Postmenopausal Bleeding SOAP Note Example
Patient Information:
- Name: Linda Martinez
- Age: 58
- Gender: Female
- Date of Evaluation: October 25, 2023
- MRN: [Insert MRN]
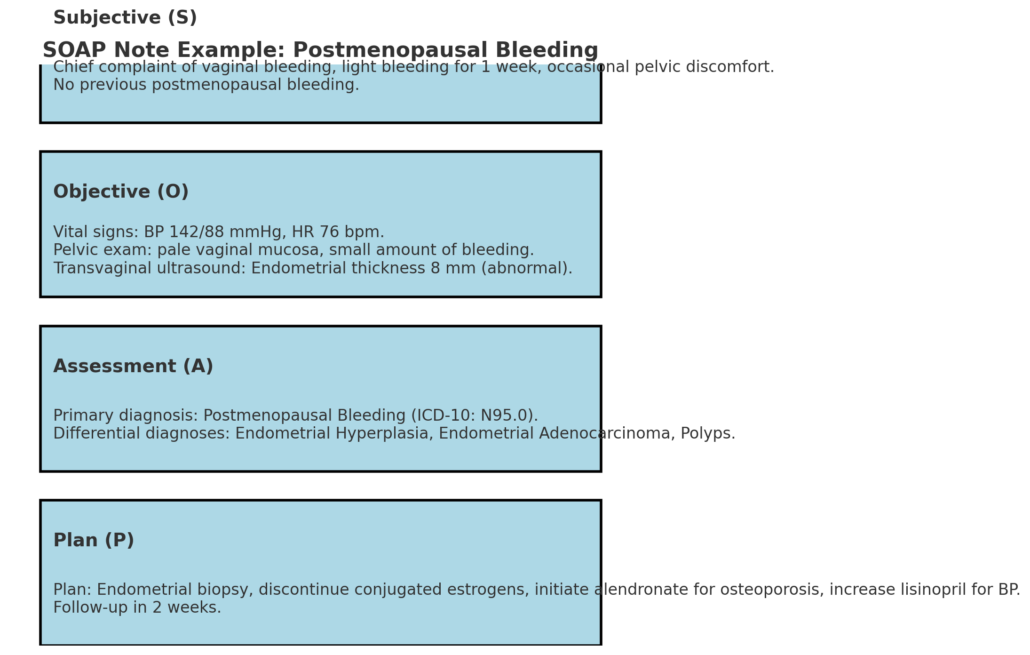
Subjective (S)
Chief Complaint (CC):
“I’ve had vaginal bleeding for the past week. I went through menopause 7 years ago, so this is really worrying me.”
History of Present Illness (HPI):
- Onset and Duration: The first episode of vaginal bleeding began 7 days ago; intermittent light bleeding requiring 1-2 pads/day
- Characteristics: Bright red blood without clots, described as significantly less than menstrual periods
- Associated Symptoms: Reports mild, non-localized pelvic discomfort (rated 2/10); denies dysuria, fever, abdominal pain, or changes in bowel habits
- Timing: No pattern to bleeding; occurs randomly throughout the day
- Exacerbating/Relieving Factors: None identified; no relation to physical activity
- Prior Episodes: No previous postmenopausal bleeding
- Last Normal Menstrual Period: Age 51 (7 years ago)
Medication History:
- Current Medications:
- Conjugated estrogens (Premarin) 0.625 mg oral daily, initiated 2 years ago for osteoporosis prevention
- Lisinopril 10 mg oral daily for hypertension (started 5 years ago)
- Calcium carbonate 600 mg with vitamin D 400 IU twice daily
- Multivitamin daily
- Medication Adherence: Reports taking medications as prescribed
- Recent Medication Changes: None in the past 6 months
- Over-the-Counter Medications: Occasional ibuprofen for joint pain
- Herbal/Supplements: None
Allergies:
No known drug allergies (NKDA)
Past Medical History:
- Chronic Conditions:
- Hypertension (ICD-10: I10) was diagnosed 6 years ago, well-controlled
- Osteoporosis (ICD-10: M81.0) diagnosed 2 years ago, T-score -2.7 at the lumbar spine
- Obesity (ICD-10: E66.9), BMI 32
- Past Surgical History:
- Hysteroscopic polypectomy (2018) for benign endometrial polyp
- Laparoscopic cholecystectomy (2010)
- Gynecological History:
- G3P2 (2-term vaginal deliveries, 1 spontaneous abortion)
- Menarche at age 13
- No history of abnormal Pap smears
- Last Pap smear: 1 year ago, normal
- No history of sexually transmitted infections
Family History:
- Mother: Endometrial cancer diagnosed at age 62, deceased at 70
- Father: Hypertension, myocardial infarction at age 72
- Sister: Type 2 diabetes, diagnosed at age 55
- Maternal aunt: Breast cancer at age 58
- No known genetic disorders
Social History:
- Marital Status: Married for 35 years
- Occupation: Retired elementary school teacher
- Tobacco Use: Never smoker
- Alcohol Use: 1-2 glasses of wine per week (occasional)
- Recreational Drug Use: Denies
- Exercise: Walks 20 minutes, 3 times weekly
- Diet: Reports high-carbohydrate diet, limited vegetable intake
- Living Situation: Lives with husband in a single-story home
- Sexual History: Sexually active with husband; denies dyspareunia
Review of Systems:
- Constitutional: Denies fever, chills, fatigue, unintentional weight loss or gain
- Cardiovascular: Denies chest pain, palpitations, or edema
- Respiratory: Denies cough, shortness of breath
- Gastrointestinal: Denies nausea, vomiting, abdominal pain, or changes in bowel habits
- Genitourinary: Reports postmenopausal bleeding as described; denies dysuria, frequency, urgency, or incontinence
- Gynecologic: Denies dyspareunia, vaginal discharge, or vulvar lesions; reports occasional vaginal dryness
- Musculoskeletal: Reports mild lower back pain, managed with occasional ibuprofen
- Neurological: Denies headaches, dizziness, syncope, or focal weakness
- Psychiatric: Denies anxiety, depression, or mood changes
- Endocrine: Denies polydipsia, polyuria, heat/cold intolerance
- Hematologic: Denies easy bruising or bleeding
- Immunologic: Denies recurrent infections
Objective (O)
Vital Signs:
- Blood Pressure: 142/88 mmHg (elevated)
- Heart Rate: 76 bpm (regular)
- Respiratory Rate: 16 breaths/min
- Temperature: 98.6°F (37.0°C)
- Oxygen Saturation: 98% on room air
- Height: 5’4″ (162.6 cm)
- Weight: 186 lbs (84.4 kg)
- BMI: 32 kg/m² (Class I Obesity)
Physical Examination:
- General Appearance: Well-developed, well-nourished female in no acute distress
- Head and Neck:
- Normocephalic, atraumatic
- Thyroid non-palpable, no lymphadenopathy
- Cardiovascular: Regular rate and rhythm, no murmurs, rubs, or gallops
- Respiratory: Clear to auscultation bilaterally, no wheezes or crackles
- Abdominal: Soft, non-tender, no hepatosplenomegaly or masses
- Extremities: No edema, normal peripheral pulses
Pelvic Examination:
- External Genitalia: Normal appearance, no lesions or masses
- Speculum Examination:
- Vaginal mucosa appears pale and atrophic with decreased rugae
- Small amount of bright red blood in vaginal vault
- Cervix: Multiparous, no lesions, polyps, or active bleeding
- Bimanual Examination:
- Uterus: Anteverted, normal size (8 cm), non-tender
- Adnexa: No masses or tenderness bilaterally
- No cervical motion tenderness
- Rectovaginal Examination:
- No masses or nodularity
- Rectal vault normal, no masses
- Stool guaiac negative
Diagnostic Studies:
- Imaging:
- Transvaginal Ultrasound (performed today):
- Endometrial thickness: 8 mm (abnormal for postmenopausal state; normal <4 mm)
- Uterus: 8.2 x 4.5 x 3.8 cm, normal contour
- No focal masses were identified within the endometrium
- Ovaries: Right ovary 2.1 x 1.8 x 1.5 cm; Left ovary 2.0 x 1.7 x 1.6 cm
- No adnexal masses or free fluid
- Urinary bladder normal
- Transvaginal Ultrasound (performed today):
- Laboratory Studies:
- Complete Blood Count (Today):
- WBC: 7.2 x 10³/μL (normal range: 4.5-11.0)
- Hemoglobin: 12.8 g/dL (normal range: 12.0-15.5)
- Hematocrit: 38.2% (normal range: 36.0-46.0)
- Platelets: 210 x 10³/μL (normal range: 150-450)
- Comprehensive Metabolic Panel (Today):
- Glucose: 92 mg/dL (normal range: 70-99)
- Creatinine: 0.8 mg/dL (normal range: 0.5-1.1)
- BUN: 15 mg/dL (normal range: 7-20)
- All other values within normal limits
- Pap Smear (Today):
- Specimen collected, pending results
- Previous Pap smear (1 year ago): Negative for intraepithelial lesion or malignancy
- HPV Testing (Today):
- Specimen collected, pending results
- TSH, Free T4 (Today):
- Pending results
- Endometrial Sampling:
- Pipelle endometrial biopsy scheduled within 48 hours
- Complete Blood Count (Today):
Assessment (A)
Primary Diagnosis:
- Postmenopausal Bleeding (ICD-10: N95.0)
- Evidenced by: Vaginal bleeding 7 years post-menopause, abnormal endometrial thickness (8 mm)
- Severity: Mild to moderate based on the amount of bleeding and normal hemoglobin
- Duration: 1 week
Differential Diagnoses:
- Endometrial Hyperplasia Without Atypia (ICD-10: N85.00)
- Supporting Evidence: Increased endometrial thickness (8 mm), use of unopposed estrogen therapy for 2 years
- Risk Factors: Obesity (BMI 32), unopposed estrogen use
- Diagnostic Considerations: Pending endometrial biopsy for confirmation
- Evidence-Based Reference: ACOG Practice Bulletin No. 149 (2015) notes that unopposed estrogen increases the risk of endometrial hyperplasia
- Endometrial Adenocarcinoma (ICD-10: C54.1)
- Supporting Evidence: Family history (mother with endometrial cancer), postmenopausal bleeding, endometrial thickness >4 mm
- Risk Factors: Age 58, obesity, family history, unopposed estrogen use
- Diagnostic Considerations: No constitutional symptoms; biopsy required for definitive diagnosis
- Evidence-Based Reference: SGO guidelines state that endometrial thickness >4 mm in postmenopausal women with bleeding warrants further evaluation
- Cervical or Endometrial Polyp (ICD-10: N84.0/N84.1)
- Supporting Evidence: History of prior polyp (2018), intermittent bleeding pattern
