Sample PICOT Questions in Nursing: Research Guides, Clinical Question Examples, and Evidence-Based Practice Tips
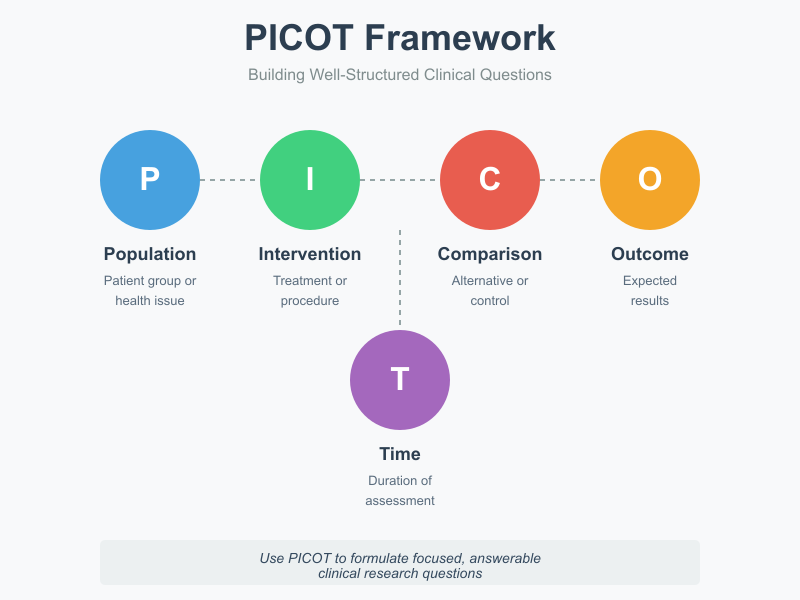
Formulating a well-structured clinical question is a fundamental step in nursing research and evidence-based practice. Just as standardized care pathways guide patient management, the PICOT framework offers nurses a systematic method for translating clinical uncertainties into focused, answerable questions. By breaking down a problem into five essential components—Population, Intervention, Comparison, Outcome, and Time—the framework provides a foundation for critical inquiry that informs both research design and nursing practice.
At its core, a PICOT question bridges the gap between clinical experience and scientific evidence. It enables nurses to refine broad clinical observations—such as how to reduce pain among patients with chronic conditions or control high blood pressure in hypertensive adults—into measurable, researchable questions. Through this process, practitioners move beyond intuition toward decisions grounded in relevant evidence and the best available data. The structure also supports nurses in comparing interventions, such as oxygen therapy versus standard care or psychological intervention compared with no intervention, to evaluate their effectiveness in improving health outcomes.
The value of the PICOT format lies not only in its clarity but also in its role in strengthening the research process. Nursing students, clinicians, and researchers alike use it to formulate well-built clinical questions that guide literature searches, support the development of nursing interventions, and enhance patient care. Whether investigating blood glucose control among patients with type 2 diabetes, exploring pain relief strategies for patients with chronic pain, or assessing maternal health outcomes in pregnant women, a precise question structure ensures that research remains focused, reproducible, and clinically meaningful.
In contemporary nursing practice, the integration of the PICOT framework reflects a broader commitment to evidence-based nursing. It helps align clinical decision-making with measurable outcomes and supports the translation of findings into practice settings—from the ICU and acute care units to community health and maternal-child programs. By grounding clinical inquiry in structured reasoning, the PICOT question has become an indispensable element of professional nursing research, linking thoughtful questioning with improved patient outcomes and advancing the science of nursing practice.
Understanding the PICOT Framework
The PICOT framework is one of the most effective tools in nursing research and evidence-based practice. It provides a structured approach for developing clear, focused, and answerable clinical questions. Whether a nurse is investigating ways to reduce hospital readmissions, evaluating pain management strategies, or assessing patient education methods, the PICOT question serves as the foundation for meaningful inquiry. By breaking down a complex clinical issue into manageable components, the framework helps guide the research process, making it easier to locate, appraise, and apply the best available evidence in nursing practice.
What Does PICOT Stand For?
PICOT is an acronym that represents the five essential elements of a well-structured clinical question:
- P (Population or Patient Problem): Describes the patient group or health issue of interest. For instance, “older adults with type 2 diabetes” or “postoperative patients experiencing acute pain.”
- I (Intervention): Refers to the treatment, procedure, or exposure being considered, such as “using mindfulness-based stress reduction” or “implementing a nurse-led discharge education program.”
- C (Comparison): Indicates the alternative or control intervention, if applicable. This might include “standard care,” “no intervention,” or “another form of therapy.”
- O (Outcome): Defines what results are expected or measured, such as “improved wound healing,” “reduced anxiety,” or “lower fall rates.”
- T (Time): Specifies the duration over which the outcome is assessed, like “within three months post-surgery” or “during a six-week rehabilitation period.”
Together, these elements form the PICOT format, transforming a broad topic into a specific, measurable question that can guide both research and clinical decision-making.
Why is the PICOT Format Important in Nursing Research?
