Dorsal Recumbent Position: Essential Guide to Patient Positioning, Recumbent Positions, and Lithotomy Position Uses
Patient positioning is a fundamental aspect of nursing care, playing a crucial role in both patient safety and the effectiveness of medical procedures. Among the various positions utilized in clinical practice, the dorsal recumbent position is particularly notable for its versatility and accessibility during medical examinations. Far from being a simple matter of where a patient lies, understanding the dorsal recumbent position involves appreciating anatomical alignment, functional benefits, and the implications for procedural efficiency and patient comfort. In practice, this position provides nurses and clinicians with a stable and controlled framework for conducting assessments and interventions while minimizing risks associated with improper positioning.
The study of recumbent positions extends beyond the dorsal recumbent posture, encompassing lateral, prone, decubitus, and functional variations that are frequently employed across different medical settings. Each of these positions offers specific advantages depending on the patient’s condition, the type of medical examination, or the procedural requirements. By understanding the distinctions among these positions and the principles guiding their use, nursing staff can ensure that patient care is both safe and effective.
This guide examines the dorsal recumbent position in depth, highlighting its definition, key anatomical considerations, and functional applications. It also situates the position within the broader context of patient positioning, discussing related recumbent and functional positions, and comparing the dorsal recumbent posture to alternatives such as lithotomy, Sims, and knee-chest positions. The discussion emphasizes practical considerations for implementing the position safely, adjusting for patient comfort, and optimizing outcomes during medical examinations and procedures.
By integrating evidence-based practices and clinical insights, nurses can enhance patient care through informed positioning strategies. Understanding when and how to use the dorsal recumbent position—and recognizing its benefits relative to other recumbent positions—is essential for providing high-quality care, improving patient comfort, and supporting procedural efficiency in diverse healthcare environments. This article provides a comprehensive exploration of these concepts, offering guidance that is applicable to both novice and experienced nursing professionals.
By integrating evidence-based practices and clinical insights, nurses can enhance patient care through informed positioning strategies. Understanding when and how to use the dorsal recumbent position—and recognizing its benefits relative to other recumbent positions—is essential for providing high-quality care, improving patient comfort, and supporting procedural efficiency in diverse healthcare environments. This article provides a comprehensive exploration of these concepts, offering guidance that is applicable to both novice and experienced nursing professionals.
Understanding the Dorsal Recumbent Position
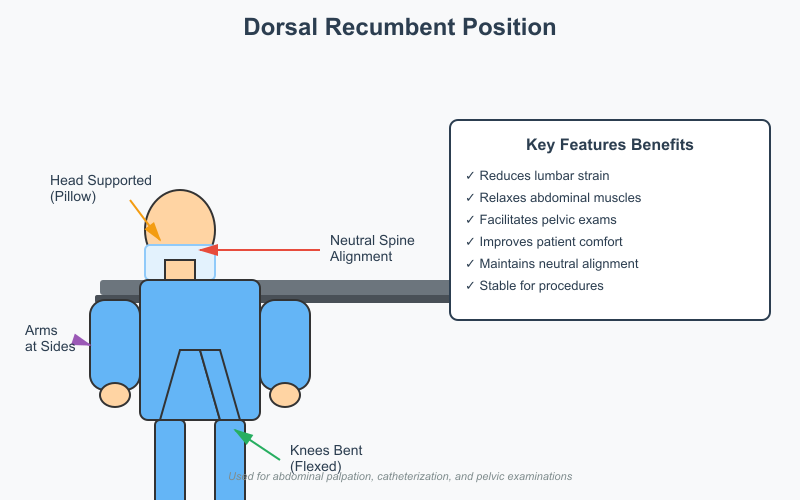
Definition and Key Features
The dorsal recumbent position is a commonly used patient positioning technique in nursing and medical care. It is defined as a lying position where the patient lies flat on their back, with the head, neck, and spine in a neutral alignment. The knees are typically bent, and feet are placed flat on the examination surface. This arrangement provides both patient comfort and safety while allowing clinicians optimal access for medical assessments.
Key anatomical and functional features of this position include:
- Spinal Alignment:
- The spine remains in a neutral, supported posture.
- Reduces lumbar strain compared to lying fully supine.
- Knee Flexion:
- Slightly bent knees relax abdominal muscles.
- Facilitates abdominal and pelvic examinations.
