REBT vs CBT in Nursing: Understanding the Differences Between REBT and CBT
In the practice of nursing, understanding diverse approaches to mental health care is essential for providing comprehensive patient support. Psychotherapy offers structured methods for addressing emotional distress, cognitive distortions, and maladaptive thought patterns, all of which can influence a patient’s overall well-being. Among the variety of therapeutic models, Rational Emotive Behavior Therapy (REBT) and Cognitive Behavioral Therapy (CBT) are two widely used interventions that guide nurses and therapists in supporting patients with mental health conditions. While both therapies share foundational cognitive principles, they differ in their emphasis, techniques, and approaches to emotional regulation and rational thinking.
REBT, developed by Albert Ellis, focuses on identifying and challenging irrational beliefs that contribute to emotional disturbances, promoting unconditional self-acceptance, and teaching patients to respond to situations with rational thinking. CBT, on the other hand, emphasizes restructuring thought patterns, addressing cognitive distortions, and implementing behavioral strategies to alleviate symptoms of anxiety, depression, and other common mental health issues. Both therapies provide nurses with evidence-based tools for understanding the relationship between cognition, emotions, and behaviors, yet their application in clinical practice requires careful consideration of patient needs, therapeutic goals, and clinical context.
For nurses working in diverse clinical settings, knowledge of the differences between REBT and CBT enables informed decisions about which therapy aligns with a patient’s cognitive readiness, emotional state, and therapeutic objectives. This understanding extends beyond theoretical knowledge; it informs practical interventions, enhances patient engagement, and supports measurable improvements in mental health outcomes. By exploring the origins, principles, and clinical applications of REBT and CBT, nurses can develop a nuanced understanding of how each therapy addresses irrational beliefs, cognitive distortions, and emotional distress, ultimately enhancing the quality of care delivered.
This article provides an in-depth examination of REBT versus CBT, highlighting their core principles, techniques, and applications in nursing practice. It addresses the theoretical foundations of each therapy, their approaches to cognitive and emotional challenges, and evidence-based guidance for choosing the most appropriate therapy for specific patient scenarios. Through this exploration, nursing professionals can strengthen their competence in psychotherapy, improve patient outcomes, and foster a thoughtful approach to mental health care.
Foundations and Theoretical Principles of REBT and CBT
Historical Origins of Rational Emotive Behavioral Therapy and Cognitive Behavioral Therapy
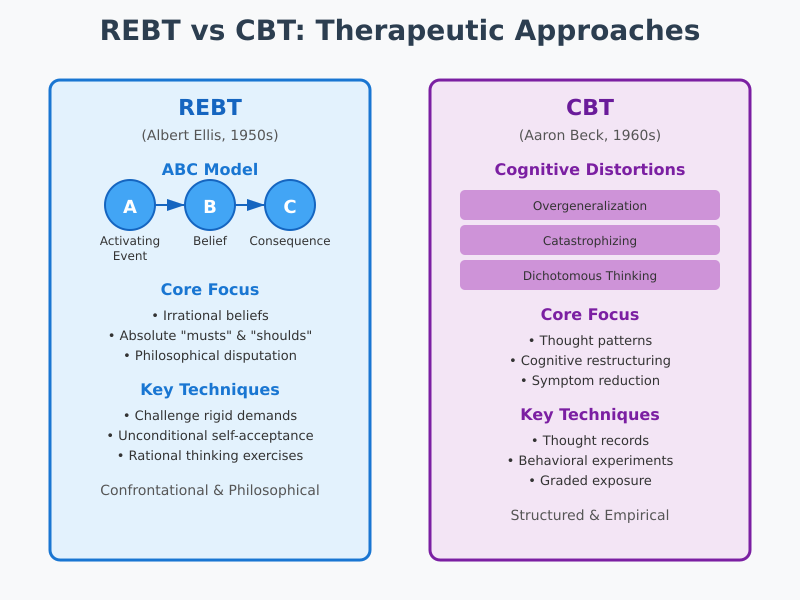
Rational Emotive Behavioral Therapy (REBT) was developed by Albert Ellis in the 1950s as a structured approach to addressing emotional distress caused by faulty thinking. Ellis observed that people’s emotional and behavioral reactions were often not proportional to external events but were significantly influenced by their irrational beliefs—rigid, absolute demands they place on themselves, others, or the world. Key elements of REBT’s historical development include:
- The formulation of the ABC model: Activating event (A), Belief (B), and Consequence (C), which illustrates how irrational beliefs lead to emotional disturbances.