In nursing research, clarity is crucial. The PICOT question ensures that a research topic is not only relevant but also structured in a way that can be effectively studied. It helps nurses formulate questions that align with evidence-based practice by focusing on measurable outcomes and well-defined interventions. Using the PICOT format allows researchers to conduct targeted literature searches, identify gaps in current knowledge, and design studies that directly address patient care challenges.
For example, instead of asking, “Does exercise help with hypertension?” a PICOT-based question would be: “In adults with hypertension (P), does participation in a daily 30-minute walking program (I), compared to no structured exercise (C), reduce blood pressure levels (O) over a 12-week period (T)?” This version offers a clearer research direction and produces results that are easier to evaluate and apply in practice.
The PICOT question format also promotes critical thinking and ensures that research efforts remain patient-centered. By emphasizing population and outcome, it connects the scientific inquiry to real-world nursing concerns, bridging the gap between theory and bedside care.
How Can PICOT Questions Improve Clinical Practice?
Well-formulated PICOT questions are not limited to research settings—they are equally valuable in day-to-day nursing practice. They help nurses approach clinical uncertainties systematically, identify the best available evidence, and apply it to improve patient outcomes. In essence, the PICOT framework transforms routine problem-solving into evidence-based practice.
For example, a nurse noticing frequent catheter-associated infections in a medical-surgical unit might ask: “In hospitalized patients with urinary catheters (P), does using a closed drainage system (I), compared to an open drainage system (C), reduce the rate of catheter-associated infections (O) during hospitalization (T)?”
This question can guide literature review, quality improvement initiatives, and policy changes.
By encouraging precision, PICOT helps ensure that interventions are not based on tradition or opinion but grounded in measurable outcomes and validated research. Over time, this approach enhances clinical reasoning, supports patient safety, and contributes to the advancement of nursing as a discipline rooted in evidence-based practice.
Ultimately, understanding and applying the PICOT framework empowers nurses to become active participants in research and innovation. It allows them to link clinical experience with scholarly inquiry, ensuring that nursing practice continues to evolve in response to the best available evidence.
Components of a Strong PICOT Question
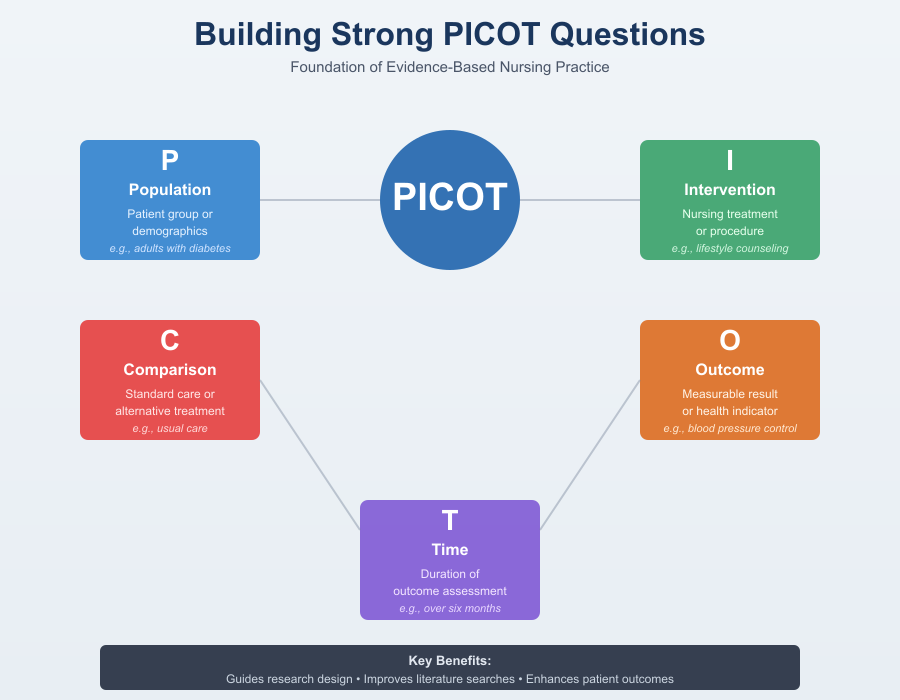
A strong PICOT question is the foundation of high-quality nursing research and evidence-based practice (EBP). It guides how nurses identify a clinical problem, gather relevant evidence, and apply findings to improve patient care. The PICOT format ensures every clinical question is structured, measurable, and applicable in real-world nursing practice. When each element—Population, Intervention, Comparison, Outcome, and Time—is well-defined, nurses can design studies, conduct literature searches, and evaluate health outcomes with clarity and focus.
What Are the Key Elements of a PICOT Question?
The PICOT framework helps nursing students and professionals formulate a research question that is focused and testable. Each letter in PICOT stands for a component essential in developing an evidence-based inquiry:
- P (Population): This refers to the group or patient population being studied. It may involve specific demographics, conditions, or settings—such as patients with chronic pain, adolescents with type 1 diabetes, or elderly patients with hypertension. For example, a nurse may explore how oxygen therapy affects mechanically ventilated patients in the ICU.