- Head and Neck Position:
- Head may be supported with a pillow to maintain neutral cervical alignment.
- Prevents neck hyperextension during prolonged procedures.
- Arm Placement:
- Arms are usually positioned comfortably at the sides or across the abdomen.
- Prevents nerve compression and allows for unobstructed access to the torso.
Comparison to Other Positions:
| Position | Patient Alignment | Clinical Considerations |
|---|---|---|
| Supine | Lying flat with legs extended | Suitable for general exams but may strain the lower back if prolonged |
| Anatomical | Upright, standing, arms at sides | Standard reference for anatomical orientation; not used for procedures |
| Dorsal Recumbent | Lying on back, knees bent | Reduces lumbar tension, facilitates abdominal/pelvic access, improves patient comfort |
Functional Benefits in Medical Care:
- Facilitates minor procedures and routine examinations (e.g., catheterization, abdominal palpation, pelvic assessment).
- Supports patient relaxation, particularly for those with back pain or mobility limitations.
- Provides stable positioning that minimizes movement during sensitive medical assessments.
Clinical Advantages of the Dorsal Recumbent Position
The dorsal recumbent position is preferred in medical settings due to a combination of procedural efficiency, patient safety, and comfort. Its clinical advantages include:
- Enhanced Access for Medical Examinations:
- Provides optimal exposure of the anterior body surface.
- Used for assessments of the abdomen, pelvic region, and genitourinary system.
- Allows clinicians to perform inspections, palpation, and minor interventions without repeatedly repositioning the patient.
- Patient Safety and Comfort:
- Reduces stress on the lumbar spine by bending the knees.
- Minimizes the risk of falls or injury during examinations.
- Supports comfort for patients experiencing fatigue, pain, or post-surgical limitations.
- Procedural Efficiency:
- Streamlines nursing care by reducing the need for additional adjustments.
- Accommodates the use of supportive devices such as pillows or rolled towels to maintain posture.
- Useful during short or prolonged procedures, ensuring patient stability throughout.
- Adaptability Across Patient Populations:
- Can be modified for patients with limited mobility, obesity, or postpartum needs.
- Compatible with other positioning techniques when combined with supportive interventions (e.g., semi-sitting, slight Trendelenburg adjustments).
Example in Practice:
- During urinary catheterization, placing a patient in the dorsal recumbent position allows the nurse to maintain proper alignment of the pelvis while ensuring the patient’s knees are comfortably bent.
- For abdominal assessments, the flexed knees relax the abdominal wall, allowing for more accurate palpation and reducing patient discomfort.
Overview of Recumbent and Related Positions
Types of Recumbent Positions
Recumbent positions are a group of patient positioning techniques in which the patient lies in a horizontal or semi-horizontal posture. These positions are widely used in nursing and medical care to optimize patient comfort, facilitate medical examinations, and support specific clinical procedures. Understanding the distinct types of recumbent positions is essential for safe and effective nursing practice.
- Lateral Recumbent Position
- In the lateral recumbent position, the patient lies on their side, typically with one arm extended for support and the legs slightly flexed.
- Clinical use: Often used to facilitate airway clearance, especially in patients who are vomiting or at risk of aspiration. It is also common in post-surgical recovery to relieve pressure on certain body areas.
- Nursing considerations: Ensure the spine remains aligned and a pillow supports the head and between the knees to maintain comfort and prevent musculoskeletal strain.
- Left Lateral Recumbent Position
- A variation of the lateral recumbent position where the patient specifically lies on the left side.
- Clinical use: Frequently used in cardiac or obstetric assessments, as it may improve venous return and reduce pressure on the inferior vena cava in pregnant patients.
- Nursing considerations: Support under the torso and between the knees is essential to prevent discomfort during prolonged positioning.
- Prone Position
- The prone position involves the patient lying face down on the abdomen, with the head turned to one side.
- Clinical use: Commonly used for procedures that require posterior access, such as back wound care, certain surgical procedures, and respiratory therapy in patients with acute respiratory distress syndrome (ARDS).
- Nursing considerations: Avoid excessive neck rotation; ensure proper support for the chest, pelvis, and lower extremities to prevent pressure injuries.
- Decubitus Position
- In the decubitus position, the patient lies on the side with the body fully extended. This is a variant of the lateral position often used for imaging studies, such as chest X-rays, to allow specific diagnostic angles.
