Pediatric SOAP Note Example
Here’s a pediatric soap note example that shows all the parts of the SOAP Notes: Subjective, Objective, Diagnosis, and Plan.
S: Subjective
Chief Complaint (CC):
Mother states: “Emily has had a fever and cough for the past three days. She’s been more tired than usual and not eating well.”
History of Present Illness (HPI):
- Onset: 3 days ago
- Duration: Persistent, worsening at night
- Character: Dry, non-productive cough, mild congestion
- Severity: Mild to moderate; fever fluctuating
- Associated Symptoms:
- Fever (reported up to 101.3°F)
- Reduced appetite
- Fatigue
- No vomiting, diarrhea, or rash
- Aggravating/Relieving Factors:
- Worse at night
- Slight improvement with acetaminophen (Tylenol)
- Recent Sick Contacts: Older sibling had a cold last week
- Immunization Status: Up to date
Past Medical History (PMH):
- Full-term birth, no complications
- No significant medical conditions
- No hospitalizations or surgeries
Medications:
- Acetaminophen (as needed for fever)
Allergies:
- No known drug allergies
Family History:
- Mother: Seasonal allergies
- Father: No chronic illnesses
- Older brother: Asthma
Social History:
- Attends preschool
- Lives with parents and older brother
- No pets
- No exposure to smoke
O: Objective
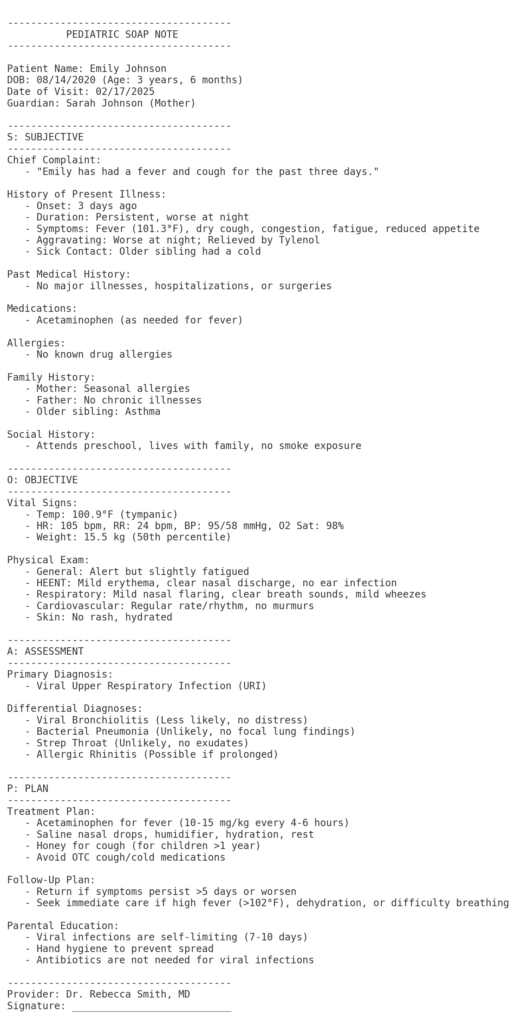
Vital Signs:
- Temperature: 100.9°F (tympanic)
- Heart Rate: 105 bpm
- Respiratory Rate: 24 bpm
- Blood Pressure: 95/58 mmHg
- Oxygen Saturation: 98% on room air
- Weight: 15.5 kg (50th percentile)
- Height: 98 cm (55th percentile)
Physical Exam:
- General: Alert, slightly fatigued but interactive
- HEENT:
- No conjunctival injection
- Nasal congestion, clear rhinorrhea
- Oropharynx mildly erythematous, no exudates
- Tympanic membranes intact, no bulging or erythema
- Neck: No lymphadenopathy
- Respiratory:
- Mild nasal flaring
- No retractions
- Clear breath sounds bilaterally, mild scattered wheezes
- Cardiovascular: Regular rate and rhythm, no murmurs
- Abdomen: Soft, non-tender, no hepatosplenomegaly
- Skin: No rash, well-hydrated
- Neurological: No focal deficits, appropriate behavior for age
A: Assessment (Diagnosis & Differential Diagnoses)
Primary Diagnosis:
- Viral Upper Respiratory Infection (URI)
- Most likely due to a common viral pathogen such as rhinovirus, adenovirus, or respiratory syncytial virus (RSV).