- I (Intervention): This specifies the nursing intervention or treatment under consideration, such as negative pressure wound therapy, psychological intervention, or blood pressure monitoring. Interventions are designed to improve health outcomes or reduce the risk of complications.
- C (Comparison): This defines what the intervention is being compared against—such as standard care, usual care, placebo, or no intervention. Comparisons like “compared to standard care” or “compared with no intervention” help determine the intervention’s effectiveness.
- O (Outcome): The desired or measurable result of the intervention. This could include pain relief, improved blood sugar levels, blood pressure control, or a reduction in hospital readmissions. Outcomes should be measurable and clinically meaningful.
- T (Time): The timeframe over which the effect is measured—such as during hospitalization, over six months, or during pregnancy and six weeks postpartum. Including time ensures that outcomes are tracked consistently and accurately.
Together, these elements allow nurses to construct a good PICOT question that aligns with evidence-based nursing and supports the research process in academic and clinical settings.
How Do Population and Intervention Influence Research Outcomes?
Both the population and intervention directly determine the focus and validity of a PICOT question.
- Population: Clearly defining the population improves the accuracy of the research design. For instance, patients with chronic conditions such as hypertension, type 1 diabetes, or breast cancer require targeted interventions. A focused clinical population ensures that findings are relevant and accurate in diagnosing issues or predicting responses.
- Intervention: A well-defined nursing intervention—such as blood glucose monitoring, oxygen therapy, or pain relief strategies—drives the quality of clinical research. Specific interventions make it easier to replicate studies and evaluate their impact on health outcomes. For example, a nurse might explore whether psychological intervention among patients with chronic pain can reduce pain compared to usual care.
- Relevance to patient care: The PICOT format ensures interventions are grounded in clinical reality, enhancing nursing practice and ensuring results are applicable to patients with chronic illnesses.
Defining the right population and intervention also helps refine the search strategy, making it easier to locate research guides and libguides at university databases for the research paper.
What Role Do Comparison and Outcome Play in Formulating Questions?
The comparison and outcome components are what make a PICOT question measurable and meaningful.
- Comparison: A clinical question must specify whether the new intervention is being tested compared to standard care, compared to no intervention, or compared to placebo. For example, a study may compare negative pressure wound therapy to standard dressing care among patients with chronic wounds. This helps determine whether the new nursing intervention provides superior results or simply maintains usual care outcomes.
- Outcome: Outcomes are the indicators of success. In evidence-based nursing, outcomes like blood pressure control, blood glucose regulation, or pain relief are central to determining whether an intervention should be implemented. These outcomes must be measurable, objective, and tied to evidence-based standards.
- Example: A nursing PICOT question might ask, “In adults with high blood pressure (P), does home blood pressure monitoring (I), compared to usual care (C), improve blood pressure control (O) over six months (T)?” This clearly identifies the population, intervention, comparison, and measurable outcome.
A well-constructed PICOT question not only strengthens the research design but also aligns with evidence-based practice goals. By ensuring that comparison and outcome are specific, nurses can evaluate interventions effectively, improve patient care, and make data-driven decisions in both clinical and academic settings.
How Can Time Frame Be Integrated into a PICOT Question?
Integrating the time frame into a PICOT question is one of the most effective ways to make a clinical or research question more specific, measurable, and applicable to nursing practice. In the PICOT format, the “T” represents “Time,” which defines the period needed to observe and measure the outcomes of an intervention. Without this element, a PICOT question may remain too broad or lack direction, making it difficult to assess results accurately or apply findings to evidence-based practice.
The time frame sets boundaries around how long an outcome should be monitored and when results should be evaluated. For example, a nurse formulating a nursing PICOT question might ask, “In adult patients with hypertension (P), does nurse-led lifestyle counseling (I), compared to standard care (C), reduce systolic blood pressure (O) over six months (T)?” In this case, the six-month time frame gives the question structure and defines when success will be determined. This clarity is essential for designing a study, selecting data collection methods, and interpreting results that inform nursing research.
Incorporating time also ensures that the clinical question aligns with realistic nursing goals and patient outcomes. Some interventions produce rapid effects—such as pain relief following a new analgesic protocol—while others, like lifestyle modification or education-based interventions, require longer follow-up periods to demonstrate measurable change. By integrating a time frame, the PICOT question reflects the natural course of the condition being studied and the expected response to the intervention. This alignment strengthens the validity of the evidence-based practice process and improves the translation of research into clinical application.
When formulating PICOT question examples, it’s important to choose a time frame that fits both the clinical setting and the type of outcome being studied. For instance, a PICOT question related to postoperative wound healing might measure improvement “within four weeks,” while one addressing long-term diabetes control might focus on results “after six months.” The key is to select a time period that is neither too short to detect meaningful change nor too long to maintain practical relevance for patient care and nursing practice.
The inclusion of time also enhances consistency when comparing outcomes between different interventions or patient groups. Both the intervention and the comparison group should share the same observation period to ensure that differences in outcomes are due to the intervention itself, not variations in time. This uniformity contributes to more reliable and credible results in nursing research, where precision and replicability are crucial for improving clinical outcomes.