- Recognition of secondary disturbance, where negative emotions are amplified by one’s own reactions to primary emotional responses.
- Integration of philosophical principles, particularly the promotion of unconditional self-acceptance and rational thinking to improve emotional regulation.
The evolution of Cognitive Behavioral Therapy (CBT) occurred in the 1960s under Aaron T. Beck, who developed cognitive therapies to address distorted thought patterns contributing to depression. While REBT emphasized philosophical disputation of irrational beliefs, CBT introduced a structured, empirical approach to cognitive restructuring, combining cognitive and behavioral interventions. Key milestones in CBT include:
- Identification of cognitive distortions, such as overgeneralization, catastrophizing, and dichotomous thinking.
- Structured CBT techniques like thought records, behavioral experiments, and graded exposure to manage anxiety, depression, and other mental health conditions.
- Adaptation to multiple clinical settings, including inpatient and outpatient mental health care, substance use disorder treatment, and community nursing interventions.
In nursing practice, understanding these origins helps professionals distinguish between a rebt therapist’s philosophical, belief-focused approach and a cbt therapist’s structured, technique-driven interventions. For example:
- In psychiatric nursing, a rebt therapist may guide a patient through identifying rigid demands, fostering rational thinking, and practicing unconditional self-acceptance to reduce anger or anxiety.
- In a primary care or outpatient setting, a cbt therapist might work with a patient on cognitive-behavioral therapy exercises like monitoring automatic thoughts or implementing behavioral experiments to address insomnia or depressive symptoms.
Core Concepts and Cognitive Focus of REBT and CBT
The core concept of REBT centers on the premise that emotional disturbances arise from irrational beliefs rather than external events. These beliefs often include absolute “musts” or “shoulds,” such as:
- “I must always succeed, or I am worthless.”
- “Others must treat me fairly, or life is intolerable.”
- “I cannot tolerate discomfort or emotional pain.”
REBT focuses on challenging these beliefs using techniques that include:
- Disputation of irrational beliefs, questioning their logic and practical consequences.
- Emphasis on unconditional self-acceptance, helping patients separate self-worth from performance or approval.
- Behavioral exercises, such as role-playing or homework assignments, to reinforce rational thinking.
By comparison, CBT focuses on identifying and modifying cognitive distortions and thought patterns that contribute to maladaptive emotions and behaviors. Its techniques emphasize:
- Thought records to track negative automatic thoughts and their impact on emotions and behaviors.
- Cognitive restructuring, helping patients evaluate and replace distorted thinking with more balanced, realistic cognitions.
- Integration of behavioral strategies to change actions alongside thoughts, useful in addressing anxiety and depression or behavioral challenges.
Key distinctions between REBT and CBT include:
- Therapeutic focus: REBT targets beliefs and philosophical acceptance; CBT targets maladaptive thought patterns and behaviors.
- Approach to emotional distress: REBT addresses both primary and secondary disturbance, emphasizing rational thinking, while CBT primarily focuses on symptom reduction through structured cognitive-behavioral interventions.
- Application style: REBT is more confrontational and philosophical, fostering insight and self-reflection, whereas CBT is structured, stepwise, and often used in short-term therapy formats.
Example in nursing practice:
- A patient with generalized anxiety disorder might work with a rebt therapist to challenge beliefs like “I cannot cope with uncertainty” and develop rational thinking skills.
- The same patient could engage in CBT therapy, completing thought records to identify cognitive distortions and practicing exposure techniques to gradually tolerate uncertainty.
Both approaches are evidence-based and widely used in mental health care, giving nurses a range of options for tailoring interventions to individual patient needs. Understanding these foundational principles is crucial for choosing between REBT and CBT, guiding effective mental health support, and improving emotional and behavioral outcomes in clinical settings.