- Clinical use: Frequently used in radiology or for pressure relief in immobile patients.
- Nursing considerations: Proper padding under bony prominences is necessary to maintain patient comfort and safety.
- Neutral Position
- In the neutral position, the patient lies flat on the back without flexion or extension of the joints, maintaining a natural spinal alignment.
- Clinical use: Often used during routine medical examinations or when transferring patients to beds or stretchers.
- Nursing considerations: Supports musculoskeletal stability and is useful as a baseline position before transitioning to other functional or procedural positions.
- Fetal Position
- In the fetal position, the patient lies on their side with knees drawn toward the chest and arms flexed around the head or torso.
- Clinical use: Used for comfort in patients with abdominal pain, during certain lumbar procedures, or to reduce intracranial pressure in neurological care.
- Nursing considerations: Ensure support with pillows along the spine and under the head to maintain alignment and prevent pressure injuries.
Functional and Anatomical Variations
Understanding the variations of functional and anatomical positions is crucial in nursing care, as these adaptations allow for both procedural efficiency and patient-centered comfort.
- Functional Position
- This position focuses on patient comfort and procedural accessibility, often incorporating slight flexion or elevation of limbs.
- Clinical use: Ideal for patients recovering from surgery or for those with limited mobility, as it reduces strain while allowing safe performance of medical examinations.
- Neutral Position
- Emphasizes maintaining the natural alignment of the spine and joints without additional flexion or extension.
- Clinical use: Serves as a baseline for transitioning patients into other positions or for short-term assessments.
- Anatomical Position
- The anatomical position is a standardized reference where the patient stands upright with arms at the sides and palms facing forward.
- Clinical use: Used primarily as a reference in medical documentation, anatomical studies, and descriptions of body structures.
- Reclining and Tripod Adjustments
- The reclining position involves tilting the patient back at varying degrees to reduce pressure on the spine or support respiratory effort.
- The tripod position involves the patient sitting upright, leaning slightly forward with hands or arms supported on a table or bed.
- Clinical use: Both positions are useful for patients with respiratory difficulties, such as chronic obstructive pulmonary disease (COPD), and provide enhanced breathing comfort during examinations.
- Orthopneic or Upright Positions
- Involves placing the patient in a semi-sitting or fully sitting position to optimize lung expansion.
- Clinical use: Often employed in critical care or during medical procedures requiring maximal ventilation.
Practical Example in Nursing Practice:
A patient recovering from abdominal surgery may start in a neutral position during initial rest, then transition to a dorsal recumbent position for wound assessment, and finally adjust into a tripod position to facilitate coughing and deep breathing exercises. By understanding these recumbent and related positions, nurses can enhance patient comfort, reduce risks of pressure injuries, and improve procedural efficiency.

Medical Examinations and Procedures Using the Dorsal Recumbent Position
The dorsal recumbent position is a cornerstone in patient positioning for a wide range of medical examinations and minor procedures. Its use combines patient comfort, safety, and clinical accessibility, making it an essential position in nursing and healthcare practice.
Common Clinical Applications
The dorsal recumbent position is frequently employed in situations where examination or procedural access to the anterior body surface is required. Key applications include:
- Abdominal Examinations
- The patient lies on their back with knees slightly flexed.
- Clinical use: Facilitates palpation, auscultation, and percussion of abdominal organs.
- Nursing considerations: Ensure pillows or rolled towels support the head and knees to reduce lumbar strain and maximize comfort.
- Example: During a routine abdominal assessment, flexing the knees relaxes the abdominal muscles, allowing for more accurate palpation of the liver, spleen, and intestines.
- Pelvic Examinations
- Common in gynecological assessments, including Pap smears and vaginal examinations.
- Position used: Knees bent and feet placed flat on the table, ensuring stability while allowing clinician access.
- Nursing considerations: Maintain patient privacy with drapes and provide verbal explanations to reduce anxiety.
- Genitourinary Procedures
- Examples include catheterization and urinary specimen collection.
- Advantages of dorsal recumbent position: Provides proper alignment of the pelvis and reduces patient strain, particularly in those with limited mobility.
- Example: In female catheterization, this position allows for easier visualization and insertion while maintaining patient comfort and safety.
- Minor Surgical and Diagnostic Procedures
- Small wound care, abdominal drainage, or suture removal procedures can be safely performed in this position.
