Sleep Ergonomics SOAP Note Example
Patient Name: EC| Age: 32 | Gender: Female | Date: 2025-02-11
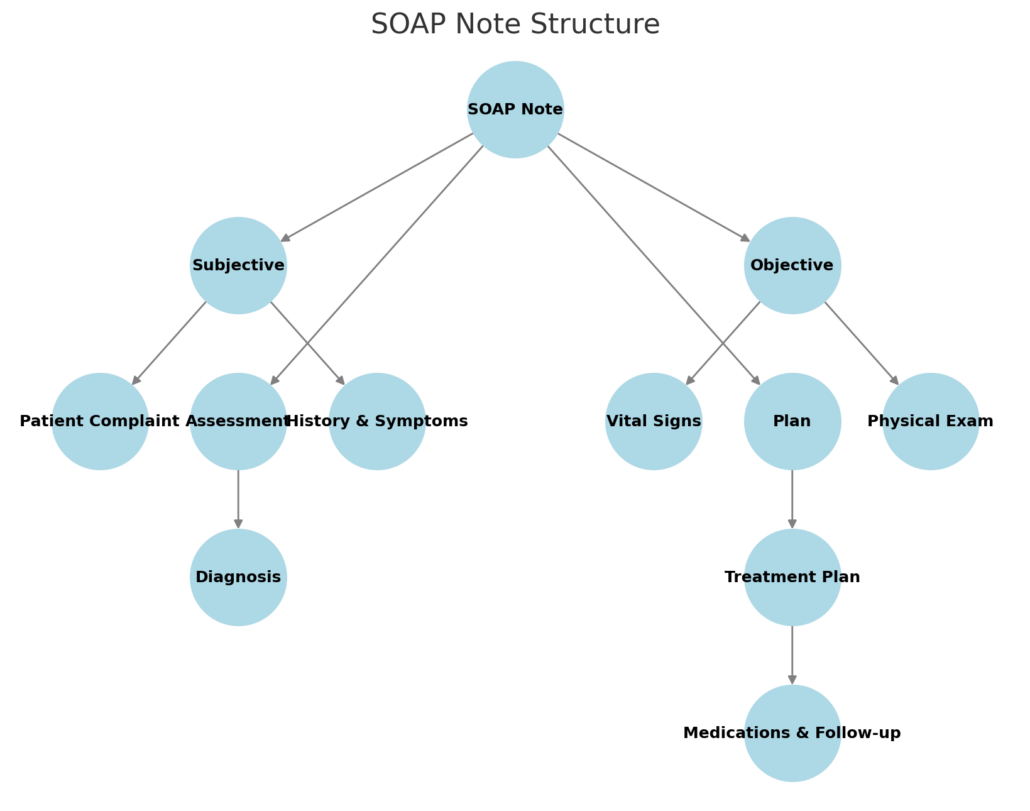
Subjective (S)
Chief Complaint (CC):
“I’ve had this nagging lower back pain for 2 months that’s worst in the mornings. It feels stiff and achy, and sometimes shoots down my left leg when I twist.”
History of Present Illness (HPI):
- Location: Lumbar spine (L4–L5 region), radiating intermittently to left posterior thigh.
- Onset: Gradual, worsening over 8 weeks.
- Character: Dull ache (4/10 at rest; 7/10 with movement).
- Timing: Peak intensity upon waking (6:00 AM). Improves slightly with heat and stretching.
- Exacerbating Factors: Prolonged sitting at work, side-sleeping with legs drawn upward.
- Associated Symptoms: Morning stiffness (~30 mins), occasional numbness in left foot.
- Medications: Ibuprofen 400 mg PRN (minimal relief).
- Allergies: NKDA.
Past Medical History:
- Anxiety (F41.9, diagnosed 2022, managed with mindfulness).
- Mild adolescent idiopathic scoliosis (M41.9, no treatment).
Social History:
- Occupation: Graphic designer (remote, 8–10 hrs/day at non-ergonomic workstation; Z56.82).
- Sleep Setup: 10-year-old soft mattress, sleeps in fetal position with 3 pillows (head elevated).
- Exercise: Sedentary (Z72.3); occasional yoga.
- Support System: Lives alone; limited social support for lifestyle changes.
Review of Systems (ROS):
- Musculoskeletal: Denies trauma, prior surgery, or joint swelling.
- Neurological: Denies bowel/bladder incontinence, weakness, or balance issues.
- Psychiatric: Reports mild anxiety (PHQ-4 score: 2/12) but denies depression or insomnia.
- Integumentary: No rashes or skin changes.