Moreover, defining time helps guide literature searches in research guides and databases. When nurses use the PICOT format to structure their search strategy, including the time element allows them to find studies that match the same duration or follow-up periods. This leads to stronger synthesis of evidence and more accurate conclusions in an evidence-based practice project or a nursing capstone assignment.
Ultimately, integrating the time frame into a PICOT question transforms it from a general inquiry into a focused, measurable, and applicable research question. It gives nurses a clear sense of direction in assessing intervention effectiveness, supports consistent data collection, and ensures that findings are both clinically relevant and timely. In nursing practice, such precision strengthens decision-making and enhances patient outcomes, making time an indispensable element in every well-crafted PICOT question.
Examples of PICOT Questions in Nursing
PICOT questions turn clinical uncertainty into a focused research question that can be answered with relevant evidence. Below are practical, well-built PICOT question examples across common nursing areas—chronic conditions, mental health, pediatrics—and an explanation of how these focused clinical questions guide evidence-based practice and the research process.
What Are Some Examples of PICOT Questions Focused on Chronic Conditions?
- In adults with hypertension (P), does home blood pressure monitoring with nurse follow-up (I), compared to usual clinic monitoring (C), reduce mean systolic blood pressure (O) over 6 months (T)?
- In patients with type 2 diabetes (P), does a nurse-led structured self-management program (I), compared to standard discharge teaching (C), reduce HbA1c (O) at 3 months (T)?
- In older adults with chronic heart failure (P), does daily telemonitoring of weight and symptoms (I), versus standard outpatient follow-up (C), reduce 30-day readmission rates (O) over 12 months (T)?
- Among patients with chronic obstructive pulmonary disease (COPD) (P), does a home-based pulmonary rehabilitation program (I), compared with usual care (C), improve 6-minute walk distance and quality-of-life scores (O) at 8 weeks (T)?
- In adults with type 1 diabetes (P), does continuous glucose monitoring plus nurse coaching (I), compared to self-monitoring of blood glucose (C), reduce time-in-range and mean blood glucose (O) over 6 months (T)?
- In patients with chronic low back pain (P), does a combined graded exercise and cognitive behavioral program (I), compared with opioid therapy alone (C), reduce pain scores and opioid use (O) after 12 weeks (T)?
- In patients with chronic kidney disease stage 3–4 (P), does nurse-led medication reconciliation and education (I), compared to usual nephrology follow-up (C), slow eGFR decline (O) over 12 months (T)?
- Among adults with type 2 diabetes (P), does adding a nurse-driven foot care clinic (I), versus standard outpatient advice (C), reduce incidence of foot ulcers (O) over 1 year (T)?
- In patients with rheumatoid arthritis (P), does a nurse-led adherence intervention (I), compared to routine care (C), improve medication adherence and reduce disease activity scores (O) at 6 months (T)?
- In obese adults with metabolic syndrome (P), does a nurse-coordinated lifestyle intervention (I), compared with printed materials alone (C), produce greater weight loss and improved fasting glucose (O) at 6 months (T)?
- In patients with chronic hepatitis C (P), does nurse navigator support for treatment initiation (I), versus standard referral (C), increase treatment uptake and sustained virologic response (O) at 12 months (T)?
- Among patients with chronic wound (P), does negative pressure wound therapy (I), compared to standard dressing changes (C), increase wound healing rate (O) at 12 weeks (T)?
- In adults with peripheral arterial disease (P), does supervised exercise therapy plus nurse counseling (I), compared to usual care (C), improve pain-free walking distance (O) at 16 weeks (T)?
- In patients with chronic migraine (P), does nurse-delivered self-management education (I), compared to medication optimization alone (C), reduce monthly headache days (O) at 3 months (T)?
- Among patients with hypertension and poor adherence (P), does a SMS reminder program plus nurse follow-up (I), compared to no reminders (C), improve medication adherence and blood pressure control (O) at 3 months (T)?
- In adults with COPD at risk of exacerbation (P), does a post-discharge nurse home visit program (I), compared to standard follow-up (C), reduce emergency visits for exacerbation (O) within 90 days (T)?
How Can PICOT Questions Address Mental Health Issues in Nursing?
- In adults with major depressive disorder (P), does nurse-coordinated telephone follow-up with brief counseling (I), compared to usual outpatient follow-up (C), reduce depression severity (O) over 6 months (T)?
- Among adolescents with anxiety disorders (P), does school-based CBT delivered by trained nurses (I), versus referral to external services (C), reduce anxiety scores and school absenteeism (O) at 12 weeks (T)?
- In postpartum women with mild-to-moderate depression (P), does nurse-led home-visit counseling (I), compared to standard postpartum care (C), reduce depressive symptoms at 6 weeks postpartum (O) (T)?
- In adults with PTSD (P), does a nurse-facilitated trauma-informed group therapy (I), compared with individual outpatient referral (C), reduce PTSD symptom severity (O) at 12 weeks (T)?