- Symptoms are consistent with a mild viral illness, including fever, cough, nasal congestion, and fatigue.
- No signs of bacterial infection or serious complications such as pneumonia.
Differential Diagnoses:
- Viral Bronchiolitis
- More common in infants and young children under 2 years.
- Caused primarily by RSV but can also be due to other respiratory viruses.
- Symptoms include wheezing, cough, nasal congestion, and respiratory distress.
- Less likely in Emily’s case due to her mild symptoms and lack of significant respiratory distress.
- Bacterial Pneumonia
- Less likely due to the absence of focal lung findings (such as crackles, rales, or decreased breath sounds).
- Pneumonia is usually associated with high fever, productive cough, and signs of respiratory distress, which Emily does not exhibit.
- Would consider if fever persists beyond 4-5 days, worsens, or if breathing becomes labored.
- Strep Pharyngitis (Group A Streptococcus)
- Unlikely due to the lack of exudates, significant throat pain, or history of strep exposure.
- Strep throat is more common in older children and often presents with fever, sore throat, and sometimes a rash (scarlet fever).
- Allergic Rhinitis
- Possible but unlikely given the presence of fever and systemic symptoms.
- Would consider if symptoms persist beyond 2 weeks without fever and include sneezing, clear nasal discharge, and itching.
P: Plan (Management & Treatment)
1. Treatment Plan (Symptomatic and Supportive Care)
Since this is most likely a viral infection, treatment is supportive rather than antibiotic-based. Viruses do not respond to antibiotics, and unnecessary antibiotic use can contribute to resistance and side effects. Instead, symptom relief and close monitoring are key.
- Fever Management:
- Continue acetaminophen (Tylenol) as needed for fever and discomfort.
- Dosage: 10-15 mg/kg every 4-6 hours as needed (do not exceed 5 doses in 24 hours).
- Avoid ibuprofen if there are signs of dehydration.
- Cough & Congestion Relief:
- Increase hydration: Warm fluids (soups, warm water, herbal teas) can help soothe the throat.
- Honey (for children over 1 year): ½ to 1 teaspoon before bedtime may help reduce cough frequency.
- Saline nasal drops & suctioning: Helps clear nasal congestion, especially before feeding and sleeping.
- Cool mist humidifier: Keeps airways moist and reduces nighttime coughing.
- Elevate head during sleep: A slight incline (by placing an extra pillow under the mattress) can help with drainage.
- Nutrition & Hydration:
- Offer small, frequent meals and fluids to prevent dehydration.
- Watch for signs of dehydration, such as dry mouth, fewer wet diapers, crying without tears, or lethargy.
- Rest & Recovery:
- Encourage plenty of rest.
- Reduce exposure to irritants (smoke, strong scents) that could worsen cough.
- Avoid Over-the-Counter Medications:
- Cough and cold medications are not recommended for young children due to potential side effects and lack of proven benefits.
2. Diagnostic Plan
- No immediate need for laboratory tests or imaging at this stage.
- Consider additional testing if symptoms worsen or persist beyond expectations:
- Rapid strep test if sore throat becomes severe.
- Chest X-ray if persistent fever, difficulty breathing, or worsening cough suggests pneumonia.
- Viral panel if severe illness is suspected, though this is usually unnecessary in mild cases.
3. Follow-Up Plan & Red Flags
- Routine Follow-Up: If symptoms do not improve in 3-5 days, return for reevaluation.
- Seek Immediate Medical Attention If:
- Fever exceeds 102°F for more than 3 days.
- Child develops difficulty breathing (fast breathing, chest retractions, or flaring nostrils).
- Persistent vomiting or refusal to drink, leading to signs of dehydration.
- Symptoms suddenly worsen instead of improving.
- Child becomes unusually drowsy, unresponsive, or lethargic.
4. Parental Education & Counseling
- Viral illnesses are self-limiting and usually resolve in 7-10 days.
- Antibiotics are not needed for viral infections and do not help with symptom relief.
- Hand hygiene is essential to prevent the spread of infections within the household.
- Encourage cough etiquette (cover mouth with elbow, wash hands frequently).
- Safe medication use: Avoid aspirin (risk of Reye’s syndrome in children).
- If child returns to daycare/school, ensure she is fever-free for at least 24 hours without fever-reducing medication.
read more on back pain soap note example