Cognitive Distortions and Emotional Distress in REBT and CBT
REBT Approach to Irrational Beliefs and Emotional Disturbance
REBT Approach to Irrational Beliefs and Emotional Disturbance
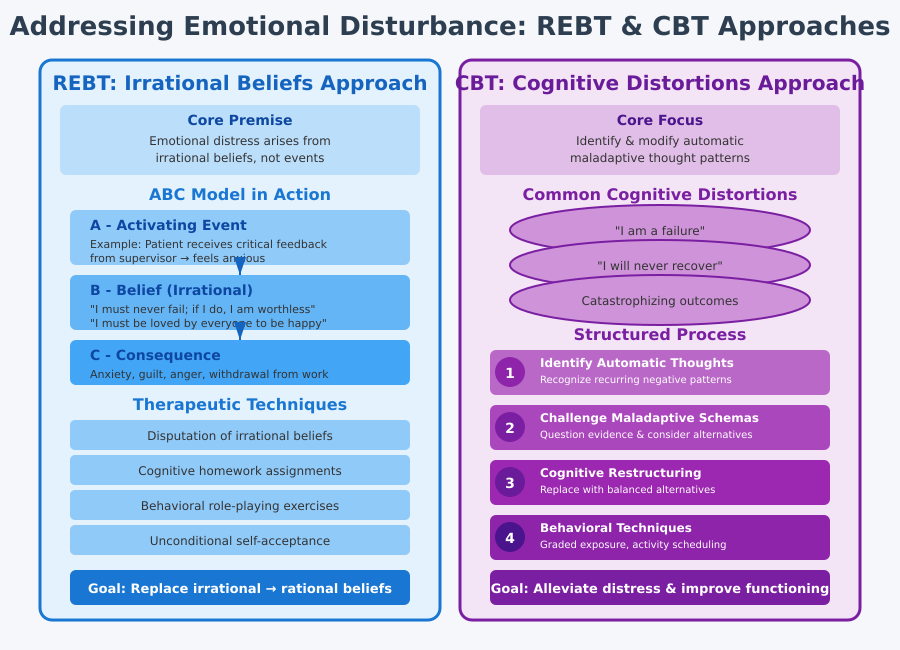
Rational Emotive Behavior Therapy (REBT) is built on the premise that emotional distress arises primarily from irrational beliefs rather than external events. Albert Ellis emphasized that maladaptive emotions, such as anxiety, guilt, or anger, are often intensified by secondary disturbance, which occurs when individuals react negatively to their own initial emotional responses. In nursing practice, understanding how REBT addresses these dynamics can help professionals support patients experiencing mental health conditions or emotional crises.
A cornerstone of REBT is the ABC model, which guides both therapists and patients in examining the connection between beliefs and emotional outcomes:
- A – Activating Event: Any situation or event that triggers a cognitive or emotional response.
- Example in nursing: A patient receives critical feedback from a supervisor and immediately feels anxious.
- B – Belief: The interpretation or irrational belief about the activating event.
- Example: “I must never fail; if I do, I am worthless.”
- C – Consequence: The emotional and behavioral outcome resulting from the belief.
- Example: Anxiety, irritability, or withdrawal from work.
The REBT approach teaches patients to identify and dispute irrational beliefs, replacing them with rational alternatives that reduce emotional distress and promote unconditional self-acceptance. Key therapeutic techniques include:
- Disputation of irrational beliefs: Guiding patients to question the logic, evidence, and utility of maladaptive thoughts.
- Cognitive homework: Encouraging patients to apply rational thinking in daily life situations.
- Behavioral assignments: Role-playing or experimenting with alternative responses to triggering events.
- Promotion of unconditional self-acceptance: Teaching patients that self-worth does not depend on outcomes, performance, or others’ approval.
In practice, a rebt therapist working in a mental health nursing unit might help a patient with depression recognize the belief, “I must be loved by everyone to be happy,” and guide them to adopt a rational alternative: “I prefer to be liked, but my value does not depend on others’ approval.” This approach directly reduces secondary disturbance and improves emotional regulation.
CBT Strategies for Managing Cognitive Distortions and Emotional Responses
Cognitive Behavioral Therapy (CBT) addresses cognitive distortions—automatic, maladaptive thought patterns that exacerbate emotional and behavioral challenges. Unlike REBT, which focuses on philosophical rationality and unconditional self-acceptance, CBT focuses on structured identification, evaluation, and modification of these thought patterns to alleviate emotional distress and improve functioning.
Key CBT strategies include:
- Identifying automatic thoughts: Nurses and therapists help patients recognize recurring negative or distorted thoughts, such as “I am a failure” or “I will never recover.”
- Challenging maladaptive schemas: Patients are guided to question the evidence for their thoughts and consider alternative interpretations.
- Example: A patient with anxiety might record a worry about attending a social event and evaluate the likelihood of feared outcomes.
- Cognitive restructuring: Patients systematically replace distorted thoughts with balanced, evidence-based alternatives.
- Behavioral techniques: CBT integrates practical exercises to reinforce cognitive change, such as graded exposure, relaxation training, or activity scheduling.