- In older adults with dementia exhibiting behavioral disturbances (P), does a nurse-implemented non-pharmacologic behavioral program (I), versus usual pharmacologic management (C), reduce agitation episodes (O) over 8 weeks (T)?
- In young adults with substance use disorder (P), does nurse-led motivational interviewing plus referral (I), compared with standard referral alone (C), increase treatment engagement and reduce substance use (O) at 3 months (T)?
- Among adolescents at risk of self-harm (P), does a brief nurse-delivered safety planning intervention (I), compared to routine discharge instructions (C), reduce repeat self-harm attempts (O) within 6 months (T)?
- In patients with schizophrenia newly discharged (P), does a nurse case management program (I), versus standard outpatient follow-up (C), reduce rehospitalization (O) over 12 months (T)?
- In university students with stress and mild anxiety (P), does an app-supported nurse coaching program (I), compared with informational pamphlets (C), reduce perceived stress and improve functioning (O) at 8 weeks (T)?
- Among veterans with comorbid depression and chronic pain (P), does integrated nurse-led collaborative care (I), compared to usual care (C), improve depression scores and pain outcomes (O) at 6 months (T)?
- In adults with bipolar disorder (P), does nurse-facilitated psychoeducation plus medication monitoring (I), versus medication monitoring alone (C), reduce mood episode frequency (O) at 12 months (T)?
- In adolescents with eating disorders (P), does nurse-led family education and follow-up (I), compared to standard outpatient referral (C), improve weight restoration and psychological measures (O) at 6 months (T)?
- Among patients with chronic insomnia (P), does nurse-delivered CBT for insomnia (I), compared to sleep hygiene advice (C), improve sleep efficiency and daytime function (O) over 8 weeks (T)?
- In adults with severe mental illness (P), does a nurse-coordinated transition program at discharge (I), versus usual discharge planning (C), improve outpatient appointment attendance and reduce relapse (O) within 90 days (T)?
- In caregivers of patients with dementia (P), does a nurse-led support and education group (I), compared to no group support (C), reduce caregiver burden and depressive symptoms (O) at 3 months (T)?
- In patients with PTSD receiving primary care (P), does nurse-administered brief CBT (I), compared with referral to specialty services (C), reduce symptom severity and improve function (O) at 12 weeks (T)?
What Examples of PICOT Questions Are Relevant to Pediatric Nursing?
- In premature infants (P), does kangaroo mother care with structured nursing support (I), compared to standard incubator care (C), increase weight gain and reduce length of stay (O) by discharge (T)?
- In school-age children with asthma (P), does a nurse-led inhaler technique and action-plan education program (I), compared to written instructions only (C), reduce ER visits and improve control scores (O) at 3 months (T)?
- Among infants at risk for neonatal hypoglycemia (P), does early breastfeeding support plus nurse lactation consult (I), versus routine feeding protocols (C), reduce hypoglycemic episodes (O) in the first 72 hours (T)?
- In children with type 1 diabetes (P), does a nurse-led peer support and education program (I), compared with standard clinic education (C), improve HbA1c and self-management skills (O) at 6 months (T)?
- In toddlers receiving routine immunizations (P), does a nurse-administered distraction and comfort protocol (I), as opposed to standard preparation (C), reduce observed pain scores and distress (O) immediately post-vaccination (T)?
- In children with moderate dehydration from gastroenteritis (P), does nurse-led oral rehydration protocol with parent education (I), vs IV rehydration standard (C), reduce hospital admissions and improve hydration markers (O) within 24 hours (T)?
- Among neonates in the NICU (P), does nurse-implemented developmental care (I), compared to standard care (C), improve neurobehavioral scores at term-equivalent age (O) (T)?
- In children undergoing elective surgery (P), does preoperative nurse-led preparation and play therapy (I), versus routine preop information (C), reduce preoperative anxiety and postoperative pain scores (O) on day 1 (T)?
- In adolescents with obesity (P), does a school-based nurse-led lifestyle intervention (I), compared with usual school health curriculum (C), reduce BMI percentile and improve fitness (O) at 12 months (T)?
- Among infants born to mothers with gestational diabetes (P), does nurse-directed early breastfeeding support (I), versus standard postpartum care (C), reduce neonatal hypoglycemia and improve breastfeeding rates (O) at discharge (T)?
- In children with eczema (P), does a nurse-delivered skin care education program (I), compared to routine advice (C), reduce flare frequency and improve quality of life (O) at 3 months (T)?
- In hospitalized children with cystic fibrosis exacerbation (P), does nurse-coordinated airway clearance scheduling (I), versus ad-hoc scheduling (C), shorten length of stay and reduce readmission (O) during hospitalization and 30 days post (T)?
- In infants exposed to maternal substance use (P), does a nurse-led neonatal abstinence syndrome (NAS) non-pharmacologic care bundle (I), compared to standard pharmacologic escalation (C), reduce pharmacologic treatment need and length of stay (O) by discharge (T)?
- In children with attention deficit hyperactivity disorder (ADHD) (P), does a nurse-delivered behavioral parent training (I), compared to usual care (C), improve behavior ratings and school performance (O) at 6 months (T)?