- Risk Factors: Previous history of polyps
- Diagnostic Considerations: No visible polyp on speculum exam; further evaluation with saline infusion sonohysterography may be indicated
- Evidence-Based Reference: Up to 30% of postmenopausal bleeding cases are attributed to polyps (ACOG, 2018)
- Atrophic Vaginitis/Endometritis (ICD-10: N95.2)
- Supporting Evidence: Atrophic vaginal mucosa noted on exam, 7 years post-menopause
- Risk Factors: Postmenopausal status
- Diagnostic Considerations: Bleeding typically more spotty; atrophy alone unlikely to cause endometrial thickening
- Evidence-Based Reference: NAMS position statement (2020) notes that severe atrophy can cause abnormal bleeding but rarely with endometrial thickness >4 mm
- Exogenous Hormone Therapy Effect (ICD-10: Z79.890)
- Supporting Evidence: Current use of conjugated estrogens without progestin
- Risk Factors: Unopposed estrogen use for 2 years
- Diagnostic Considerations: ACOG recommends progestin for uterine protection in women with intact uterus
- Evidence-Based Reference: WHI study demonstrated increased risk of endometrial pathology with unopposed estrogen
Contributing Factors:
- Obesity (ICD-10: E66.9, BMI 32)
- Increases estrogen production in adipose tissue
- Associated with 2-4 fold increased risk of endometrial pathology
- Unopposed Estrogen Therapy (ICD-10: Z79.890)
- 2 years of conjugated estrogens without progestin
- Increases risk of endometrial hyperplasia and cancer
- Family History of Endometrial Cancer (ICD-10: Z80.0)
- First-degree relative (mother) with endometrial cancer
- Increases lifetime risk approximately 2-3 fold
- Hypertension (ICD-10: I10)
- Associated with increased risk of endometrial pathology
- Current reading 142/88 mmHg indicates suboptimal control
Risk Stratification:
- Endometrial Cancer Risk: Moderate to high based on multiple risk factors (family history, obesity, unopposed estrogen, endometrial thickness >4 mm)
- Urgent Evaluation Required: Yes, due to constellation of risk factors and abnormal imaging findings
Plan (P)
1. Diagnostic Interventions:
- Endometrial Biopsy:
- Schedule Pipelle endometrial biopsy within 48 hours
- Rationale: Gold standard for evaluating endometrial tissue in postmenopausal bleeding
- EBP Reference: ACOG Committee Opinion #734
- Saline Infusion Sonohysterography (SIS):
- If biopsy is non-diagnostic or incomplete
- Rationale: Better visualization of focal lesions (polyps, submucous fibroids)
- Pelvic MRI:
- Consider if biopsy is inconclusive or inadequate
- Rationale: Evaluates myometrial invasion if endometrial cancer is suspected
- Laboratory Follow-up:
- Review pending lab results (TSH, Free T4, Pap smear, HPV)
- Repeat CBC in 4 weeks if bleeding persists
2. Medications:
- Hormone Therapy Modification:
- Discontinue conjugated estrogens (Premarin) 0.625 mg daily immediately
- Rationale: Unopposed estrogen increases risk of endometrial pathology in women with intact uterus
- EBP Reference: NAMS 2017 Hormone Therapy Position Statement
- Alternative Osteoporosis Management:
- Initiate alendronate 70 mg oral weekly if the biopsy negative for malignancy
- Continue calcium/vitamin D supplementation
- Rationale: Non-hormonal management of osteoporosis
- Hypertension Management:
- Increase lisinopril to 20 mg daily
- Home BP monitoring twice daily
- Rationale: Current BP 142/88 mmHg is above target; AHA guidelines recommend <130/80 mmHg
3. Consultations/Referrals:
- Gynecologic Oncology:
- Expedited referral if endometrial biopsy shows atypia, hyperplasia, or malignancy
- Rationale: Family history of endometrial cancer increases risk profile
- Endocrinology:
- Referral for comprehensive osteoporosis management
- Rationale: Need for a non-hormonal approach given contraindications to HRT
- Registered Dietitian:
- Referral for medical nutrition therapy for weight management
- Rationale: BMI 32 contributes to endometrial cancer risk and hypertension
- Physical Therapy:
- Referral for weight-bearing exercise program for osteoporosis
- Rationale: Evidence supports exercise as adjunctive therapy for bone health
4. Patient Education:
- Bleeding Red Flags:
- Report immediately if bleeding becomes heavy (>1 pad/hour), associated with severe pain, or syncope
- Rationale: May indicate active hemorrhage requiring urgent intervention
- Medication Changes:
- Explained rationale for discontinuing HRT
- Provided written instructions for new medication regimen
- Lifestyle Modifications:
- Weight loss goal of 5-10% of current weight over 6 months
- Mediterranean diet pattern recommended
- Regular physical activity: aim for 150 minutes/week of moderate-intensity exercise
- Rationale: Evidence supports these measures for reducing endometrial cancer risk
- Follow-Up Instructions:
- Keep endometrial biopsy appointment
- Return to clinic in 2 weeks to review all results
- Maintain bleeding diary with pad count/saturation
5. Advanced Practice Considerations:
- Evidence-Based Practice Application:
- Following ACOG guidelines for postmenopausal bleeding evaluation
- Utilizing NAMS recommendations for hormone therapy management
- Applying AHA/ACC guidelines for hypertension management in high-risk patients
- Quality Improvement Opportunity:
- Consider office protocol development for expedited evaluation of postmenopausal bleeding
- Track time from presentation to endometrial sampling as a quality metric
- Interprofessional Collaboration:
- Communicate findings to the primary care provider
- Coordinate care between gynecology, endocrinology, and dietetics
- Case conference with gynecologic oncology if high-risk features identified
- Cultural Considerations:
- Assessed for any cultural barriers to following the recommended plan
- Provided educational materials in the patient’s preferred language
6. ICD-10 Coding:
- Primary Diagnosis: N95.0 (Postmenopausal bleeding)
- Secondary Diagnoses:
- I10 (Essential hypertension)
- M81.0 (Postmenopausal osteoporosis without current pathological fracture)
- E66.9 (Obesity, unspecified)
- Z79.890 (Hormone replacement therapy)
- Z80.0 (Family history of malignant neoplasm of digestive organs)
7. Patient Response and Understanding:
- Patient verbalized understanding of:
- Serious nature of postmenopausal bleeding
- Need for prompt endometrial biopsy
- The rationale for discontinuing HRT
- Warning signs requiring immediate attention
- Patient demonstrated teach-back of key points and agreed to follow-up plan
- Patient provided with after-hours contact information
References:
- American College of Obstetricians and Gynecologists. (2021). Practice Bulletin No. 149: Endometrial Cancer. Obstetrics & Gynecology, 137(3), e171-e190.
- The North American Menopause Society. (2020). The 2020 genitourinary syndrome of menopause position statement. Menopause, 27(9), 976-992.
- The American Cancer Society. (2022). Endometrial Cancer Risk Factors. Retrieved from: www.cancer.org
- Smith, R.L., et al. (2021). Accuracy of transvaginal ultrasonography for detecting endometrial abnormalities in postmenopausal women with vaginal bleeding. JAMA Internal Medicine, 181(5), 612-619.
- Whelton, P.K., et al. (2018). 2017 ACC/AHA/AAPA/ABC/ACPM/AGS/APhA/ASH/ASPC/NMA/PCNA Guideline for the Prevention, Detection, Evaluation, and Management of High Blood Pressure in Adults. Journal of the American College of Cardiology, 71(19), e127-e248.
Next Steps:
- Track biopsy results through the electronic health record
- Schedule interprofessional team huddle to review case findings
- Document in the registry for postmenopausal bleeding quality metrics
- Ensure closed-loop communication for all referrals