In nursing practice, a cbt therapist might work with a patient suffering from substance use disorder who experiences cravings triggered by stress. Through cognitive-behavioral therapy, the nurse helps the patient recognize the thought, “I cannot cope without using,” challenge its accuracy, and implement coping strategies, such as deep breathing or social support, to manage cravings and emotional responses.
CBT also provides a clear framework for monitoring progress through thought logs and outcome measures, making it particularly valuable for managing anxiety and depression, insomnia, and other common mental health issues in both inpatient and outpatient nursing settings.
Comparative Insights: REBT vs CBT in Handling Cognitive and Emotional Disturbances
- Focus of REBT: Targets irrational beliefs, emphasizes rational thinking, and reduces secondary disturbance using disputation and philosophical reasoning.
- Focus of CBT: Targets cognitive distortions and maladaptive thought patterns, emphasizing structured cognitive and behavioral interventions.
- Integration in nursing: Both therapies can be applied to mental health care, patient education, and psychoeducation, but REBT is particularly effective for patients who benefit from exploring the philosophical basis of their beliefs, while CBT is optimal for patients who respond to structured, evidence-based exercises.
- Practical example:
- A patient experiencing workplace stress may work with a rebt therapist to challenge rigid beliefs about performance and approval.
- The same patient may simultaneously use CBT therapy to monitor thought patterns, practice cognitive restructuring, and implement behavioral strategies to reduce stress and anxiety.
Key Differences Between REBT and CBT in Clinical Practice
Goals and Outcomes of REBT Compared to CBT
In clinical nursing practice, understanding the goals and outcomes of REBT versus CBT is crucial for selecting the most appropriate intervention for patients experiencing emotional distress or mental health conditions.
REBT aims to reduce irrational beliefs that drive maladaptive emotional and behavioral responses. The therapy encourages patients to adopt rational thinking and unconditional self-acceptance, which helps them:
- Manage emotional responses such as anger, guilt, or anxiety.
- Reduce secondary disturbance, the heightened emotional reaction to one’s own negative feelings.
- Develop self-directed coping strategies that promote resilience across diverse clinical situations.
CBT focuses on modifying cognitive distortions and thought patterns, helping patients recognize and restructure maladaptive thinking while implementing behavioral strategies to improve functioning. CBT’s objectives include:
- Reducing symptoms of anxiety and depression.
- Addressing maladaptive behaviors through structured cognitive-behavioral therapy exercises.
- Enhancing problem-solving skills and coping mechanisms in real-life situations, such as managing stress, sleep disturbances, or interpersonal conflicts.
Example in nursing practice:
- A patient with generalized anxiety may work with a rebt therapist to challenge beliefs like, “I cannot tolerate uncertainty,” fostering rational thinking to reduce worry.
- The same patient may engage in cbt therapy, maintaining a thought record, practicing graded exposure to anxiety-inducing situations, and implementing relaxation exercises to achieve measurable symptom relief.
Techniques and Strategies in Psychotherapy
The techniques of REBT and CBT demonstrate their different approaches to cognitive and emotional challenges.
REBT techniques include:
- Disputing beliefs: Directly challenging irrational beliefs using logical, empirical, and pragmatic questioning.
- Rational emotive exercises: Behavioral experiments and imagery to reinforce rational thinking.
- Role-playing: Simulating stressful or conflict situations to practice adaptive responses.
- Homework assignments: Encouraging patients to apply REBT principles outside therapy sessions to promote rational thinking and reduce emotional distress.
CBT techniques include:
- Thought records: Structured exercises that track automatic thoughts, emotions, and behavioral responses.
- Cognitive restructuring: Systematic evaluation of distorted thinking and replacement with balanced, evidence-based alternatives.
- Behavioral experiments: Testing beliefs through real-life experimentation to evaluate accuracy and reduce maladaptive behaviors.
- Exposure therapy: Gradual exposure to feared stimuli to reduce avoidance and anxiety symptoms.
Example in nursing practice:
- A rebt therapist may work with a patient struggling with perfectionism, having them confront unrealistic standards and practice rational self-talk.
- A cbt therapist may help the same patient create a graded exposure plan to complete tasks they have been avoiding due to fear of failure, while maintaining a thought record to challenge catastrophic thinking.
Handling Emotional Distress and Secondary Disturbance
Both REBT and CBT address emotional challenges, but their strategies and emphasis differ:
REBT’s approach:
- Targets both primary and secondary disturbance, recognizing that negative emotions are intensified by irrational interpretations of initial feelings.