Objective (O)
Vital Signs:
- BP: 118/76 mmHg | HR: 68 bpm | Temp: 98.4°F | BMI: 28.6 (Overweight).
Physical Exam:
- General: No acute distress; antalgic gait noted when rising from seated position.
- Posture: Forward head posture, increased lumbar lordosis, asymmetric shoulder height (R > L).
- Range of Motion (Lumbar Spine):
- Flexion: 40° (limited by pain; normal: 60°).
- Extension: 15° (pain at end-range).
- Lateral Flexion: 20° bilaterally (mild discomfort).
- Palpation: Tenderness at L4–L5 paraspinals; taut bands in quadratus lumborum (myofascial trigger points).
- Neurological:
- Strength: 5/5 bilateral lower extremities (hip flexion, knee extension, ankle dorsiflexion).
- Sensation: Intact to light touch in L2–S1 dermatomes.
- Reflexes: 2+ patellar/Achilles bilaterally.
- Special Tests:
- Straight Leg Raise: Negative bilaterally.
- Faber Test: Negative for sacroiliac joint dysfunction.
- Kemp’s Test: Positive for facet joint irritation (pain on lumbar extension/rotation).
- Sleep Ergonomics Assessment:
- Mattress sagging (loss of lumbar support; visible depression in sleep surface).
- Pillow height excessive (cervical flexion >30°; contributes to forward head posture).
- Sleeps in fetal position (spinal flexion compression; exacerbates scoliotic curvature).
Assessment (A)
Primary Diagnosis
M54.50 (Low back pain, unspecified)
- Etiology: Multifactorial, including:
- Poor sleep ergonomics (Z72.3, R29.818): Non-supportive mattress/pillow setup contributing to spinal misalignment.
- Sedentary behavior (Z72.3): Prolonged sitting at a non-ergonomic workstation exacerbating postural strain.
- Scoliosis history (M41.9): Mild adolescent idiopathic scoliosis predisposing to asymmetric spinal loading.
Differential Diagnoses
- M54.59 (Other low back pain) – Myofascial Pain Syndrome (M79.1)
- Rationale for Consideration:
- Taut bands and trigger points identified in quadratus lumborum during palpation.
- Morning stiffness and localized tenderness align with myofascial patterns.
- Reason for Exclusion:
- Absence of trigger points in other key muscle groups (e.g., trapezius, gluteals).
- Symptoms improve with positional changes (unlikely isolated myofascial etiology).
- Rationale for Consideration:
- M51.37 (Lumbosacral disc degeneration)
- Rationale for Consideration:
- Chronic pain exacerbated by spinal flexion (fetal sleeping position).
- History of sedentary work, a risk factor for disc pathology.
- Reason for Exclusion:
- No radicular symptoms below the knee (e.g., no foot drop or dermatomal numbness).
- Negative straight leg raise (SLR) test; imaging not yet indicated.
- Rationale for Consideration:
- M53.3 (Sacrococcygeal disorders) – Sacroiliac Joint Dysfunction
- Rationale for Consideration:
- Pain radiation to posterior thigh mimics SI joint referral patterns.
- Sedentary occupation increases risk of SI joint hypomobility.
- Reason for Exclusion:
- Negative Faber/Patrick test.
- No localized tenderness over SI joint on palpation.
- Rationale for Consideration:
- M54.16 (Lumbar radiculopathy)
- Rationale for Consideration:
- Intermittent left leg pain with twisting movements.
- Mild foot numbness reported.
- Reason for Exclusion:
- No weakness or reflex deficits (5/5 strength, 2+ reflexes bilaterally).
- Sensation intact in L2–S1 dermatomes; negative SLR.
- Rationale for Consideration:
- F45.41 (Chronic pain syndrome with somatic symptoms)
- Rationale for Consideration:
- Overlap of anxiety history (F41.9) and chronic pain.
- Reason for Exclusion:
- Symptoms directly correlate with physical exam findings (taut bands, postural asymmetry).
- PHQ-4 score (2/12) does not support significant psychological component.
- Rationale for Consideration:
Contributing Factors
Biomechanical:
- Asymmetric spinal loading secondary to mild scoliosis (M41.9).
- Compromised lumbar range of motion (flexion/extension limited by pain).
Environmental:
- Non-ergonomic workstation (Z56.82): Lack of lumbar support, monitor below eye level.
- Poor sleep environment: Sagging mattress, excessive pillow height.
Behavioral:
- Sedentary lifestyle (Z72.3): Minimal physical activity exacerbating deconditioning.
- Poor sleep hygiene: Fetal position perpetuating spinal flexion.