- In schoolchildren at risk for dental caries (P), does a nurse-supervised fluoride varnish program (I), compared to no school program (C), reduce caries incidence (O) over 12 months (T)?
- In adolescents with adolescent depression (P), does a nurse-facilitated school counseling referral pathway (I), versus standard teacher referral (C), improve timely access to care and depressive symptom reduction (O) at 3 months (T)?
How Do PICOT Questions Guide Evidence-Based Practice in Nursing?
A clear PICOT question is the first step in a rigorous search strategy and the backbone of evidence-based nursing practice. Here’s how PICOT drives the process:
- Focuses the search and improves relevance. Deriving keywords directly from PICOT elements (population, intervention, comparison, outcome, time) produces targeted database queries and efficient use of libguides and research guides at university libraries. This reduces time spent sifting through unrelated studies and helps retrieve relevant evidence faster.
- Aligns question with research design. A PICOT that asks whether an intervention is better than standard care points toward experimental designs (randomized trials or quasi-experimental studies), while questions about diagnosis or prognosis suggest diagnostic accuracy or cohort studies. This match improves the quality of evidence selected for review.
- Defines measurable outcomes. PICOT forces the selection of patient-centered, measurable endpoints (blood pressure control, blood glucose, validated pain scores) so that findings can be translated into patient care metrics and audited over time.
- Clarifies comparisons for practice change. By stating whether the comparison is usual care, placebo, or no intervention, PICOT helps stakeholders evaluate the practical value and feasibility of adopting a new nursing intervention in routine practice.
- Supports teaching and scholarship. For nursing students and clinicians writing a research paper or completing a nursing research assignment, PICOT provides a reproducible framework for generating literature searches, critiquing study methods, and synthesizing evidence for clinical recommendations.
- Enables measurable practice improvement. When a PICOT-driven intervention is implemented, outcomes defined by the question (e.g., reduced emergency visits, improved blood pressure control, reduced the future risk of complications) provide objective measures to evaluate success and inform policy or protocol changes.
Developing Your Own PICOT Questions
Turning a clinical problem into a strong PICOT question is a skill every nurse needs for evidence-based practice and nursing research. A well-formulated PICOT question narrows the scope of inquiry, makes outcomes measurable, directs an efficient search strategy, and links bedside observations to rigorous evidence. The guidance below walks you through concrete steps to create your own PICOT questions and shows how clinical experience directly shapes meaningful, practice-relevant research questions.
What Steps Should You Follow to Create a PICOT Question?
- Start with a clear clinical problem or observation.
Note a recurrent issue in patient care—for example, unstable blood pressure readings in a clinic population, frequent catheter-associated infections on a ward, or poor postoperative pain control in an orthopaedic unit. This real-world clinical problem becomes the seed for your research question. - Refine the problem into a focused clinical question.
Translate the observation into a concise clinical question: “What can we change to improve X for Y patients?” Avoid vague phrasing. Focus on a problem that is actionable in nursing practice. - Map the elements to PICOT.
Break the focused question into P (Population), I (Intervention), C (Comparison), O (Outcome), T (Time). Use precise descriptors (age, diagnosis, setting) for Population; clearly define the Intervention (dose, frequency, delivery); specify a realistic Comparator (standard care, placebo, no intervention); choose patient-centered, measurable Outcomes; and add a feasible Timeframe. Example mapping:- P = adults with hypertension attending a community clinic
- I = nurse-led home blood pressure monitoring + education
- C = usual clinic-based monitoring
- O = proportion achieving target BP and mean systolic change
- T = 6 months
- Make outcomes measurable and relevant.
Select validated measures—HbA1c, numeric pain rating, systolic BP, readmission rate, validated anxiety scale—so your PICOT question yields data that are clinically meaningful. Define what constitutes a clinically significant change (e.g., “≥10 mm Hg systolic reduction”). - Assess feasibility and scope.
Consider resources, sample size, ethical constraints, and timeline. For a student research paper or quality improvement, a narrower P or shorter T may be necessary. For larger clinical research, broader populations and longer follow-up may be viable. - Check the literature and refine the question.
Use your PICOT elements to build a search strategy—keywords and Boolean strings—from the P, I, C, O, and T. Consult research guides or libguides at your university to find relevant systematic reviews, trials, or practice guidelines. If evidence is abundant, refine the question (narrow population, specify intervention details); if scarce, the question may be worth pursuing as original nursing research. - Align study design with the question.
An intervention PICOT often points to randomized controlled trials or quasi-experimental designs; diagnostic or predictive PICOTs may require diagnostic accuracy studies or cohort designs. Matching design to question improves the likelihood that evidence will answer your clinical concern. - Engage stakeholders and consider ethics.
Discuss the PICOT with unit leaders, fellow nurses, patients where appropriate, and institutional review processes. If the comparator involves withholding an effective intervention (e.g., placebo), evaluate ethical implications and feasibility. - Draft and test the question.
Write the final PICOT question in one sentence and test it: can you extract keywords for a search? Would the question guide data collection? Is it specific enough to inform a protocol or audit? - Document and prepare to implement.