- Promotes unconditional self-acceptance to reduce self-criticism and improve coping.
- Uses philosophical reasoning and disputation to teach patients how to manage intense emotional reactions effectively.
CBT’s approach:
- Focuses on modifying cognitive distortions and changing behaviors to manage emotional symptoms.
- Emphasizes monitoring and restructuring thought patterns that perpetuate anxiety, depression, or stress.
- Employs behavioral interventions, such as graded exposure or activity scheduling, to complement cognitive change.
Example in clinical practice:
- For a patient experiencing workplace stress:
- A rebt therapist may challenge beliefs like “I must never fail” and encourage the patient to accept human imperfection, reducing secondary disturbance.
- A cbt therapist may teach coping skills, like breaking tasks into manageable steps and reframing negative automatic thoughts, thereby reducing emotional distress and improving performance.
In practice, nurses may integrate both therapies depending on patient needs. REBT is often used when philosophical reflection and rational thinking are key to resolving persistent irrational beliefs, while CBT is effective when structured interventions and measurable cognitive-behavioral outcomes are desired. Understanding these major differences between REBT and CBT enables nurses to tailor therapy, enhance patient engagement, and improve mental health outcomes in diverse clinical settings.
Application of REBT and CBT in Nursing Practice
Implementing CBT in Nursing Settings
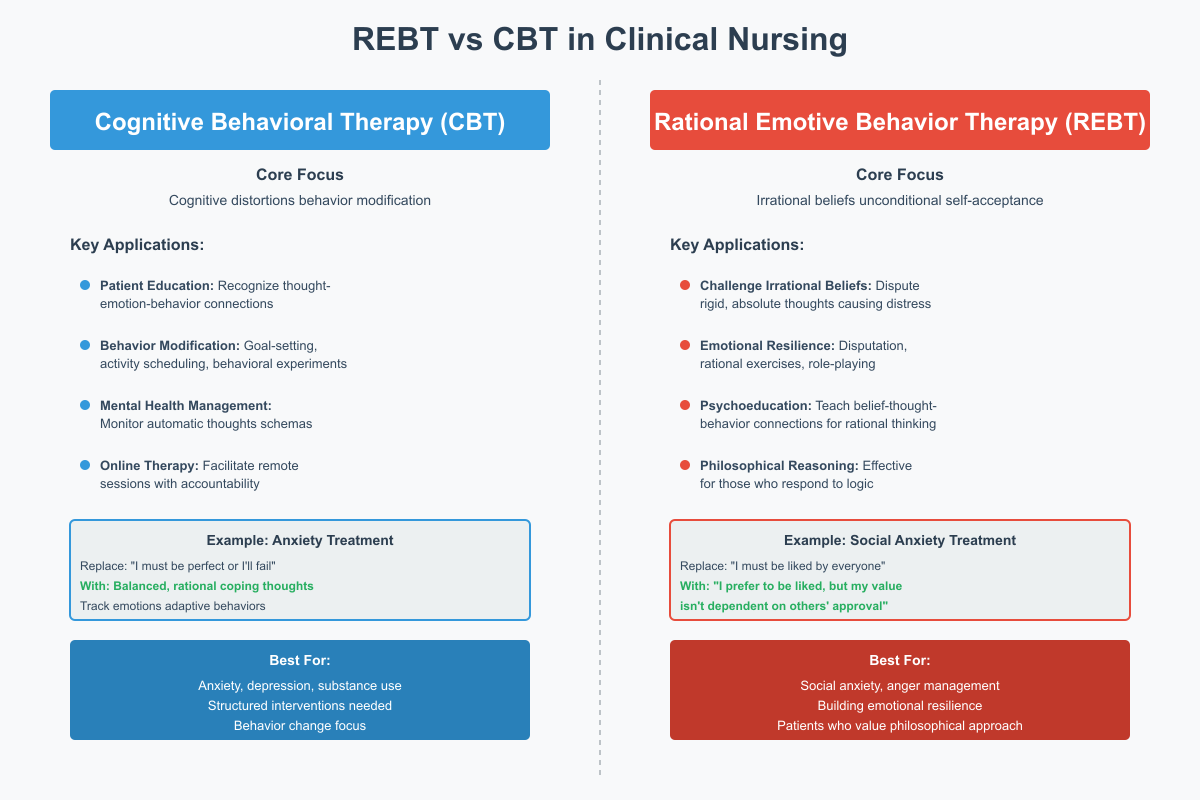
Cognitive Behavioral Therapy (CBT) is a widely utilized cognitive therapy in nursing practice for addressing mental health conditions such as anxiety and depression, substance use disorder, and stress-related disorders. Nurses trained in CBT techniques can guide patients in modifying maladaptive thought patterns and behaviors while improving emotional regulation.
