reduces risk of recurrent myocardial infarction and improves long-term cardiovascular outcomes.
Nursing Role:
- Rapid identification of STEMI and NSTEMI using ECG and troponin levels.
- Preparing patients for PCI or thrombolysis, including consent, IV access, and monitoring.
- Administering adjunct medications and educating patients on symptom recognition and cardiac precautions.
Impact of Timely Reperfusion on Prognosis
Timely reperfusion has a profound effect on prognosis and outcomes for both STEMI and NSTEMI patients:
- Reduction in Heart Muscle Damage:
- The earlier blood flow is restored, the less myocardial injury occurs, preserving heart muscle function.
- Delayed reperfusion increases the risk of heart failure and cardiogenic shock.
- Improved Short- and Long-Term Outcomes:
- STEMI patients receiving primary PCI within guideline-recommended time frames have lower mortality rates and reduced risk of recurrent myocardial infarction.
- NSTEMI patients managed with early intervention and medical therapy experience improved long-term cardiovascular prognosis and reduced hospital readmissions.
- Prevention of Complications:
- Timely reperfusion limits arrhythmias, ventricular remodeling, and extensive myocardial infarction, improving overall cardiac function.
Example in Practice:
A 62-year-old man with ST-segment elevation in inferior leads receives primary PCI within 80 minutes of hospital arrival, preserving ventricular function and preventing acute heart failure. Conversely, delayed intervention in NSTEMI can lead to progression to full-thickness myocardial infarction, highlighting the importance of rapid risk assessment and timely management.
Complications and Prognosis
STEMI Complications: Cardiogenic Shock and Heart Failure
STEMI patients are at higher risk of severe complications due to the transmural myocardial injury that occurs when a coronary artery is completely occluded. Two of the most serious complications are cardiogenic shock and heart failure.
Cardiogenic Shock:
- Defined as a state of inadequate tissue perfusion due to extensive heart muscle damage.
- Occurs in approximately 5–10% of STEMI cases and is associated with high mortality.
- Pathophysiology involves massive loss of contractile function, reduced cardiac output, and systemic hypoperfusion.
- Clinical signs include hypotension, tachycardia, cold extremities, oliguria, altered mental status, and persistent chest pain.
Nursing Considerations:
- Continuous hemodynamic monitoring is essential.
- Early recognition and rapid intervention with inotropes, vasopressors, and mechanical support (e.g., intra-aortic balloon pump) can improve outcomes.
- STEMI patients with cardiogenic shock often require urgent reperfusion via PCI or coronary artery bypass graft (CABG).
Heart Failure:
- STEMI can lead to acute heart failure due to loss of functional heart muscle, especially with large anterior infarctions.
- Symptoms include dyspnea, pulmonary congestion, edema, fatigue, and decreased exercise tolerance.
- Risk is higher in patients with delayed reperfusion, older age, prior myocardial infarction, or extensive coronary artery disease.
Example in Practice:
A 60-year-old male with anterior STEMI develops hypotension and pulmonary edema within hours of hospital arrival. Nurses initiate continuous ECG and hemodynamic monitoring, administer inotropes, and prepare the patient for emergent PCI, preventing further heart muscle damage.
NSTEMI Long-Term Cardiovascular Risks
While NSTEMI patients often present with less dramatic acute symptoms, they face significant long-term cardiovascular risks due to subendocardial myocardial injury and ongoing coronary artery disease.
Long-Term Risks Include:
- Recurrent Myocardial Infarction:
- Partial obstruction or unstable plaques may progress to complete occlusion, causing subsequent STEMI or NSTEMI events.
- Chronic Heart Failure:
- Even limited myocardial injury can impair ventricular function over time, particularly in patients with comorbidities such as hypertension or diabetes.
- Arrhythmias:
- Fibrotic changes in the heart muscle may predispose patients to ventricular tachycardia or atrial fibrillation.
- Increased Mortality:
- Studies indicate that patients with NSTEMI have a higher risk of long-term cardiovascular mortality if not adequately managed with risk-guided interventions and secondary prevention.
Nursing Implications:
- Education on lifestyle modifications, medication adherence, and symptom monitoring is critical.
- Regular follow-up, ECG monitoring, and management of risk factors such as hyperlipidemia and hypertension reduce long-term complications.
Example in Practice:
A 68-year-old female with NSTEMI undergoes early PCI and medical therapy. She is discharged with dual antiplatelet therapy, statins, and beta-blockers, and receives structured patient education on exercise, diet, and early recognition of chest pain, reducing her risk of future myocardial infarction.