- Nursing considerations: Support the patient’s head and extremities to prevent discomfort during procedures that may take longer than routine examinations.
Comparison with Other Positions
Understanding the differences between the dorsal recumbent position and other commonly used positions is critical for effective nursing practice. Each position has distinct indications, advantages, and limitations:
| Position | Indications | Advantages | Limitations |
|---|---|---|---|
| Dorsal Recumbent Position | Abdominal, pelvic, and genitourinary exams; minor procedures | Reduces lumbar strain; facilitates anterior access; comfortable for patient; stable for short-term procedures | Limited posterior access; less effective for extensive gynecological procedures compared to lithotomy |
| Lithotomy Position | Gynecological surgeries, childbirth, extensive pelvic procedures | Provides maximum exposure of pelvic region; ideal for surgical interventions | Less comfortable; higher risk of musculoskeletal strain; requires careful support of legs and lower back |
| Sims’ Position | Rectal examinations, enemas, certain vaginal exams | Facilitates access to posterior pelvic area; useful for drainage procedures | Less suitable for abdominal exams; requires side-lying coordination |
| Knee-Chest Position | Rectal examinations, proctologic procedures, certain spinal procedures | Provides optimal posterior access; allows deep palpation or instrumentation | Can be uncomfortable; not suitable for patients with limited mobility or cardiovascular compromise |
Key Nursing Considerations:
- The dorsal recumbent position is ideal for procedures requiring access to the anterior body without placing strain on the patient.
- Compared to the lithotomy position, it offers superior patient comfort, making it preferable for routine or short-duration procedures.
- While Sims’ and knee-chest positions allow access to posterior structures, they are less versatile and can be uncomfortable for prolonged use.
- Nursing staff must always ensure proper patient positioning, including support of the head, knees, and arms, and monitor for pressure points or signs of discomfort.
Example in Practice:
- A patient undergoing a urinary catheterization benefits from the dorsal recumbent position for proper pelvic alignment and minimal strain.
- If a patient requires a more extensive pelvic procedure, the lithotomy position may be selected instead, with the nurse ensuring proper leg support and monitoring patient safety throughout.
Proper Patient Positioning Techniques for Safety and Comfort
Effective patient positioning is essential in nursing care to ensure patient safety and comfort, facilitate medical examinations, and optimize procedural outcomes. The dorsal recumbent position is particularly versatile, but proper technique and adjustments are required to maximize its benefits and minimize risks.