Key applications of CBT therapy in nursing include:
- Patient Education: Nurses teach patients to identify cognitive distortions and understand how thoughts influence emotions and behaviors.
- Example: A patient experiencing anxiety may use thought records to recognize catastrophic thinking like “I will fail if I don’t do everything perfectly,” and reframe it into rational, balanced thoughts.
- Behavior Modification: CBT encourages gradual behavioral change through behavioral experiments, activity scheduling, and graded exposure.
- Example: A patient with depression who avoids social interaction may start by attending short group sessions, gradually increasing participation while monitoring emotional responses.
- Management of Mental Health Conditions: Nurses implement CBT strategies to help patients challenge automatic thoughts and modify maladaptive schemas.
- Example: In a clinical setting, a cbt therapist helps a patient with insomnia track worry patterns and restructure thoughts such as “I must sleep perfectly or tomorrow will be ruined,” reducing nighttime anxiety.
- Integration in Online and Telehealth Platforms: Online CBT allows nurses to provide talk therapy remotely, guiding patients through cognitive restructuring exercises, exposure tasks, and self-monitoring activities.
Implementing REBT in Nursing Practice
Rational Emotive Behavior Therapy (REBT) emphasizes irrational beliefs, secondary disturbance, and the development of unconditional self-acceptance to improve emotional resilience. Nurses trained in rebt methods help patients challenge irrational thinking and adopt rational thinking strategies that positively influence both emotions and behavior.
Applications of REBT therapy in nursing include:
- Challenging Irrational Beliefs: Nurses assist patients in identifying rigid, extreme, or absolute beliefs that contribute to emotional distress.
- Example: A patient with social anxiety may work with a rebt therapist to replace the belief “I must always be liked” with a rational alternative: “I prefer to be liked, but my self-worth does not depend on others’ approval.”
- Promoting Emotional Resilience: Through disputation, rational emotive exercises, and role-playing, patients learn to manage intense emotional responses and reduce secondary disturbance.
- Example: A patient with anger management difficulties may practice identifying triggers, disputing irrational beliefs, and applying rational coping strategies to respond calmly in stressful situations.
- Patient Education and Psychoeducation: Nurses introduce rebt therapy principles to help patients understand how irrational beliefs influence emotions and behaviors REBT vs CBT, fostering long-term cognitive and emotional regulation.
- Practical Integration in Nursing Care: REBT is effective in both inpatient and outpatient settings for patients who benefit from philosophical reasoning and reflective exercises.
- Example: In an outpatient mental health clinic, a nurse may combine REBT exercises with mindfulness practices to enhance unconditional self-acceptance and resilience in patients struggling with chronic anxiety or depressive thought patterns.
Choosing Between REBT and CBT in Clinical Nursing
Factors Influencing Therapy Selection
Cognitive Behavioral Therapy (CBT) is one of the most widely applied cognitive therapies in nursing, particularly for managing anxiety and depression, substance use disorder, and other mental health conditions. Nurses trained in CBT techniques can facilitate structured interventions, provide behavior modification, and support patients in reshaping thought patterns that drive maladaptive behaviors.
Key ways nurses implement CBT therapy in clinical practice include:
- Patient Education: Nurses teach patients to recognize cognitive distortions, understand the connection between thoughts, emotions, and behaviors, and practice cognitive-behavioral therapy strategies.
- Example: A patient with generalized anxiety may learn to replace the thought “I will fail if I don’t perform perfectly” with a more balanced cognition, promoting rational coping.
- Behavior Modification: CBT encourages active behavioral change through goal-setting, activity scheduling, and behavioral experiments.
- Example: A patient with depression avoiding social interaction may gradually re-engage in social activities, tracking both emotions and adaptive behaviors.
- Management of Mental Health Conditions: Nurses use cbt therapies to monitor automatic thoughts and modify maladaptive schemas.
- Example: A patient with insomnia may maintain a thought record to identify unhelpful beliefs like “I must sleep perfectly or I will fail tomorrow,” while learning relaxation techniques.
- Online Therapy Integration: Nurses can facilitate online CBT sessions, providing guidance and accountability for patients practicing talk therapy techniques at home.