Use a PICOT worksheet or table (columns P/I/C/O/T) to keep elements clear for grant applications, assignments, or quality improvement plans.
How Can Clinical Experience Inform Your PICOT Question Development?
Clinical experience is the source of the most relevant and high-impact PICOT questions. Nurses who spend time at the bedside are uniquely positioned to notice patterns, safety gaps, and practice variations that matter to patients and teams. Here’s how to use that experience intentionally:
- Identify recurring clinical problems. Pattern recognition—frequent falls on a unit, persistent uncontrolled blood sugar in a subpopulation, or prolonged ventilator days in ICU patients—signals areas where a PICOT question can drive practice improvement.
- Use real cases to define the Population. Concrete cases help you specify inclusion criteria. “Patients recently discharged after heart failure exacerbation who live alone” is more actionable than “heart failure patients.”
- Shape interventions from feasible practice changes. Interventions born from experience—nurse-led discharge calls, a new wound-care protocol, bedside education—are more likely to be sustainable and studied in real clinical contexts.
- Select outcomes that matter to patients and staff. Clinical experience informs which outcomes are meaningful—reduced pain scores, fewer readmissions, quicker time to ambulation—rather than academic measures that lack bedside relevance.
- Estimate realistic time frames. Experience tells you whether an effect could be seen in days, weeks, or months. For example, ICU sedation protocols may impact ventilator days within hospitalization; lifestyle interventions require months.
- Anticipate practical barriers and confounders. Nurses can foresee adherence issues, staffing constraints, and comorbidities that affect study design and measurement, allowing the PICOT to be crafted to control or measure these factors.

Challenges in Formulating PICOT Questions
Developing a strong PICOT question is one of the most important yet challenging steps in nursing research and evidence-based practice (EBP). The PICOT format helps nurses convert broad clinical problems into focused, answerable research questions that guide decision-making and improve patient care. However, many nursing students and clinicians encounter difficulties when trying to structure their questions using the PICO framework. Understanding these challenges—and knowing how to overcome them—is essential for ensuring clarity, accuracy, and clinical relevance in nursing practice.
What Common Mistakes Do Nurses Make When Creating PICOT Questions?
One of the most common mistakes in formulating a PICOT question is being too general or unfocused. A vague clinical question such as “Does exercise help hypertension?” lacks measurable outcomes, comparison, or time frame. Using the PICOT format refines this to: In adults with hypertension (P), does a nurse-led exercise program (I), compared to standard care (C), improve blood pressure control (O) over three months (T)? This structured nursing PICOT question is specific, measurable, and relevant to evidence-based nursing.
Another common error involves mixing multiple outcomes in one research question. For instance, trying to evaluate both “pain relief and emotional well-being” in a single PICOT question can confuse the study design. Each well-built PICO question should focus on one clear, measurable outcome to guide the research process effectively.
Nurses also frequently forget to identify a valid comparison. The comparison element (C)—such as “standard care,” “no intervention,” or “placebo”—is essential for understanding whether the intervention being studied offers any benefit. Without this, the question remains incomplete and limits the ability to perform a sound clinical research study.
Another mistake occurs when nurses choose non-measurable or subjective outcomes. For example, “better well-being” or “improved lifestyle” cannot be reliably measured. Instead, outcomes should be quantifiable—such as reduced blood glucose, lower blood pressure, or improved wound healing. Similarly, neglecting to include a realistic time frame can make the question too broad. For example, monitoring blood sugar changes after a week may be too short, while five years might be impractical for a small nursing research assignment.
Lastly, many nursing students struggle with identifying a feasible population. A nursing PICOT question must define a realistic population, such as elderly patients with chronic pain, pregnant women at risk of hypertension, or patients with type 2 diabetes—populations that nurses frequently encounter in clinical settings. Overly narrow or overly broad populations make it difficult to collect relevant data or draw conclusions applicable to nursing practice.
How Can You Overcome Barriers in Developing Your PICOT Questions?
To overcome these barriers, nurses must integrate both clinical experience and the structured logic of the PICOT framework. The process begins with identifying a clinical problem observed in everyday patient care—for example, poor adherence to medication among patients with chronic hypertension, or increased anxiety in mechanically ventilated ICU patients. Using research guides and libguides at university libraries helps nurses locate existing studies, refine the search strategy, and develop good PICOT questions aligned with available evidence.
Collaboration also plays a key role. Engaging with mentors, preceptors, and faculty members allows nursing students to test whether their PICOT question is both relevant and feasible. For instance, a student may want to explore whether psychological intervention compared to standard care can reduce anxiety among patients awaiting cardiac surgery. Feedback from clinical supervisors ensures that such questions are realistic and ethically sound.
Another strategy involves using measurable and clinically meaningful outcomes. Nurses should consider data such as blood pressure readings, pain scores, or infection rates—objective metrics that can validate their evidence-based practice. For instance, a question like: In patients with chronic pain (P), does negative pressure wound therapy (I), compared to usual care (C), reduce pain scores (O) within two weeks (T)? is both practical and measurable.