Comparing Mortality, Recovery, and Heart Muscle Damage
The severity of myocardial injury largely dictates mortality, recovery, and long-term prognosis in STEMI and NSTEMI.
Mortality:
- STEMI patients have higher short-term mortality, primarily due to cardiogenic shock, arrhythmias, and extensive heart muscle damage.
- NSTEMI patients generally have lower initial mortality but may have comparable long-term mortality if underlying coronary artery disease is not addressed.
Recovery:
- STEMI: Recovery depends on the extent of transmural myocardial infarction and timeliness of reperfusion therapy. Patients with successful early PCI may regain significant heart muscle function and avoid severe complications.
- NSTEMI: Recovery is typically faster due to subendocardial involvement, but patients require careful long-term monitoring to prevent recurrent events.
Heart Muscle Damage:
- STEMI: Full-thickness injury can result in ventricular remodeling, reduced ejection fraction, and chronic heart failure.
- NSTEMI: Partial-thickness injury preserves more heart muscle, but repeated episodes can lead to cumulative damage and progressive cardiovascular decline.
Example in Practice:
A 55-year-old male STEMI patient undergoes primary PCI within 90 minutes. Post-procedure, he shows mild left ventricular dysfunction but avoids heart failure, highlighting the impact of timely intervention. A 72-year-old NSTEMI patient with delayed PCI experiences subtle ventricular impairment over months, emphasizing the need for secondary prevention and lifestyle modifications.
Nursing Care and Patient Education
Monitoring, ECG Assessment, and Early Recognition for Nurses
Nursing care for STEMI and NSTEMI patients begins with continuous monitoring and early recognition of myocardial ischemia or evolving infarction. Nurses are often the first to identify subtle changes in a patient’s condition, making their role crucial for reducing heart muscle damage and improving prognosis.
Key Nursing Responsibilities Include:
- Vital Signs and Hemodynamic Monitoring:
- Monitor blood pressure, heart rate, oxygen saturation, and respiratory status continuously.
- Early detection of hypotension, tachyarrhythmias, or signs of cardiogenic shock allows rapid intervention.
- ECG Assessment:
- Obtain a 12-lead ECG within 10 minutes of presentation in all patients with suspected acute coronary syndrome.
- Monitor for ST-segment elevation, ST depression, T-wave inversion, or new bundle branch blocks, as these indicate STEMI or NSTEMI.
- Serial ECGs are critical for NSTEMI patients due to transient or subtle changes.
- Symptom Assessment:
- Frequent evaluation of chest pain, dyspnea, diaphoresis, and fatigue.
- Document onset, duration, intensity, and associated symptoms to guide diagnostic and treatment decisions.
Example in Practice:
A nurse in the cardiac unit continuously monitors a 65-year-old male presenting with chest pain. Serial ECGs reveal progressive ST-segment elevation in V2–V5, prompting immediate notification of the cardiology team for primary PCI. Early recognition prevents extensive heart muscle damage.
Nursing Interventions: Supporting STEMI and NSTEMI Patients
Effective nursing interventions aim to stabilize patients, minimize complications, and support recovery in both STEMI and NSTEMI.
For STEMI Patients:
- Preparation for Reperfusion Therapy: Ensure IV access, administer antiplatelets and anticoagulants, and assist with primary PCI or thrombolytic therapy.
- Continuous Cardiac Monitoring: Watch for arrhythmias, ST-segment changes, or signs of cardiogenic shock.
- Symptom Management: Provide oxygen if hypoxemic, administer nitroglycerin for chest pain, and manage anxiety to reduce cardiac workload.
- Post-PCI Care: Monitor for bleeding at catheter site, maintain strict hemodynamic observation, and ensure patient is educated about activity restrictions and medications.
For NSTEMI Patients:
- Medical Management Support: Administer dual antiplatelet therapy, anticoagulation, beta-blockers, and statins according to protocol.
- Risk Assessment: Utilize tools to stratify patients for early invasive strategies or delayed PCI.
- Monitoring for Progression: Watch for worsening chest pain, arrhythmias, or hemodynamic instability, which may indicate evolving STEMI.
- Education During Hospital Stay: Teach patients about lifestyle modifications, medication adherence, and symptom recognition to reduce recurrence.
Example in Practice:
A 72-year-old female with NSTEMI is managed with anticoagulation and early PCI. Nursing care includes frequent ECG checks, troponin monitoring, and patient education on recognizing chest discomfort and preventing complications.