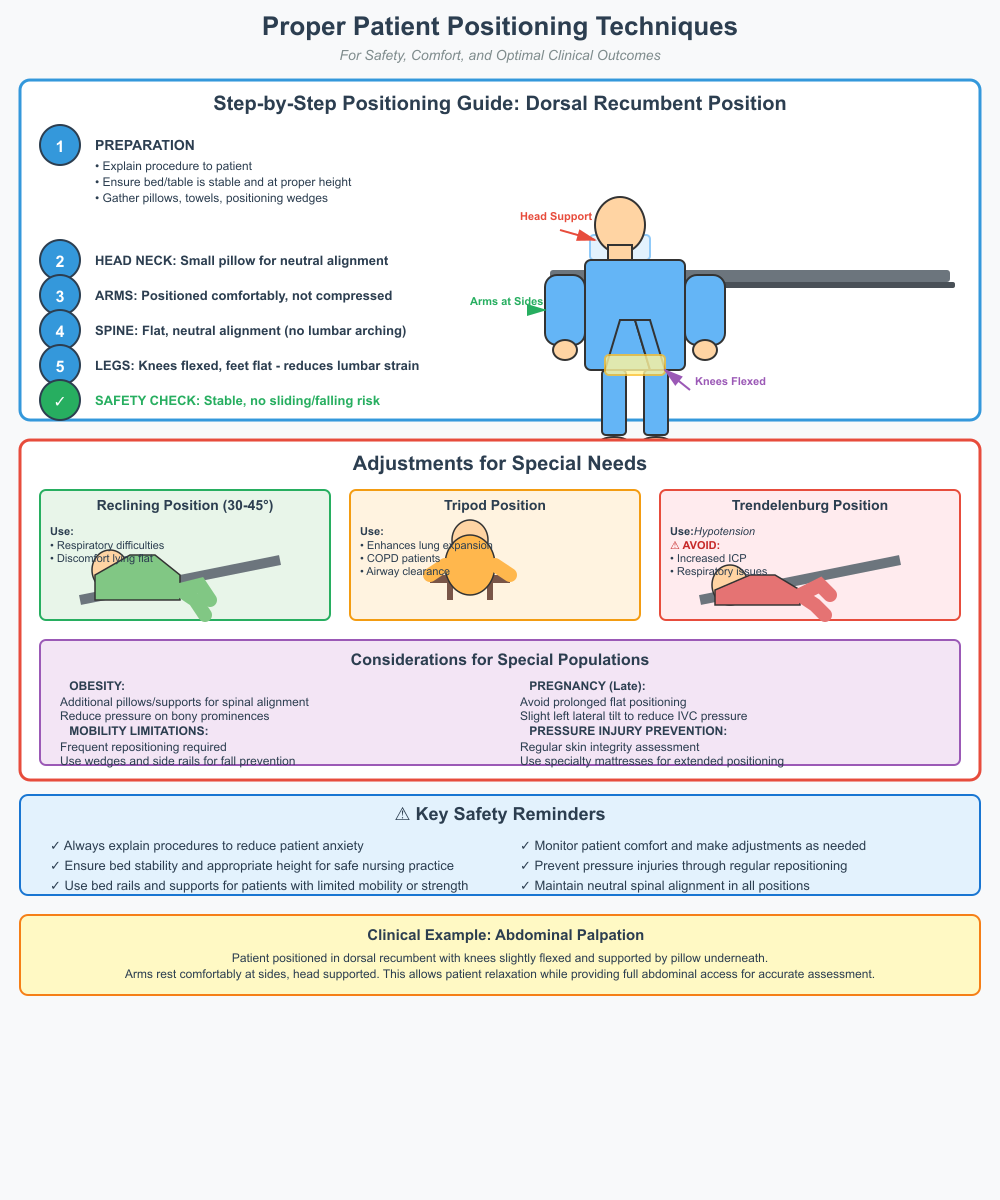
Step-by-Step Positioning Guide
Placing a patient in the dorsal recumbent position involves careful attention to spinal alignment, joint support, and overall comfort. A structured approach ensures safety and reduces the risk of musculoskeletal strain or pressure injuries.
- Preparation
- Explain the procedure to the patient to reduce anxiety.
- Ensure the bed or examination table is stable and at an appropriate height for safe nursing practice.
- Gather supportive devices such as pillows, rolled towels, and positioning wedges.
- Positioning the Patient
- Head and Neck: Place a small pillow under the head to maintain neutral cervical alignment and prevent neck hyperextension.
- Arms: Position the arms comfortably at the sides or across the abdomen, ensuring they are not compressed. If necessary, place a pillow under the arms for additional support.
- Spinal Alignment: Ensure the patient lies flat on the back with the spine in a neutral, straight alignment. Avoid excessive arching of the lumbar region.
- Legs and Feet: Flex the knees slightly and place the feet flat on the bed. This reduces lumbar strain and relaxes the abdominal muscles, which is critical for abdominal and pelvic assessments.
- Safety Check: Confirm that the patient is stable, with no risk of sliding or falling from the bed or table.
- Final Adjustments
- Use additional pillows under the knees or along the back if the patient experiences discomfort.
- Adjust the bed rails or provide side supports for added security, particularly for patients with limited mobility or impaired strength.
Example in Practice:
A nurse preparing a patient for abdominal palpation will place the patient in the dorsal recumbent position, flexing the knees slightly with a pillow underneath, arms comfortably at the sides, and the head supported. This allows the patient to relax while providing the nurse full access to the abdominal area for accurate assessment.
Adjustments for Special Needs
Certain patient conditions require modifications to the standard dorsal recumbent position to ensure comfort, safety, and procedural efficiency.
- Reclining Position
- Slight elevation of the head and upper torso, typically at a 30–45° angle.
- Clinical use: Supports patients with respiratory difficulties or those experiencing discomfort in a fully flat position.
- Nursing consideration: Ensure proper lumbar support and avoid excessive bending at the hips, which may strain the lower back.
- Tripod Position
- Patient sits upright with hands or arms supported on a table or surface in front.
- Clinical use: Enhances lung expansion and airway clearance for patients with respiratory conditions such as chronic obstructive pulmonary disease (COPD).
