SOAP Note Example Nurse Practitioner
Here’s a SOAP Note Example Nurse Practitioner to help you chart your SOAP Note for NP School
Subjective:
CC (chief complaint): 42-year-old Caucasian male, Pt states the judge ordered him to get a psych eval after receiving a charge for aggravated assault. Pt defended himself when someone pulled a gun out on him. Pt feels he has no issues mentally. Pt feels he should be able to defend himself. Pt says he doesn’t deserve what happened. Pt is having nightmares and struggling with sleep since being out. He states he is doing better now. Pt experienced the trauma of losing his best friend (dog) when he was in jail. Pt reports not being able to sleep, only getting 2-3 hrs, and having difficulty getting back to sleep. He says he has racing thoughts and “tons” of anxiety.
HPI: Pt went to jail for five months. Pt feels he’s been done wrong. Pt says it’s really scary there, and he’s never seen anything like it before. Pt states his family thinks he may have PTSD now after.
Substance Current Use: Patient reports stopped alcohol, last use six months ago, stopped marijuana because it makes him more anxious. Denies any other illicit drug use.
Medical History:
- Current Medications: Not currently taking any medications
- Allergies:None reported
- Reproductive Hx:N/A
ROS:
- GENERAL: No fevers, sweats, shakes, chills, or change in weight
- HEENT: 20/20 vision no report of vision changes. No epistaxis or tinnitus
- SKIN: Denies rashes or itching
- CARDIOVASCULAR: No edema, chest pain, or palpitations
- RESPIRATORY: Denies shortness of breath, cough, wheezing, or sputum
- GASTROINTESTINAL: No anorexia, nausea, vomiting, or diarrhea. No abdominal pain or blood
- GENITOURINARY: Denies frequency, nocturia, dysuria, or hematuria
- NEUROLOGICAL: Denies any focal neurologic complaints
- MUSCULOSKELETAL: No joint swelling, stiffness, pain or myalgias
- HEMATOLOGIC: No abnormal prolonged bleeding or bruising
- LYMPHATICS: No enlarged nodes
- ENDOCRINOLOGIC: Denies excessive thirst, urination, heat or cold intolerance, diabetes or thyroid disease
Objective:
Diagnostic results: No labs, X-rays, or other diagnostics are needed to develop the differential diagnoses at this time. Will follow up with labs before the next appointment.
Assessment:
Mental Status Examination: The patient’s Appearance: Neatly Groomed, Appears Stated Age: Yes, Gait is normal, Behavior: Calm, Eye Contact: Fair, Speech Rate: Normal, Tone: Normal, Mood: Euthymic, Affect: Congruent, Thought Process: Linear, Thought Content: Delusions None, Suicide Ideation: None, Homicidal Ideation: None, Perceptual Disturbances: Auditory- none, Visual- none, Insight: Good, Judgement: Good, Fund of Knowledge: Good, Memory: Good, Cognition: Alert, Oriented to self, place, situation, date.
Diagnostic Impression:
The patient presents with symptoms indicative of a complex psychological response to recent traumatic experiences. The diagnostic impression includes Generalized Anxiety Disorder (GAD), Post-Traumatic Stress Disorder (PTSD), and Major Depressive Disorder (MDD). The patient’s chief complaint, coupled with the reported symptoms, supports the consideration of these three diagnoses.
F43.10 Post-Traumatic Stress Disorder (PTSD) (confirmed):
The confirmed diagnosis is PTSD. The patient’s exposure to traumatic events, including aggravated assault, incarceration, and loss of a close companion, his dog), aligns with the criteria for PTSD. The patient’s nightmares, sleep disturbances, anxiety, and persistent distress are consistent with the hallmark features of PTSD (Bryant, 2019). The traumatic experience in jail and the subsequent development of symptoms, including hypervigilance, racing thoughts, and difficulty sleeping, strongly suggest PTSD as the primary diagnosis.
Differential Diagnoses:
- F41. 1 Generalized Anxiety Disorder (GAD):
The patient indicates signs of anxiety, including racing thoughts, sleep disturbances (2-3 hours of sleep), nightmares, hypervigilance related to a traumatic event, and subjective feelings of fear and anxiety in response to experiences in jail (Mishra & Varma, 2023). While the patient does report significant anxiety symptoms, the specific trigger for the anxiety appears to be trauma-related, stemming from the assault and incarceration. The intensity and nature of anxiety align more closely with the criteria for PTSD rather than GAD.
- F32. 9 Major Depressive Disorder (MDD):
The patient indicates signs of Major Depressive Disorder (MDD), reporting feelings of not deserving what happened and struggling with sleep, suggesting disturbances in mood and sleep patterns (Christensen et al., 2020). Although the patient reports feelings of not deserving what happened and struggles with sleep, the prominent feature appears to be the trauma-related symptoms and nightmares indicative of PTSD. The depressive symptoms do not seem to be the primary focus, making MDD less likely as the principal diagnosis.
Rationale for Diagnosis
The patient’s symptomatology aligns most closely with the criteria for PTSD. The traumatic events in the patient’s recent history, coupled with the reported nightmares, anxiety, and impaired sleep, are consistent with the diagnostic criteria for PTSD. The patient’s mental status examination reveals signs of distress, including fair eye contact and the presence of anxiety-related symptoms. Although GAD and MDD symptoms are present to some extent, they are secondary to the traumatic stressor, reinforcing the primary diagnosis of PTSD. The patient’s insight, judgment, and cognitive functioning remain intact, supporting the differentiation from other possible mental health conditions.