Evidence-Based Recommendations for REBT vs CBT
Rational Emotive Behavior Therapy (REBT) focuses on irrational beliefs, secondary disturbance, and promoting unconditional self-acceptance to build emotional resilience. Nurses applying REBT methods help patients challenge maladaptive beliefs and adopt rational thinking, improving both emotional regulation and behavioral outcomes.
Key applications of REBT therapy in nursing include:
- Challenging Irrational Beliefs: Nurses help patients identify and dispute rigid or absolute thoughts that contribute to emotional distress.
- Example: A patient with social anxiety may be guided by a rebt therapist to transform the belief “I must be liked by everyone” into the rational perspective: “I prefer to be liked, but my value is not dependent on others’ approval.”
- Promoting Emotional Resilience: Through disputation, rational emotive exercises, and role-playing, patients practice responding adaptively to stressors.
- Example: A patient with anger issues may identify triggers, evaluate underlying irrational beliefs, and apply rational coping strategies to reduce secondary emotional reactions.
- Patient Education and Psychoeducation: Nurses introduce rebt therapy principles to teach the connection between beliefs, thought patterns, and behaviors, encouraging long-term rational thinking.
- Practical Integration in Nursing: REBT is particularly effective for patients who respond to philosophical reasoning.
- Example: In an outpatient clinic, patients with chronic anxiety may combine REBT exercises with mindfulness techniques to reinforce unconditional self-acceptance and reduce secondary disturbance.
Comparative Insights: Applying REBT and CBT in Nursing
- CBT focuses on structured interventions and measurable outcomes, ideal for behavior modification and monitoring mental health issues.
- REBT focuses on challenging irrational beliefs and cultivating rational thinking, ideal for addressing deeply ingrained maladaptive beliefs and promoting emotional resilience.
- Integration in practice: Nurses may use cbt and rebt complementarily depending on patient needs:
- A patient with depression may benefit from cbt therapy to structure coping strategies.
- REBT may simultaneously address core irrational beliefs that amplify emotional distress.
Measuring Outcomes and Effectiveness of REBT vs CBT
Patient Outcomes and Symptom Improvement
Evaluating the effectiveness of REBT vs CBT in nursing practice is essential to ensure that therapeutic interventions achieve meaningful improvements in emotions and behaviors REBT vs CBT, cognitive functioning, and overall patient well-being. Both approaches provide structured methods to monitor outcomes, but the focus differs slightly:
REBT focuses on reducing irrational beliefs and managing secondary disturbance, aiming to improve emotional stability and resilience. Outcomes commonly assessed in clinical practice include:
- Reduction of emotional distress: Patients report decreases in anxiety, anger, or depressive symptoms as irrational beliefs are challenged.
- Example: A patient with social anxiety may demonstrate reduced avoidance and improved engagement in group activities after practicing rebt methods such as disputing beliefs.
- Enhanced rational thinking and self-acceptance: Measures of cognitive change often include self-report scales assessing the degree of unconditional self-acceptance and rational response to triggering events.
- Improved coping with stressors: Patients learn strategies to tolerate uncertainty or discomfort without excessive emotional reactivity, demonstrating resilience in daily functioning.
CBT focuses on modifying cognitive distortions and maladaptive thought patterns to achieve both emotional and behavioral outcomes. Measurable outcomes include:
- Symptom reduction in mental health conditions: Standardized assessments (e.g., Beck Depression Inventory, GAD-7) indicate decreases in anxiety and depression severity.
- Example: A patient with major depressive disorder may report improvements in mood and daily functioning after completing cognitive-behavioral therapy sessions, using thought records and activity scheduling.
- Cognitive improvement: Assessment tools measure changes in thought patterns, accuracy of perceptions, and reduced catastrophizing or overgeneralization.
- Behavioral adaptation: Patients demonstrate changes in habits, routines, or coping strategies, such as better sleep hygiene or social engagement, following cbt techniques like behavioral experiments and graded exposure.
Comparative insights:
- REBT outcomes often emphasize philosophical and emotional shifts, including acceptance and rational evaluation of beliefs.
- CBT outcomes focus on observable cognitive and behavioral changes, making it suitable for structured outcome measurement in nursing care.
- In practice, nurses may combine approaches, using REBT methods to address core irrational beliefs while tracking CBT treatment outcomes such as symptom improvement and behavioral engagement.