- Nursing consideration: Adjust support height to prevent shoulder fatigue and maintain patient comfort.
- Trendelenburg Position
- The head is lower than the feet, tilting the body in a reverse recline.
- Clinical use: Sometimes used to improve venous return in patients with hypotension or during certain surgical procedures.
- Nursing consideration: Avoid in patients with increased intracranial pressure, respiratory compromise, or obesity. Continuous monitoring is essential to maintain patient safety.
- Considerations for Special Populations
- Obesity: Use additional pillows or adjustable supports to maintain spinal alignment and reduce pressure on bony prominences.
- Pregnancy: Avoid prolonged flat positioning in late pregnancy; slight left lateral tilt may be necessary to reduce pressure on the inferior vena cava.
- Mobility Limitations: Patients with restricted mobility may require frequent repositioning, supportive wedges, or side rails to prevent falls and pressure injuries.
- Pressure Injury Prevention: Regularly assess skin integrity and redistribute weight using cushions or specialty mattresses when patients remain in the dorsal recumbent position for extended periods.
Example in Practice:
During urinary catheterization for an elderly patient with limited mobility, the nurse may slightly recline the patient while maintaining knee flexion and head support. Pillows are placed under the knees and along the back to ensure patient comfort and safety, reducing the risk of musculoskeletal strain or pressure injury.
Key Nursing Principles for Safe Positioning
- Always maintain neutral spinal alignment and support joints appropriately.
- Continuously monitor the patient for signs of discomfort, pressure points, or impaired circulation.
- Combine the dorsal recumbent position with other supportive postures (reclined, tripod, Trendelenburg) based on the patient’s condition and procedural requirements.
- Document the positioning technique and any adjustments made for accountability and continuity of care.
Comparing Dorsal Recumbent Position to Other Positions
In nursing care and medical settings, understanding how the dorsal recumbent position compares to other patient positions is crucial for ensuring patient comfort and safety while providing effective procedural access. Different positions serve specific clinical purposes, and the choice of position used depends on the type of medical examination, the patient’s condition, and the procedure being performed.
Lithotomy and Related Positions
The lithotomy position involves the patient being placed on their back with hips and knees flexed, thighs abducted, and feet supported in stirrups or leg holders. This position is frequently used in medical settings for gynecological procedures, childbirth, and certain urological interventions.
Comparison with Dorsal Recumbent Position:
Body Alignment: The dorsal recumbent position involves the patient lying on the back with knees slightly flexed, whereas the lithotomy position requires sharp flexion of the hips and thighs.
Procedural Access: The lithotomy position provides maximal access to the pelvic area for surgical interventions, while the dorsal recumbent position is particularly useful for routine examinations and minor procedures.
Patient Comfort and Safety: The dorsal recumbent position is generally more comfortable and stable, reducing strain on the lower back and joints. In contrast, the lithotomy position can be uncomfortable if maintained for extended periods, requiring careful support and monitoring to maintain patient safety and comfort.
Example in Practice: A patient undergoing a routine pelvic exam is placed in the dorsal recumbent position, which allows them to relax while providing the nurse adequate access. For a more invasive gynecological procedure, the lithotomy position is used, with proper support for the legs and close observation to prevent pressure injuries.
Sims, Jackknife, and Knee-Chest Positions
The dorsal recumbent position complements or substitutes other positions depending on the type of procedure and the patient’s comfort and safety.
- Sims’ Position
- Patient lies on the left side with the lower arm behind the back, the upper leg flexed, and the upper arm supported.
- Uses in medical procedures: Rectal exams, enemas, and certain vaginal procedures.
- Limitations: Less accessible for anterior procedures.
- Relation to Dorsal Recumbent Position: The nurse may transition the patient from dorsal recumbent position to Sims’ position for sequential assessments, maintaining proper patient positioning throughout.
- Jackknife Position
- Patient lies prone with hips flexed and buttocks elevated.
- Uses: Proctological procedures, spinal surgeries.
- Limitations: Can cause discomfort and strain, requiring continuous monitoring.
- Integration: The dorsal recumbent position is often used before or after the jackknife position to allow the patient to rest comfortably on the back.
- Knee-Chest Position
- Patient is placed on the knees and chest with hips elevated.
- Uses: Rectal exams and procedures requiring posterior pelvic access.