Educating Patients on Recurrent Chest Pain and Prevention of Future Heart Attacks
Patient education is a critical component of nursing care for STEMI and NSTEMI patients, aiming to prevent recurrent myocardial infarction and improve long-term cardiovascular outcomes.
Key Education Topics:
- Recognizing Recurrent Chest Pain:
- Teach patients to identify angina-like pain, shortness of breath, fatigue, or atypical symptoms.
- Stress the importance of seeking immediate medical attention if symptoms recur.
- Medication Adherence:
- Explain the purpose of antiplatelets, statins, beta-blockers, and ACE inhibitors.
- Emphasize adherence to prescribed doses and timing, as it directly impacts heart muscle preservation and prevention of future infarctions.
- Lifestyle Modifications:
- Encourage smoking cessation, heart-healthy diet, regular physical activity, and weight management.
- Control of hypertension, diabetes, and hyperlipidemia to reduce coronary artery disease progression.
- Secondary Prevention and Follow-Up:
- Advise on regular cardiac check-ups, stress testing, and ECG monitoring.
- Discuss the role of cardiac rehabilitation programs in improving functional capacity and prognosis.
Example in Practice:
A 65-year-old male discharged after STEMI attends a nursing-led education session. He learns to monitor for chest pain, adhere to dual antiplatelet therapy, and incorporate dietary and exercise modifications, significantly reducing the risk of future heart attacks.
Conclusion
Understanding the differences between STEMI and NSTEMI is essential for nurses, cardiologists, and other healthcare professionals managing acute myocardial infarction patients. While both represent forms of acute coronary syndrome, they differ fundamentally in pathophysiology, ECG findings, extent of myocardial injury, and urgency of treatment. STEMI patients typically experience complete coronary artery occlusion, resulting in transmural infarction and requiring immediate reperfusion through primary PCI or thrombolytic therapy. In contrast, NSTEMI patients experience partial occlusion and subendocardial myocardial injury, often necessitating risk-guided medical therapy and early invasive strategies.
Nursing care plays a pivotal role in both scenarios. Nurses are at the forefront of early recognition, continuous ECG and hemodynamic monitoring, and administration of life-saving medications. Timely interventions and diligent monitoring significantly influence short- and long-term outcomes, including heart muscle preservation, prevention of cardiogenic shock and heart failure, and reduction in mortality. Moreover, patient education on symptom recognition, medication adherence, lifestyle modification, and secondary prevention empowers patients to reduce the risk of recurrent myocardial infarction and improve overall cardiovascular health.
Ultimately, effective management of STEMI and NSTEMI is not solely about interventions in the acute setting—it is a continuum of care that integrates rapid diagnosis, evidence-based treatment, vigilant nursing care, and patient-centered education. By mastering these principles, nurses contribute directly to optimizing prognosis, reducing complications, and enhancing quality of life for patients with acute myocardial infarction. Understanding these distinctions allows healthcare professionals to respond with precision, ensuring that each patient receives the right care at the right time and that the heart muscle and overall cardiovascular function are preserved as much as possible.
Frequently Asked Questions
What is the difference between NSTEMI and STEMI?
The main difference lies in the extent of myocardial injury and ECG changes. STEMI (ST-segment elevation myocardial infarction) involves complete coronary artery occlusion, leading to transmural myocardial infarction and ST-segment elevation on the ECG. NSTEMI (non-ST-segment elevation myocardial infarction) is caused by partial coronary artery blockage, resulting in subendocardial injury and ST-segment depression or T-wave inversion, without full-thickness infarction.
Is an NSTEMI a heart attack?
Yes. An NSTEMI is a type of heart attack. Although the damage is usually less extensive than a STEMI, it still involves myocardial injury due to reduced blood flow to the heart muscle, confirmed by elevated troponin levels.
Is a STEMI heart attack a widowmaker?
Not all STEMI heart attacks are “widowmakers,” but STEMIs affecting the left anterior descending artery (LAD) are sometimes called widowmakers because they can cause massive anterior myocardial infarction and high mortality if untreated promptly. STEMIs in other coronary arteries are serious but may carry lower immediate risk.
How to identify STEMI and NSTEMI?
Identification relies on a combination of ECG, cardiac biomarkers, and clinical symptoms:
- STEMI: ST-segment elevation on ECG, elevated troponin, and classic chest pain or acute coronary syndrome symptoms.
- NSTEMI: No ST-segment elevation; may show ST depression or T-wave inversion, elevated troponin, and chest pain or discomfort, often subtler than STEMI.
- Nursing assessment and timely ECG within 10 minutes are crucial for early identification and intervention.