Finally, time management and feasibility are critical. Selecting appropriate study durations—such as three months for blood glucose monitoring or six weeks for postpartum recovery—ensures that outcomes are observable within a reasonable clinical period. Using the PICOT format to establish this timeline keeps the research focused and manageable.
What Strategies Can Help Ensure Clarity and Focus in Your Questions?
Ensuring clarity in a PICOT question begins with simplicity. Each component—Population, Intervention, Comparison, Outcome, and Time—must be clearly defined. Avoid long, complex phrasing or multiple variables. A well-built clinical question should be answerable, evidence-based, and directly linked to nursing practice.
Using the PICOT framework also ensures consistency when comparing studies and interventions. Nurses can easily search for relevant evidence, replicate findings, and apply them to evidence-based nursing practice. For instance, a PICOT question such as: In adolescents with type 1 diabetes (P), does a nurse-led educational program on blood glucose monitoring (I), compared to no intervention (C), improve blood sugar control (O) over six months (T)? allows for measurable analysis and improved health outcomes.
Another effective strategy is to rely on research guides at university or health sciences libraries. These resources provide structured templates, examples, and frameworks that simplify the research process for both students and professionals. They also help ensure that the nursing PICOT question is grounded in current literature and aligned with established evidence-based nursing standards.
Finally, nurses should always test their PICOT question against real-world applicability. A clear, focused PICO question is one that can be implemented in diverse care settings—such as the ICU, community health centers, or maternal health programs. A good PICOT question not only identifies a measurable outcome but also improves patient care by addressing real clinical challenges.
Conclusion
The PICOT framework stands as one of the most valuable tools in modern nursing research and evidence-based practice. It transforms vague or broad inquiries into structured, answerable clinical questions that directly inform nursing practice. By organizing thinking around Population, Intervention, Comparison, Outcome, and Time, nurses can better identify gaps in care, evaluate interventions, and apply relevant evidence to improve patient care across various settings—from acute care and the ICU to community health and maternal care programs.
A well-developed PICOT question not only enhances the precision of a research design but also strengthens the link between research and clinical application. When nurses use the PICOT format to explore issues such as hypertension management, pain relief, or psychological interventions for patients with chronic illness, they are able to formulate measurable and meaningful research questions that reflect real-world challenges. Whether comparing oxygen therapy compared to standard care, assessing wound healing outcomes using negative pressure wound therapy, or evaluating blood sugar levels in patients with type 2 diabetes, the PICO framework ensures that each question aligns with evidence-based nursing principles.
Moreover, PICOT questions cultivate critical thinking and scientific reasoning among nursing students and practitioners. They guide the research process, inform search strategies using research guides and libguides, and ensure that evidence-based nursing practice is not based on intuition but on systematically gathered and analyzed data. Through this structured approach, nurses gain the ability to identify the most effective interventions, compare outcomes across patient groups, and develop new standards for nursing care.
Ultimately, mastering the PICOT question format is about more than academic precision—it is about elevating the quality of patient care. The PICOT framework empowers nurses to make decisions rooted in evidence, reduce the risk of errors, and achieve measurable improvements in health outcomes. In an era where clinical research drives healthcare innovation, the ability to formulate and apply strong PICOT questions remains central to advancing both nursing practice and the broader goals of evidence-based practice in the health sciences
Frequently Asked Questions
What are examples of clinical questions in nursing?
Examples of clinical questions in nursing include:
- In adult surgical patients, does early ambulation compared to bed rest reduce the incidence of postoperative pneumonia?
- Among elderly patients in long-term care, how does a high-protein diet compared to a regular diet affect wound healing?
- In patients with chronic pain, does mindfulness-based therapy compared to opioid treatment improve pain control and quality of life?
These questions guide evidence-based investigations and help nurses make informed clinical decisions that improve patient outcomes.
Which question would be an example of PICOT used by nurses to obtain the best evidence-based practice?
An example of a PICOT question used by nurses for evidence-based practice is:
- In adult ICU patients (P), how does the use of daily sedation interruption (I) compared to continuous sedation (C) affect the duration of mechanical ventilation (O) over a two-week period (T)?
This question applies the PICOT framework to determine the most effective intervention based on measurable outcomes and a defined timeframe.
What is an example of a PICO question for nursing shortage?
An example of a PICO question addressing the nursing shortage is:
- In hospital units experiencing staffing shortages (P), how does the use of flexible scheduling and incentive programs (I) compared to traditional fixed shifts (C) affect nurse retention rates and job satisfaction (O) over six months (T)?
This question explores how staffing strategies influence workforce stability and quality of patient care.
What is the PICOT question for nurse staffing?
A strong PICOT question for nurse staffing might be:
- In acute care hospitals (P), how does maintaining optimal nurse-to-patient ratios (I) compared to higher workloads (C) influence patient safety outcomes, such as medication errors and fall rates (O), over a one-year period (T)?
This example demonstrates how the PICOT model helps identify relationships between staffing levels and patient outcomes, supporting evidence-based staffing policies in nursing practice.