Training and Competencies for Nursing Therapists
Effective delivery of REBT or CBT therapy in nursing settings requires specific skills and professional competencies. Nurses trained in these interventions not only implement therapy but also evaluate outcomes to ensure patient safety and improvement.
Essential competencies for nurses providing REBT include:
- Ability to identify irrational beliefs and secondary disturbance in patients.
- Skill in applying rational emotive behavioral therapy techniques, including disputation, role-play, and cognitive exercises.
- Understanding of emotional distress management and methods to foster unconditional self-acceptance.
- Competence in psychoeducation to teach patients how to apply rational thinking outside therapy sessions.
Essential competencies for nurses providing CBT include:
- Proficiency in cognitive-behavioral therapy methods, including thought records, cognitive restructuring, and behavioral experiments.
- Knowledge of cognitive distortions and their impact on mental health conditions.
- Ability to monitor progress using standardized outcome measures and adjust interventions accordingly.
- Skills in facilitating online CBT or talk therapy sessions for remote patient care.
Examples of nursing application:
- A cbt therapist in an outpatient clinic may guide patients with anxiety in completing daily thought records and graded exposure exercises, while assessing symptom reduction via standardized scales.
- A rebt therapist in a psychiatric ward may help patients with anger management challenge irrational beliefs such as “I cannot tolerate being disrespected,” fostering rational responses and emotional regulation.
Integrating these competencies ensures that nurses can deliver therapy effectively, measure outcomes accurately, and adapt interventions to meet the patient’s cognitive readiness, emotional needs, and behavioral goals. This professional preparedness enhances both patient outcomes and overall quality of nursing care.
Conclusion
Understanding the nuances of REBT vs CBT is essential for nurses who aim to provide evidence-based, patient-centered care in diverse clinical settings. Both rational emotive behavior therapy and cognitive-behavioral therapy offer structured approaches to addressing emotional distress, cognitive distortions, and maladaptive thought patterns, yet they differ in focus, techniques, and therapeutic goals. REBT focuses on challenging irrational beliefs and cultivating unconditional self-acceptance, enabling patients to manage both primary and secondary disturbance effectively. In contrast, CBT focuses on modifying distorted cognition and implementing behavioral interventions to achieve measurable symptom improvement in mental health conditions such as anxiety and depression, substance use, and stress-related disorders.
For nursing practice, these differences have tangible implications. Nurses skilled in REBT methods can guide patients toward rational thinking, foster emotional resilience, and reduce the impact of self-defeating beliefs. Meanwhile, nurses trained in CBT therapies can facilitate structured interventions, monitor cognitive and behavioral change, and support patients through talk therapy and online CBT modalities. Selecting the appropriate approach requires careful assessment of patient needs, cognitive readiness, and the nurse’s expertise, ensuring interventions are both effective and personalized.
By integrating insights from both rebt and cbt, nurses can enhance therapeutic outcomes, promote emotions and behaviors REBT vs CBT, and provide holistic care that addresses both thought patterns and emotional regulation. Ultimately, mastery of these therapies empowers nursing professionals to deliver care that not only alleviates psychological distress but also equips patients with the tools for long-term cognitive and emotional resilience. Understanding the key differences between REBT and CBT, as well as their practical application, is therefore crucial for optimizing mental health outcomes and advancing professional nursing practice.
Frequently Asked Questions
What is the main difference between REBT and CBT?
The main difference is that REBT focuses on identifying and challenging irrational beliefs to promote rational thinking and unconditional self-acceptance, whereas CBT focuses on recognizing and restructuring distorted thought patterns and behaviors to improve emotional and functional outcomes.
What is the 5-minute rule in CBT?
The 5-minute rule is a CBT strategy where patients commit to engaging in a challenging task or confronting an anxiety-provoking situation for just five minutes. This short, structured exposure helps reduce avoidance, build confidence, and gradually change maladaptive thought patterns.
Is Rational Emotive Behavior Therapy (REBT) CBT?
Yes and no. REBT is a form of cognitive therapy that shares principles with CBT, such as the link between thoughts, emotions, and behaviors, but it is distinct in emphasizing philosophical reasoning, irrational beliefs, and unconditional self-acceptance as central to therapy.
What is one of the main differences between cognitive therapy (CT) and Rational Emotive Behavioral Therapy (REBT)?
One key difference is that CT focuses primarily on restructuring distorted automatic thoughts, while REBT addresses deeper, core irrational beliefs and incorporates disputation and rational thinking exercises to modify emotional responses.