- Limitations: Not suitable for patients with limited mobility, respiratory compromise, or cardiovascular issues.
- Relation to Dorsal Recumbent Position: The dorsal recumbent position may serve as a preparatory or resting position, ensuring patient comfort and safety before assuming the knee-chest posture.
- Left Lateral Recumbent Position
- Patient lies on the left side with knees slightly flexed.
- Uses: Cardiac assessments, post-operative drainage, and respiratory support.
- Relation: This position is used when the dorsal recumbent position is less suitable, such as when minimizing aspiration risk or providing comfort in certain medical conditions.
- Orthopneic Position
- Semi-sitting with arms supported on a table or pillow.
- Uses: Enhances respiratory effort in patients with COPD or dyspnea.
- Relation: Offers an alternative to the dorsal recumbent position when patient comfort and safety require a semi-upright or tripod position adjustment.
Example in Practice: A patient may begin in the dorsal recumbent position for an abdominal assessment and then transition to Sims’ or knee-chest positions for rectal evaluation. This ensures sequential procedural access while maintaining patient comfort and safety.
Considerations for Patient Positioning
Selecting the appropriate position involves careful nursing assessment of:
- Type of Examination or Procedure
- Abdominal or minor pelvic procedures → Dorsal recumbent position is particularly useful.
- Extensive gynecological procedures → Lithotomy position.
- Posterior access → Sims, jackknife, or knee-chest positions.
- Patient Condition
- Respiratory compromise → Orthopneic or tripod adjustments.
- Late-stage pregnancy → Avoid supine; consider left lateral recumbent position.
- Limited mobility or obesity → Use pillows, wedges, and supportive devices to maintain proper patient positioning.
- Patient Safety and Comfort
- Support the head, neck, arms, and knees.
- Monitor for pressure points and circulation compromise.
- Reposition periodically when the position is used for prolonged procedures.
- Clinical Efficiency
- Use the dorsal recumbent position when feasible to minimize repositioning.
- Combine with reclining, tripod, or semi-sitting adjustments as needed to enhance procedural access and patient comfort.
Benefits of the Dorsal Recumbent and Recumbent Positions in Nursing Care
The dorsal recumbent position and other recumbent positions are essential tools in nursing care and patient positioning, providing both clinical and practical advantages. Their use extends beyond simple comfort, supporting patient safety, facilitating medical procedures, and optimizing workflow in various medical settings. Understanding the benefits of the recumbent position allows nurses to deliver more effective, safe, and patient-centered care.
Enhanced Patient Safety and Comfort
- Stable and Secure Positioning
- The dorsal recumbent position allows the patient to lie on their back with knees slightly flexed, ensuring stability during medical examinations.
- This position minimizes the risk of falls or sudden movements, which is critical for patients who are post-operative, elderly, or have limited mobility.
- Example: During urinary catheterization, the nurse places the patient in the dorsal recumbent position, ensuring the patient is secure and comfortable while maintaining proper patient positioning.
- Reduction of Musculoskeletal Strain
- For patients who remain in bed for extended periods, the dorsal recumbent and other recumbent positions help maintain neutral spinal alignment, reducing strain on the back and joints.
- The slight knee flexion in the dorsal recumbent position relaxes abdominal muscles, which is particularly useful for patients undergoing abdominal or pelvic examinations.
- Pressure Injury Prevention
- Recumbent positions distribute body weight more evenly, reducing prolonged pressure on bony prominences.
- Frequent repositioning using variations of recumbent positions, such as lateral recumbent, left lateral recumbent, or neutral positions, helps prevent pressure injuries, particularly in immobilized or critically ill patients.
Facilitation of Medical Examinations and Procedures
- Improved Accessibility for Clinicians
- The dorsal recumbent position provides unobstructed access to the anterior abdomen, pelvis, and genitourinary areas.
- Other recumbent positions, including decubitus and fetal positions, may be used for specialized assessments, but the dorsal recumbent position is often used for routine evaluations.
- Example: During a pelvic exam, the patient is placed in the dorsal recumbent position, which allows the clinician to perform the assessment efficiently while keeping the patient relaxed and comfortable.
- Versatility Across Procedures
- Recumbent positions can be adapted for minor procedures, such as wound care, catheterization, or dressing changes.
- Adjustments, including reclining or tripod variations, can further optimize access while maintaining patient comfort and safety.