Clinical Synthesis
The patient’s low back pain is most consistent with non-specific mechanical strain exacerbated by ergonomic stressors. Differential diagnoses were systematically ruled out through history, physical exam, and absence of “red flag” symptoms (e.g., radiculopathy, systemic illness). Contributing factors are modifiable, emphasizing the need for targeted ergonomic and behavioral interventions.
ICD-10 Codes:
- Primary: M54.50
- Secondary: Z72.3, R29.818, M41.9, Z56.82
Plan (P)
1. Therapeutics:
- Physical Therapy Referral:
- Focus: Core stabilization, postural correction, and ergonomic education.
- Evidence: 2023 AAOS guidelines recommend PT as first-line treatment for chronic low back pain.
- Manual Therapy:
- Soft tissue mobilization to lumbar paraspinals (2x/week for 4 weeks; J Orthop Sports Phys Ther 2022).
- Therapeutic Exercises (HEP):
- Bird-dog, dead bug (3 sets of 10 reps daily).
- Hamstring/hip flexor stretches (hold 30 sec, 3x/day).
2. Sleep Ergonomics Modifications:
- Mattress Replacement: Recommend medium-firm orthopedic mattress (studies show reduced morning stiffness; Sleep Med Rev 2021).
- Pillow Adjustment: Contoured cervical pillow to maintain neutral alignment (reduce cervical strain).
- Sleep Position: Trial semi-Fowler’s position with pillow under knees (aligns lumbar spine).
3. Activity Modification:
- Workstation Adjustments:
- Lumbar roll for chair (improves lordotic curve).
- Monitor riser to eye level (reduces forward head posture).
- Document ergonomic assessment with occupational therapist (interprofessional collaboration).
- Behavioral Strategies:
- Hourly standing/stretching breaks (5 mins/hour; set smartphone reminders).
4. Medications:
- Naproxen 500 mg BID x 7 days (maximizes anti-inflammatory effect; monitor renal function).
- Cyclobenzaprine 5 mg HS PRN (muscle relaxant; limit to 14 days due to sedation risk).
5. Follow-Up & Monitoring:
- 2-Week Follow-Up:
- Reassess pain scale, HEP adherence, and mattress replacement progress.
- If unresolved: Order lumbar X-ray (rule out structural abnormalities) and consider CBC/ESR (screen for inflammation).
- 6-Week Goal: Reduce pain to ≤3/10, improve lumbar flexion to 50°.
6. Health Promotion:
- Weight Management: Refer to dietitian for Mediterranean diet plan (target BMI <25).
- Stress Reduction: Mindfulness-based stress reduction (MBSR) classes (aligns with anxiety management).
7. Interprofessional Collaboration:
- Occupational Therapist: Workspace ergonomic evaluation.
- Pain Management Specialist: Consult if NSAIDs/PT fail.
ICD-10 Codes:
- Primary: M54.50 (Low back pain, unspecified)
- Secondary: Z72.3 (Sedentary lifestyle), R29.818 (Abnormal posture), M41.9 (Scoliosis), Z56.82 (Work-related ergonomic stress)
MSN-Level Clinical Reasoning
Evidence-Based Practice:
- Diagnostic Reasoning: Prioritized musculoskeletal etiologies over psychosomatic causes due to clear physical exam findings (taut bands, postural asymmetry).
- Pharmacology: Selected cyclobenzaprine over benzodiazepines due to lower addiction risk (per 2022 CDC guidelines).
Ethical/Legal Considerations:
- Informed Consent: Discussed risks/benefits of NSAID use (GI bleeding, renal strain).
- Scope of Practice: Collaborated with supervising physician for cyclobenzaprine prescription (state-specific NP regulations).
Patient-Centered Care:
- Cultural Competence: Addressed financial barriers to mattress replacement by providing budget-friendly retailer options.
Patient Education:
- Provided visual aids for sleep posture modifications and HEP exercises.
- Discussed long-term risks of untreated poor ergonomics (chronic pain, degenerative changes).
Signed:
[Your Name], MSN Student
Instructor Review: [Instructor’s Signature]
References:
- ICD-10-CM 2024 Updates (CMS).
- American Academy of Orthopaedic Surgeons (AAOS). (2023). Low Back Pain Clinical Guidelines.
- National Institute for Occupational Safety and Health (NIOSH). (2021). Ergonomics for Remote Workers.
- Journal of Orthopaedic & Sports Physical Therapy. (2022). “Manual Therapy for Lumbar Pain.”
- CDC. (2022). Guidelines for Prescribing Opioids and Muscle Relaxants.
Next Steps:
- Monitor patient’s pain journal submissions via EHR portal.
- Schedule interprofessional team huddle with PT/OT.