Reflections:
I largely agree with the preceptor’s assessment and diagnostic impression of PTSD. The patient’s narrative, coupled with the mental status examination, provides a compelling case for trauma-related distress. The alignment of symptoms with the criteria for PTSD, including nightmares, anxiety, and impaired sleep, supports this diagnosis. The recognition of the patient’s insight and cognitive functioning being intact reinforces the specificity of PTSD as the primary concern. The differentiation of GAD and MDD highlights the importance of a nuanced understanding of mental health presentations.
From this case, I have learned the significance of exploring the contextual factors surrounding a patient’s symptoms. The legal and ethical considerations extend beyond confidentiality and consent, delving into the complex interplay between legal issues, trauma, and mental health. Understanding the social determinants of health is crucial, as the patient’s traumatic experience, legal entanglements, and socioeconomic background contribute to the complexity of the case (Deferio et al., 2019). In terms of what I would do differently, I would enhance my exploration of the patient’s cultural background and its potential impact on his perception of the traumatic events. Additionally, incorporating a more comprehensive assessment of the patient’s support system and resources could provide valuable insights into potential avenues for intervention and support.
Considering health promotion and disease prevention, a holistic approach that addresses not only the psychiatric symptoms but also the social determinants of health is essential. Collaborating with legal professionals to ensure the patient’s rights and well-being are protected is crucial. Furthermore, tailoring interventions to the patient’s age, ethnic group, and socioeconomic factors can enhance treatment efficacy and promote long-term mental well-being (Beck et al., 2021). In future cases, I will continue to refine my ability to integrate legal and ethical considerations, cultural competence, and a comprehensive understanding of social determinants into the assessment and treatment planning process.
How to Write a SOAP Note: Nurse Practitioner Guide
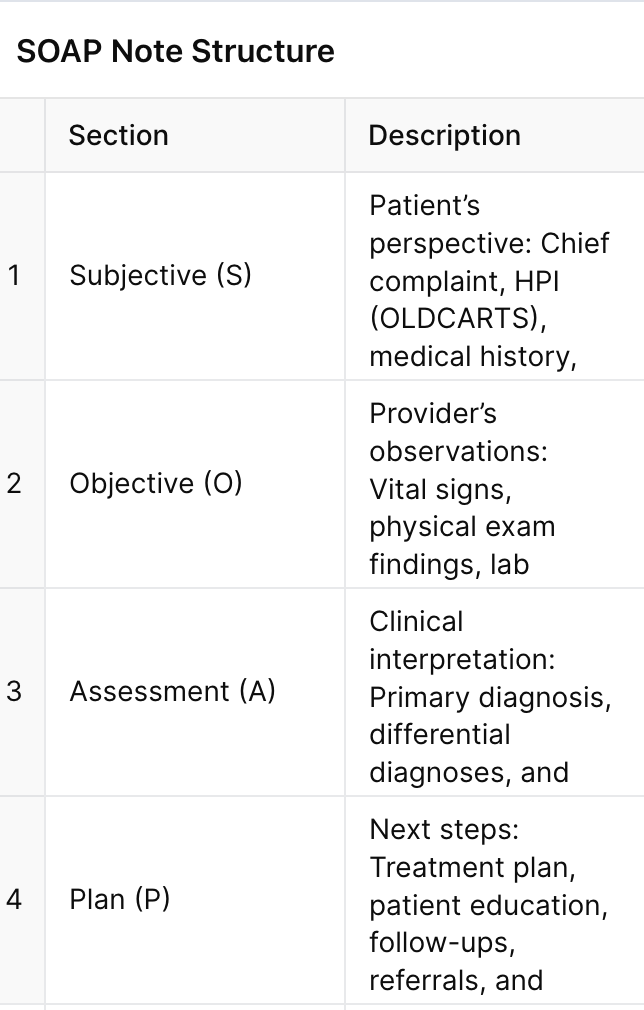
1. Subjective (S)
- Chief Complaint (CC): Start with the patient’s own words (e.g., “I have chest pain”).
- History of Present Illness (HPI): Use OLDCARTS (Onset, Location, Duration, Characteristics, Aggravating/Relieving factors, Timing, Severity) to structure symptom details 9.
- Past Medical/Surgical History: Include only relevant conditions (e.g., diabetes for a foot ulcer case).
- Medications/Allergies: List current prescriptions and reactions.
- Social History: Note smoking, alcohol, occupation, or stressors 610.
2. Objective (O)
- Vital Signs: BP, HR, RR, Temp, SpO2, BMI.
- Physical Exam:
- System-based findings (e.g., “Lungs: Clear to auscultation bilaterally”).
- Diagnostics: Lab results, imaging, or point-of-care tests (e.g., “Rapid Strep: Negative”) 28.
3. Assessment (A)
- Diagnosis: Prioritize the primary issue (e.g., “Back Pain Soap Note, J45.901″).
- Differentials: List ruled-out conditions (e.g., “GERD vs. angina”).
- Clinical Reasoning: Explain why the diagnosis fits (e.g., “Wheezing and peak flow decline support asthma exacerbation”) 411.
4. Plan (P)
- Treatment: Medications (name, dose, duration), therapies, or procedures.
- Education: Diet, activity modifications, warning signs (e.g., “Return if fever >102°F”).
- Follow-Up: Timeline for re-evaluation (e.g., “Recheck HbA1C in 3 months”).
- Referrals: Specialists or support services (e.g., “Cardiology consult”) 513.
Key Tips for Effective SOAP Notes
Legal Safeguards: Document thoroughly to support billing and avoid malpractice risks
Use Structured Frameworks: OLDCARTS for HPI and system-based exams for objectivity 9.
Avoid Jargon: Write clearly for interdisciplinary teams (e.g., “No accessory muscle use” instead of “No AMU”).
Be Concise: Omit irrelevant details (e.g., childhood allergies in a UTI case).
Update Plans: Adjust follow-ups or medications in subsequent notes 8.