Enhanced Nursing Workflow and Efficiency
- Reduction in Repositioning Needs
- Using dorsal recumbent and other recumbent positions reduces the frequency of repositioning for routine assessments and minor procedures.
- This enhances nursing efficiency while maintaining proper patient positioning and comfort.
- Ease of Monitoring and Observation
- Patients in dorsal recumbent or neutral positions are easily observed for vital signs, respiratory function, and comfort levels.
- Example: In a post-operative unit, maintaining patients in the dorsal recumbent position allows nurses to monitor incision sites, abdominal distension, and overall patient well-being without excessive repositioning.
Support for Patient-Centered Care
- Accommodating Special Needs
- Recumbent positions can be modified for patients with obesity, pregnancy, mobility limitations, or respiratory compromise.
- For example, slight elevation of the head in a reclining dorsal recumbent position supports breathing while maintaining a relaxed body position.
- Comfort and Psychological Ease
- Patients often feel more secure and less anxious when positioned in a dorsal recumbent or semi-reclining posture, facilitating cooperation during medical examinations and minor procedures.
- Positioning plays a significant role in patient experience, as comfort is directly linked to reduced stress and better procedural outcomes.
Conclusion
The dorsal recumbent position is a foundational element of patient positioning in nursing and various medical settings, offering a balance of comfort, safety, and accessibility that benefits both patients and healthcare providers. As a versatile recumbent position, it allows patients to lie on their back in a stable, relaxed posture while facilitating a wide range of medical examinations and minor procedures. Compared to other positions, such as lithotomy, Sims, jackknife, knee-chest, and left lateral recumbent positions, the dorsal recumbent position is often used for routine abdominal, pelvic, and genitourinary assessments, providing both clinical efficiency and patient-centered care.
Beyond procedural accessibility, recumbent positions play a critical role in promoting patient comfort and safety, preventing complications such as pressure injuries, musculoskeletal strain, and respiratory compromise. Through careful attention to proper patient positioning, including adjustments like reclining, tripod, or Trendelenburg variations, nurses can tailor the position to allow individualized support for patients with obesity, pregnancy, or mobility limitations.
The benefits of the recumbent position extend beyond individual patient encounters. They enhance nursing workflow, reduce unnecessary repositioning, and allow for effective monitoring during procedures, thereby improving overall care delivery. Understanding the distinctions and clinical applications of dorsal recumbent and related positions empowers nurses to make evidence-based decisions, ensuring that each patient is placed safely and comfortably according to procedural requirements and health status.
Ultimately, mastery of patient positioning techniques, with the dorsal recumbent position as a cornerstone, supports a standard of care that prioritizes safety, comfort, and clinical effectiveness. Nurses who integrate these practices into daily care can optimize procedural outcomes, reduce complications, and enhance the patient experience, reinforcing the critical role of positioning in modern nursing practice.
Frequently Asked Questions
How do you position a patient dorsal recumbent?
- The patient lies flat on their back (patient is on their back) with knees slightly bent and feet flat on the bed.
- Arms are positioned comfortably at the sides or on pillows for support.
- The head and neck are in a neutral alignment, and the spine is straight to maintain proper patient positioning.
How will the nurse place a patient in dorsal recumbent position correctly?
- Explain the procedure to the patient to ensure patient comfort and safety.
- Assist the patient to lie on their back on the examination table or bed.
- Place a pillow under the head and optionally under the knees to relieve lumbar strain.
- Ensure arms are supported and the body is centered on the bed, maintaining neutral alignment.
- Adjust positioning as needed for patient size, mobility limitations, or clinical procedure requirements.
What is the dorsal recumbent position most commonly used for?
- Routine abdominal, pelvic, and genitourinary examinations.
- Minor procedures such as catheterization or wound care on the anterior body.
- Patient comfort during assessments that require easy access to the front of the body without causing strain.
What important principles should you consider while positioning the patient to protect him from pain and injury?
- Maintain spinal alignment and support under pressure points to prevent pressure injuries.
- Use pillows, wedges, or supports to enhance patient comfort and reduce musculoskeletal strain.
- Communicate with the patient throughout to ensure they are comfortable and understand the procedure.
- Adjust the position for special needs (e.g., obesity, pregnancy, limited mobility) while ensuring patient safety and comfort.
- Ensure the patient is secure and stable, minimizing the risk of falls or sudden movements.
